FROM July 25th, 2024
As a Seed Global Health Board Member, I am proud to announce the 2030 Strategic Plan! Health workers save lives. Seed’s 2030 strategic plan is focused on health workers because people are the leading levers of change in a health system. Seed is committed — working hand-in-hand with partners, including the Wellbeing Foundation Africa — to build the health workforce of the future and advance the health workforce as a global priority. I look forward to continuing to support longtime friend and ally CEO Dr Vanessa Kerry, and the entire Seed Global Health team, on our path to 2030 as we strive to save lives — and our planet. Read the strategic plan here: https://seedglobalhealth.org/approach/2030-strategic-plan/
FROM June 15th, 2024
On Friday, I was pleased to receive Arjun Jain, UNHCR Nigeria Country Representative, and Nancy Aburi, Head, UNHCR Private Sector Partnerships Africa, in a UNHCR Country Delegation Courtesy Call to the Wellbeing Foundation Africa. In a key expansion of our longstanding disaster response and relief efforts, since 2021, the Wellbeing Foundation Africa Midwives and Nurses, in our Hope Away From Home Refugee and Displaced Families Program Support Partnership with UNHCR Nigeria, began providing our continuous weekly Mamacare360 antenatal, intrapartum and postnatal classes for women, mothers, their children and families at the Adagom Refugee Settlement, Ukende Refugee Settlement, and host communities in Cross River State, not only to keep people healthy, but also offer kindness, education and empowerment during a time of uncertainty. The skills and compassion of the WBFA midwives are critical in refugee and displacement situations, especially fostering inclusion, and hope away from home. Analysing the UNHCR Global Trends; Forced Displacement in 2023 Report, I commended UNHCR Nigeria’s efforts characterised by extensive inter-agency coordination and strategic partnerships to respond to 2,305,335 internally displaced persons in Bornu, Adamawa and Yobe States, North-East Nigeria, 1,092,196 in North-West and North Central Nigeria, 2,083,835 Nigerian returnees, 381,293 Nigerian refugees resistered in Cameroon, Chad and Niger, and 87,475 refugees and asylum seekers registered in Nigeria. As the lead agency for protection and Human Security and Risk Management under the United Nations Development Assistance Framework UNDAF, UNHCR collaborates with various United Nations bodies, focused on integrating refugee assistance programs into broader development strategies, benefiting both displaced and local communities. Additionally, UNHCR works closely with the Federal Ministry of Humanitarian Affairs, Disaster Management and Social Development, and the North East Development Commission to enhance humanitarian response capabilities.
FROM June 13th, 2024
#ForeverKings - On Tuesday 11th of June, I was delighted to be flanked by Dr Saraki II and Dr Saraki III, respectively my dear husband HE Abubakar Bukola Saraki MBBS CON and my darling daughter Dr Teniola Saraki MBBS, and to be accompanied by a Former Speaker, Kwara State House of Assembly, Right Honorable Razak Atunwa, and highly renowned Global Health Leader and Innovator, Bhavin Vaid, as I was honoured with the prestigious King’s Changemaker Award as part of the 2024 King’s College London Distinguished Alumni Awards. I am humbled to receive the King’s Changemaker Award, as this recognition highlights the power of using knowledge with purpose and celebrates my efforts in global development, particularly in maternal, newborn, and child health through the Wellbeing Foundation Africa, while also acknowledging my work in advancing the United Nations Sustainable Development Goals and championing health equity through active global and national policy and advocacy. Reflecting on my educational journey at King’s College London, attaining an LLM in International Economic Law, I truly appreciate the profound impact of my time at the institution on my career trajectory, as my experience at #KCL instilled in me a sense of responsibility to use my education to make a meaningful impact on society with an international perspective. King’s mission to drive positive and sustainable change in society, through its commitment to empowering interdisciplinary thinking, has been a guiding force. At the distinguished award ceremony which took place at The Great Hall, King’s Building, Strand Campus, hosted by King’s Vice-Chancellor & President, Professor Shitij Kapur with Former Award Winner David Stanley BEM (Music Mmus), 2001 acting as compere for the evening, I congratulated all the distinguished awardees, including Dr Victoria ‘Vickki’ Harmer, alongside whom I serve on the Global Breast Cancer Care Council. I extend my heartfelt appreciation to King’s College London for the honour bestowed upon me, thank you, King’s College London, for this incredible distinction. Let us continue to harness the power of education and use our wisdom for the greater good!
FROM June 11th, 2024
As Founder and President of the Wellbeing Foundation Africa, which completes our 19th year and enters our 20th year of continued Advocacy, Action and Impact, it is with great pleasure that I present to you the Toyin Saraki Global Office and Philanthropy 2023 Annual Report. DOWNLOAD [3d-flip-book mode="fullscreen" id="2500"][/3d-flip-book] A testament to our steadfast dedication to safeguarding global commitments and advancing the mission of WBFA through our global promise of enhancing community health and wellbeing across Nigeria and beyond, in harmony with the United Nations Sustainable Development Goals; this alignment remains resolute as we expand into another decade of impactful national and global advocacy, policy and frontline programmatic initiatives. The 2023 programmatic year heralded transformative milestones that highlighted the power of Personal, social, health and economic education Education centred frontline schools and HCF engagement implementations, community-led solutions, and solidarity in enhancing health and wellbeing for all and improving the quality of planetary life. My Global Office and Philanthropy remains firm in supporting the Wellbeing Foundation Africa's resolve to confront the gaps within health systems, build capacity in basic and comprehensive emergency obstetric levels of care, advanced obstetric surgical skills, and better equip healthcare workers, to counsel, support and confidently navigate their patients journeys, particularly within reproductive maternal, newborn, child and adolescent health and nutrition, maternal mental health, water and sanitation hygiene, as well as neonatal intensive care unit #NICU support for lactation and breastfeeding.
FROM June 10th, 2024
Last week, I was delighted to visit the Lagos University Teaching Hospital EmONC Centre of Excellence, and address our training participants, as the Liverpool School of Tropical Medicine’s EmOC&QoC Unit of LSTM Nigeria, our Wellbeing Foundation Africa Lead Partner in the Advanced Emergency Obstetrics and Newborn Care Competency-Based Curriculum for Resident Doctors in Obstetrics and Gynaecology program at the National Postgraduate Medical College of Nigeria, commenced and completed the second cohort of Advanced Obstetric and Surgical Skills training for National Postgraduate Medical College of Nigeria faculty examiners of resident doctors in Obstetrics and gynaecology. Launched in February 2024, this project is the latest milestone in our shared goal of deploying highly effective advanced level training to improve maternal and child healthcare outcomes across Nigeria, responding to Nigeria’s high maternal and neonatal mortality rates; as the 2023 United Nations report on Trends in Maternal Mortality from 2000-2020 revealed that nearly 28.5% of global maternal deaths happen in Nigeria, and further stated that a woman in Nigeria has a 1 in 19 lifetime risk of dying during pregnancy, childbirth, or postpartum. The advanced training course and equipment provided by the EmOC&QoC Unit of LSTM, supported by the Royal College of Obstetricians and Gynaecologists (Nigeria Liaison Group), trained this 2nd cohort 24 faculty-examiner doctors from across Nigeria including examiner-level members of the Medical Women’s Association of Nigeria and Armed Forces Medical Corps, delivered by 4 facilitators from Nigeria and 4 facilitators from the UK, whom I thanked as they proceed to start trainings in Abuja this week. This Global Health Workforce Programme Project Partnership is funded by the UK Department of Health and Social Care and managed by the Tropical Health and Education Trust and Ducit Blue Solutions, to achieve more resilient health systems and support progress toward Universal Health Coverage.
FROM June 9th, 2024
I am privileged to congratulate His Royal Majesty, Kabiyesi, Oba Abdulwasiu Omogbolahan Lawal, Abisogun II, The Oniru of Iru Land, Oba Abdulwasiu Gbolahan Lawal CON and his amiable Queen Olori Mariam Lawal, on his 4th Year Coronation Anniversary, Commemorative Prayers, and the Inauguration of the Iyaoba Muinat Abeni House edifice, within the environs of Iru Palace, which took place on 7th June, 2024. In traditional recognition of my duties as Princess Royal of Ojora Kingdom and Iganmu Lands, and as the Erelu Bobajiro of Iru Land Royal Cabinet, it is an enduring honour to join Royal Fathers, Kings, Princesses and Princes, titled Chiefs and Chieftesses, and the good people of Iru Kingdom in celebrating a remarkable leader whose reign has been marked by grace, wisdom, and a steadfast commitment to the progress of our people, as His Royal Majesty’s visionary leadership ushers in prosperity and development for Iru Land, reflecting his dedication to the wellbeing of our community. Kabiyesi, Oye A Mori, may your reign continue to be blessed with peace, and your legacy shine brightly for generations to come!
FROM June 3rd, 2024
As a Global Breast Cancer Care Council Member, I greatly appreciate the invitation to participate in the Advisory Board Meeting organised by Policy Wisdom and Astra Zeneca on the sidelines of the 2024 American Society of Clinical Oncology Cancer Annual Meeting, which I am currently virtually attending, as it takes place in Chicago, Illinois. ASCO24 is one of the world’s largest and most prestigious cancer research conferences, with over 40,000 oncology professionals, 200 professional sessions, and more than 5,000 abstracts, focused on the fight against cancer, funded through Conquer Cancer, the ASCO Foundation, a nonprofit organisation created in 1999 to seek dramatic advances in the diagnosis, prevention, treatment, and cure of all types of cancers. Building off of this momentum, the Advisory Board Meeting is bringing together a network of esteemed experts and stakeholders interested in breast cancer, with the aim to validate and refine the preliminary outline of the breast cancer care quality indicator framework. I am particularly pleased by the results coming out of ASCO, including the promising results from the clinical trials of the cancer drug Enhertu, as it stalled the growth of tumours by more than a year, significantly longer than standard chemotherapy did in women with the most common form of metastatic breast cancer. This incredibly encouraging news and data, if cleared by regulators, could shift the way physicians treat hormone receptor-positive, metastatic breast cancer, and create a new standard of care in which patients with breast tumours that express even the faintest amount of HER2 protein can benefit. With the goal of learning from and leveraging the research results presented at ASCO, I look forward to advancing efforts in combating breast cancer and improving healthcare outcomes for women in Nigeria and worldwide, fostering a future where every woman has access to the best possible care.
FROM June 1st, 2024
Yesterday, I was honoured to receive His Excellency Ambassador Isaac Keen Parashina, the High Commissioner of the Republic of Kenya to the Federal Republic of Nigeria, and his Diplomatic Delegation Courtesy Call, at the Wellbeing Foundation Africa Lagos Office. Our enriching dialogue on public administration, leadership, and diplomacy was particularly poignant as Kenyans commemorate Madaraka Day today, a celebration of Kenya’s attainment of internal self-rule from colonialism in 1963. A significant national holiday, Madaraka, a Swahili word for power, symbolises the relentless sacrifices made by selfless compatriots in the struggle for self-governance, and this day, enshrined in the 2010 Constitution of Kenya, is celebrated with vibrant festivities including music, dance, military parades, and culminates in the Presidential Speech, reminding citizens of the importance of self-determination and national pride. It was a pleasure sharing the importance of public service and governance, while highlighting the strong ties between our nations of Kenya and Nigeria, as we commit to further fostering deeper connections and working together on common goals, to enhance our collective efforts in public health, education, and sustainable development, ensuring a healthier future for both nations. Happy Madaraka Day!
FROM June 1st, 2024
On Wednesday evening, I was pleased to join the Wellbeing Africa Foundation Team in honouring our social impact partners Reckitt at their Stakeholders Dinner in Lagos. The event commemorated the visit of the Reckitt Global Leadership Team and Delegation, led by Global CEO Kris Licht, to Nigeria and highlighted the organisation’s longstanding and exceptional impact in our country. Highlighting the role WBFA-Dettol Nigeria Hygiene Quest Curricula and Programming continues to play in Reckitt’s role to drive access to health and hygiene knowledge and solutions, and the socio-economic benefits, it was wonderful to have the Governor of Lagos State, H.E. Babajide Olusola Sanwo-Olu jidesanwoolu presence at the dinner, solidifying Lagos States commitment to #WASH and health equity. I was also pleased to take part in presenting the Access to Water, Sanitation and Hygiene Accelerator Seed Funding, a partnership between Reckitt and Yunus Social Business, to support and scale early-stage social enterprises in Nigeria which are championing positive health outcomes, bringing people together and changing behaviours, to build long-term sustainable change towards a cleaner and healthier world. With 90% of our national population lacking the full range of access to clean water, sanitation, and hygiene in Nigeria, only 8% of Nigerians practising proper handwashing, and over 23% still practising open defecation, our frontline impact and on-the ground efforts continue, expanding reach and solutions, by harnessing the power of public-private partnerships to change the world for the better, and catalyse innovation to achieve the United Nations Sustainable Development Goals.
FROM May 31st, 2024
On Tuesday in Abuja, I was privileged, in my capacity as Founder of the Wellbeing Foundation Africa and Reckitt Social Impact Partner, to pay a formal courtesy call upon His Excellency The President, Asiwaju Bola Ahmed Tinubu GCFR at The Aso Rock Presidential Villa. Reckitt Benckiser, the Wellbeing Foundation Africa’s longstanding private sector partner and the global leader in trusted hygiene products has proudly invested in Nigeria for over 60 years, contributing significantly to the country’s development. The Reckitt Global Delegation, led by Chief Executive Officer, Mr Kris Licht, and the distinguished Chairman of Reckitt Benckiser Nigeria Limited, Chief Olu Falomo, was honoured with a warm welcome, recognition and insightful discussions with His Excellency Mr President, renewing our mutual long-term commitment to our vibrant nation, an important business destination for today and the future, as President Tinubu’s Administration emphasised their unwavering commitment to fostering a conducive environment for private sector investments based in sustainable economic growth. At the meeting, which had in attendance, Honourable Minister of Industry, Trade and Investment, Dr Doris Uzoka-Anite, Chief of Staff to the President of Nigeria, Honourable Femi Gbajabiamila, and Principal Secretary to the President of Nigeria, Hakeem Muri-Okunola, we also extended our congratulations to H.E. President Tinubu on the anniversary of his first year in office, sharing the vision of the Renewed Hope Agenda, which hinges on the core pillars of democracy, development, demographics, and diaspora engagement. The visit was an opportune moment to remind us that Nigeria stands ready to embrace the future, and position itself as a prime global investment destination.
FROM May 30th, 2024
This week we got the opportunity to visit the WHO Nigeria/West Africa HQ in Abuja, Nigeria where the Global Leadership team of Reckitt led by Kris Licht, Patricia O’Hayer met the Regional Head of WHO Dr Walter Kazadi Mulombo & his exceptional team alongwith Reckitt’s Social Impact partner the Well-being Foundation led by H.E. Toyin Saraki We got the opportunity to present our Social Impact report around WASH to the WHO Regional Team. WHO Nigeria is WHO’s 2nd biggest team deployed in one country in the world, after only to India. The role it plays is pivotal for not only Nigeria but for the global health. We are grateful for the partnership and we believe together Reckitt-WHO along with our social impact partner, Well-being Foundation, can make a humble difference in the area of Health & Hygiene to reduce the burden of disease in Nigeria.
FROM May 30th, 2024
As President and Founder of the Wellbeing Foundation Africa, I had the distinct pleasure of facilitating an on-the-ground visit for our global partners from Reckitt to Model Primary School in Maitama, Abuja, to assess our collaborative frontline impact and commitment to fostering health and hygiene among students through the WBFA-Nigeria Hygiene Quest programme. Our Phase 2 implementation is already demonstrating significant results, which recently began in February of this year and will continue until January 2026, having thus far reached over 45,000 students, 13,000 mothers, and 12,000 community members in a few short months. This early success is a testament to the power of partnership and our shared vision for a healthier and more hygienic future for all. During our visit, we were greeted by Head Teacher, Ms Hajiya Mario Hassan, who expressed her deep gratitude for the programme’s selection of their school, as the contributions made, including the renovation of the #WASH Station and the establishment of the Hygiene Quest Wash Club, are making significant impact, as students showcased their knowledge of proper hand hygiene practices through engaging activities facilitated by WBFA’s Nurse Educator, Mrs Jennifer Ighalo. Mr Kris Licht, Global CEO of Reckitt, commended the students for their enthusiastic participation and emphasised the importance of consistent use of handwashing stations, as I reflected on the recently commemorated Children’s Day, sharing the importance of handwashing with our younger generation, empowering them to be champions of change, reaffirming our commitment and efforts towards achieving the United Nations Sustainable Development Goals, and Clean Naija, with a joint goal to reach 6 million children in Nigeria by 2025.
FROM May 29th, 2024
This week in Nigeria, I am delighted to welcome, and honoured to host, the longstanding trusted Wellbeing Foundation Africa Programmatic, Advocacy and Policy Partners Reckitt Global Delegation in Nigeria led by Kris Licht, Global CEO, Patty O’ Hayer, Global Head of External Communications & Affairs, Hamzah Sarwar, Global Social Impact & Partnerships, Ranjay Radhakrishnan, Chief HR Officer, with Chief Olu Falomo, Chairman Reckitt Nigeria Limited, Akbar Ali Shah, General Manager, Reckitt Sub-Saharan Africa, Serra Bicak, Senior Vice President, Africa Middle East and Cassandra Uzo-Ogbugh, Head of External Comms & Partnerships, Reckitt Sub-Saharan Africa, at our initial welcome events, which held at the Transcorp Abuja. This in-country visit embodies Reckitt Benckiser’s commitment to building a cleaner, healthier Nigeria in joint belief with the Wellbeing Foundation Africa that access to high-quality hygiene, health and nutrition is a universal right. Driven by social impact as key to sustainability ambitions, Reckitt is harnessing the positive power of business to create meaningful and long-lasting change, investing in frontline community behavioural change and value-centred evidence-based learnings implemented by the Wellbeing Foundation Africa through the WBFA-Dettol Hygiene Quest programme and curricula, which is accelerating the uptake of long-lasting WASH habits in schools, healthcare facilities and communities across Nigeria. With a fruitful week ahead during this significant milestone visit, and looking forward to insightful discussions with national stakeholders on beneficial socio-economic impact programming, I was also pleased to introduce our honoured Wellbeing Foundation Africa Hygiene Quest partners to Mr Tony Elumelu, Chairman Tony Elumelu Foundation and Transcorp Group, Heirs Holdings, Uba Group Directors, while exploring new opportunities for collaboration towards Wellbeing For All to reinforce our mission to foster health initiatives, and showcasing the remarkable work we have been doing on the ground.
FROM May 29th, 2024
I had the honour of joining the Reckitt’s Global Delegation in Nigeria, esteemed partners of the Wellbeing Foundation Africa, as together, we paid a courtesy visit to the British High Commission Abuja, where we had the privilege of meeting with His Excellency Dr Richard Montgomery CMG, the British High Commissioner to the Federal Republic of Nigeria, and the UK Permanent Representative to the Economic Community of West African States. Reckitt Benckiser has a rich history rooted in Britain and in Nigeria. Founded in 1840 by Isaac Reckitt in Hull, England, Reckitt initially focused solely on household products, to make the world cleaner and healthier. Over the decades, Reckitt has grown into a leading multinational corporation based in innovation and achievement, renowned for its dedication to scientific breakthroughs, revolutionary products and research and development, as well as pioneering social and environmental programmes. With business as a force for good to engender cleaner, healthier lives, Reckitt’s commitment to wellbeing and quality has made it a household name in Nigeria for over 60 years, since it’s establishment in 1960, with significant contributions to the country’s health and hygiene sectors. Through initiatives such as the WBFA-Dettol Hygiene Quest Programme, aimed at improving public health, WASH behaviours and practices, and providing essential products with consumer insights, Reckitt has made a profound impact on Nigerian communities, embedded in its global mission to protect, heal, and nurture in the relentless pursuit of a hygienically improved and health-optimised world. In speaking with His Excellency Dr Richard Montgomery CMG, we delved into strengthening this bilateral relationship with private sector partners, as we work towards co-ordinating, promoting and protecting the joint interests of the United Kingdom and Nigeria, contributing to the enhancement of Nigeria’s socio-economic prosperity.
FROM May 24th, 2024
This #FrontlineFriday, I especially commend and appreciate the Liverpool School of Tropical Medicine’s EmOC&QoC Unit of LSTM Nigeria, our Lead Partner in the Advanced Emergency Obstetrics and Newborn Care Competency-Based Curriculum for Resident Doctors in Obstetrics and Gynaecology program at the National Postgraduate Medical College of Nigeria, as we commenced and completed the first cohort of Advanced Obstetric and Surgical Skills training for National Postgraduate Medical College of Nigeria faculty examiners of resident doctors in Obstetrics and Gynaecology at the Centre of Excellence, Lagos University Teaching Hospital, on 3rd to 7th May 2024. The training course and equipment provided through the EmOC&QoC Unit of LSTM, supported by the Royal College of Obstetricians and Gynaecologists (Nigeria Liaison Group), has now completed training the first cohort of 30 lead doctor faculty members from various hospitals across Nigeria, as trainers at the CoE in Lagos for continuity and sustainability, strengthening life-saving skills and interventions for care of pregnant women and their newborn babies. The training is key to improving maternal, newborn and child health outcomes by empowering medical professionals with advanced skills and knowledge, having significant influence on the development of obstetricians across Nigeria. This Global Health Workforce Programme #GHWP Project Partnership is funded by the UK Department of Health and Social Care and managed by the Tropical Health and Education Trust and Ducit Blue Solutions with the ambition of establishing two Centres of Excellence in Northern and Southern Nigeria where the training course will be delivered, to achieve more resilient health systems for post-pandemic recovery and support progress toward Universal Health Coverage #UHC, and for the benefit of the UK and partner country health sectors.
FROM May 20th, 2024
Last week, as a council member of the Astra Zeneca Global Breast Cancer Care Council, I joined our group of cancer advisory experts in clinical research, advocacy, and policy, in warmly welcoming the new Policy Report on Improving Breast Cancer Care in the Middle East and Africa by The Swedish Institute for Health Economics, co-authored by our council member Dr. Thomas Hofmarcher, and The Lancet Breast Cancer Commission Report The Lancet Group, co-authored by our council member Dr. Benjamin Anderson. Breast cancer is one of the biggest killers of women around the world and is growing in women of working age. World leaders do not adequately prioritise breast cancer, which also impacts economies and communities. Both reports highlight that to address this mounting burden, cross-sector cooperation with strategic direction and coordination to enhance breast cancer care, particularly in low-and middle-income countries is needed, especially as the WHO Global Breast Cancer Initiative endeavours to annually decrease the breast cancer mortality rate by 2.5%, potentially saving 2.5 million lives by 2040, through the pillars of detection, diagnosis, and treatment. As a member of the Global Breast Cancer Care Council, we know that every dollar invested in women’s health has a threefold return for economic growth, and we are concerned that even the world’s largest economies are not putting patients’ care higher on the list. The Council’s urgent ambition is to put the entire continuum of breast cancer care at the forefront of government priorities at the global, national, and local levels through purposeful and targeted policy reforms with the patient at the centre. The policy recommendations will define a clear path forward, aligned with key clinical guidelines and global frameworks and will champion patients and their families, caregivers, and other stakeholders to address disparities in breast cancer care to attain optimal patient outcomes across the globe.
FROM May 16th, 2024
On Saturday the 11th of May, I appreciated the kind invitation from H.E. Dr Ngozi Okonjo Iweala, Director General of the World Trade Organization, to the Women in Leadership Nigeria gathering, hosted in honour of a Special Guest, Meghan, The Duchess of Sussex, in Abuja. In my goodwill message, conveyed to Dr Okonjo-Iweala as I concluded my USA engagements, I extended my good wishes for productive dialogue at the Women in Leadership event celebrating female leaders in Nigeria, moderated by Mo Abudu, and the further beneficial endeavours that took place during the heart-warming Private Visit of Prince Harry and Meghan, The Duke and Duchess of Sussex, to Abuja and Lagos, Nigeria; with a particular focus on the activities to improve the wellbeing of injured military veterans with disabilities through the We Are Invictus Games and Nigeria: Unconquered collaboration, sports for youth societal development with Masai Ujiri, Giants Of Africa and the Archewell Foundation.
FROM May 15th, 2024
During my time at the Milken Institute Global Conference 2024 in Beverly Hills, I was delighted to reconnect with US based partners and allies in the global health community, as we delved into the theme "Shaping a Shared Future," and translated our shared lessons learned into the creation of meaningful, healthy, and prosperous lives for all. Meeting with Kevin Thurm, Chief Executive Officer of the Clinton Foundation, I lauded President Clinton’s lifetime of public service on HIV equity, his belief that everyone deserves a chance to succeed, has a responsibility to act, and does better when we work together. Energised by these values, I shared the impact of The Wellbeing Foundation Africa in expanding economic opportunity, improving public health and education, confronting the climate crisis, and inspiring citizen engagement and service, especially for women. Shortly thereafter, I connected with Dr. Neil Buddy Shah, Chief Executive Officer of The Clinton Health Access Initiative, reflecting on our mutual historical commitments to the Saving One Million Lives Initiative Nigeria, as we continue to progress the Wellbeing Foundation Africa and The Clinton Health Access Initiative allyship to improve health outcomes and demographic trajectories in low-and middle-income countries by enabling the government and private sector to strengthen and sustain quality health and wellbeing systems. To end the day, we all joined together, motivated by multi-sectoral partnerships to make strides toward a world where our combined efforts yield transformative results, as we listened to Mike Milken, Chairman of the Milken Institute, in conversation with President Bill Clinton, the 42nd President of the United States, discuss their successful initiatives in medical research, education, public health and access to capital, as two visionaries reimagining the future for our grandchildren, and generations to come.
FROM May 13th, 2024
During the recent Milken Institute Philanthropic Investors Forum held in Beverly Hills, I was specifically asked to elucidate upon my personal experience of childbirth in 1991, and its subsequent impact on my approach to knowledge acquisition, learning, and development in challenging, overcoming and rising positively from the adversity of birth trauma, which for me, had occurred in a low and middle income country, my home nation of Nigeria. Throughout the conversation, I delved into the discovery of the maternal health trajectory and the alarming statistics regarding preventable maternal and newborn mortality, which I continuously encountered and recorded through a first-hand civil registrations and vital statistics approach across Nigeria’s public health system, during my tenure as the First Lady of Kwara State in 2003, and how through this confluence of experiences, I was ultimately inspired to establish the Wellbeing Foundation Africa which has worked to constructively empower and engender safer births and safe motherhood since 2004. Later last week, which commenced the annual celebration of International Day of the Midwife on the 5th of May and looked to celebrating the annual International Nurses Day on the 12th of May, it was during the Baby Blues: The Early Days of the Motherhood Journey Roundtable Conversation at the Milken Institute Global Conference 2024, that I reflected on how the early days of motherhood are often painted with the great and good expectations of rosy hues, but in reality, and increasingly recorded around the world, the antenatal, perinatal and postpartum period can involve significant identity transformation, physical and emotional challenges, and even birth injuries, that persist far into the first year and 1000 days. Postpartum depression affects nearly one in five new mothers, often leading many to endure physical and emotional burdens for up to a year after childbirth. Consequently, roughly 43% of highly skilled women leave their careers either temporarily or permanently after giving birth, hampering economic productivity and labour markets as well. The Early Days of the Motherhood Journey Roundtable Conversation Session delved beyond the "baby blues," uncovering postpartum realities from physical recovery to mental health struggles and workforce impact. Having long championed the skills, capacities, and competencies of midwives and nurses as Emeritus Global Goodwill Ambassador to the International Confederation of Midwives (ICM), and as a supporter of the Nursing Now Challenge, which advocates for leadership development opportunities for student and early career nurses and midwives around the world, I was immediately propelled into asking why there were no professional midwives or nurses at the colloquium table: as the gathering fielded questions and answers, hearing from mothers, healthcare professionals, doulas, advocates, and investors, who addressed resource shortcomings, investment prospects, and strategies for enhancing maternal support during this pivotal period to create a future where mothers are truly seen, heard, empowered, and invested in the way they should be. Having worked in Nigeria, and with many global efforts, such as the Every Woman Every Child #EWEC movement to intensify national and international commitment and action by governments, the UN, multilaterals, private sector and civil society to keep women's, children's and adolescents' health and wellbeing at the heart of development, Nigeria’s first and oldest country member of the esteemed and dedicated Partnership for Maternal Newborn and Child Health, and currently a PMNCH MNCH Workstream Working Group Member, for over 20 years towards safe motherhood, I am particularly alarmed and appalled by the rising data which finds that Black women are five times, and Asian women two times, more likely to die in the perinatal period than white women. Described in 2022 as an ‘urgent human rights issue and urgent action must be taken to address it’ (Birthrights, 2022), this annual report continues to show no positive change to the health outcomes of BAME (Black, Asian and minority ethnic) women. Within the UK, the All-Party Parliamentary Group #APPG on Birth Trauma has this year in January 2024, established the first national inquiry in the UK Parliament to investigate the reasons for birth trauma and to develop policy recommendations to reduce the rate of birth trauma. Today, the inquiry into traumatic childbirths has been released, and calls for an overhaul of the UK's maternity and postnatal care after finding poor care is "all-too-frequently tolerated as normal." With harrowing evidence from more than 1,300 women - some said they were left in blood-soaked sheets while others said their children had suffered life-changing injuries due to medical negligence, women complained they were not listened to when they felt something was wrong, were mocked or shouted at and denied basic needs such as pain relief. A pivotal recommendation is to engage a new maternity commissioner who would report directly to the prime minister, along with ensuring safe levels of healthcare staffing. It has been proven that BAME women report positive experiences when in receipt of woman‐centred midwifery care, and at the Wellbeing Foundation Africa, an element of the role of the WBFA midwife is to be an advocate for the women in our care, as midwives have a long and proud tradition of providing care that addresses health inequalities. I recall advocating and exemplifying the need for midwives for the most vulnerable populations through the Midwives Service Scheme established by the Nigerian federal government in 2009 until 2015 to address the scarcity of skilled health workers in rural communities by temporarily redistributing newly qualified, unemployed and retired midwives from urban communities to rural primary healthcare centres #PHCs to ensure improved access to skilled care. The scheme was designed as a collaboration among federal, state and local governments, yet the inability of the federal government to substantially influence the health care agenda of sub-national governments was a significant impediment to the achievement of the objectives of the Midwives Service Scheme, as the issues in retention, availability and training of midwives, and varying levels of commitment from state and local governments across the country, alongside women still choosing to deliver at home despite the availability of skilled birth attendants at MSS facilities, led to a lack of community and facility collaboration within the health sector, but provides many learnings we can take ahead in our journey to achieving the United Nations Sustainable Development Goals. The WBFA Mamacare360 Antenatal and Postnatal Education Classes, led as an Independent Maternity Program of Community Midwifery, are key patient advocates with regular and on-demand engagement for the central 1001 days of antenatal and postnatal care, while providing the full continuum of care through to child-centred personal, social, health and economic education and water, sanitation and hygiene practices at school age and beyond. Twenty years onwards since establishment, the Wellbeing Foundation Africa provides and delivers a lifesaving and quality improving panacea of programming for mothers and newborns across Nigeria, and while the challenges and solutions surrounding MNCH continue to evolve, certain foundational elements persist as revolutionary to this paradigm, including the imperative of respectful maternity care fostered by more midwives and nurses, which encompasses a holistic approach within specialised programmatic frontline solutions, such as Emergency Obstetric and Neonatal Care (EmONC) training for medical providers and midwives; a package of care for mothers and neonates when severe life-threatening complications occur during pregnancy, child delivery, and postpartum, believed to avert three-fourths of maternal mortality, the encouragement and uptake in breastfeeding in the Neonatal Intensive Care Units through lactation support programs, mental health safe spaces and services established by midwives and nurses, and a full spectrum of interventions designed to mitigate risks, provide timely interventions, and foster optimal health and wellbeing outcomes for both mothers and newborns. A fundamental question continues to persist in all of these cases: when to seek medical assistance. This question underscores the critical need for robust birth preparedness education, ensuring that expectant mothers are equipped with the knowledge and resources necessary to make informed decisions regarding their health and that of their newborns, as partners in their own care journey, led by quality trained midwives and nurses. Looking ahead, the continued development of maternal and newborn care demands a multifaceted approach at a global scale, for full maternity care overhaul and reform. This includes the expansion of resources such as midwifery and nursing personnel, as according to the UNFPA State of the World’s Midwifery Report, midwives can meet about 90% of the need for essential sexual, reproductive, maternal, newborn and adolescent health interventions, yet there is a global shortage of 1.1 million SRH and MCA healthcare providers, with 900,000 being midwives. With less than 2 Midwives Per 1000 People in Nigeria, 4 Midwives per 1000 People in the United States, and 9 Midwives per 1000 in the United Kingdom as according to the World Bank, and with global recommendation of 1 Midwife per 26 to 34 births, we must recruit, remunerate, regulate, replenish and resource midwifery and nursing services through upskilling and training - a universal requirement in improving and increasing the availability and quality of maternity care, counsel and support. Alongside this, increased attention to Integrated Maternal Newborn Child Health strategies, whose original consultations began in Nigeria at my request in 2007, to bolster and fortify the foundation upon which all MNCH trajectories are built are required, advancing the global health community towards a future where every mother and newborn receives the care and support they deserve.
FROM May 9th, 2024
Milken Institute Global Conference 2024: Philanthropic Investors Forum I deeply appreciate the honour of the Wellbeing Foundation Africa’s vision and mission being featured at the Milken Institute Philanthropic Investors Forum Opening Plenary Perspective, as we enter our 20th year of focused impact through improving health system strengthening, workforce capacities and personal social health, education and economic determinants for every woman, every child, every family, and communities to thrive, from safe motherhood, childhood, through to the life course of senior age. In the “Philanthropists Journey To Transformative Change” colloquium moderated by Melissa Stevens, Executive Vice President, MI Philanthropy, Milken Institute, I joined Jeffrey Katzenberg, Former Chairman, Walt Disney Studio, Founding Partner, WndrCo on the stage, as we highlighted the transformative moments that shaped our respective philanthropic endeavours setting the path to being more visionary strategic donors. From the initial spark of inspiration to action that defined our giving and programmatic approaches, we offered our unique perspectives on the challenges (and joys) we encountered along the way, to the impact we continue to seek and activate in the giving environment we consistently actuate. It was lovely to meet the hugely inspirational range of participating philanthropic leaders including Nigerian-Kenyan Masai Ujiri, Vice Chairman and President, Toronto Raptors, Founder, Giants of Africa and the Zaria group, as I explored the insights offered at the Philanthropic Investors Forum plenaries and breakout sessions focused on People: The Impact of Philanthropy to Better Lives and Livelihoods, Paradigms: Exploring Innovations in Philanthropic Giving, Place: Exploring the Role and Power of Place-Based Giving, and the closing thoughts of future considerations of Prospective: What’s Next for Corporate Foundations.
FROM May 5th, 2024
Sustainable Midwifery: Caring for Tomorrow’s World
On the 32nd International Day of the Midwife, I am truly honoured to join highly esteemed Professor Jacqueline Dunkley-Bent, Ibu Robin Lim, and Ginger Garcia, in delivering keynote addresses to the Virtual International Day of the Midwife, a 24-hour Conference focusing on midwifery as a vital solution in adapting health systems to com bat climate change, as midwives and their practice deliver safe and environmentally sustainable health services and are first responders when climate disasters hit.
The Wellbeing Foundation Africa Midwives promote and advocate the standards and frameworks of the International Confederation of Midwives in our mission as continuous providers of safe, quality and ecologically sound health and wellbeing services, especially in the face of the climate crisis, which carries specific threats for women and girls, as hotter temperatures can lead to pregnancy complications and worsen maternal-health issues including premature births.
Midwives are instrumental in ensuring that health services are more mobile and can urgently reach women, yet a global shortage of nearly one million midwives and a lack of international commitment to invest limits their capacity, while further reinforcing the latest data that every two minutes a woman or girl dies during pregnancy, childbirth or its aftermath.
By replenishing and ramping up investing in midwifery education, training and services, and scaling midwifery-delivered care, we aim to contribute to saving 4.3M women and newborns annually by 2035, and to the Global Midwifery Acceleration Roadmap, jointly developed by UNFPA, UNICEF, World Health Organisation and International Confederation of Midwives and global partners, to be launched at the World Health Summit.
Midwives are the providers of culturally sensitive health care, as leaders in their communities, and emergency responders, representing the single-most effective way to achieve safe motherhood and avoid preventable maternal deaths. Today I celebrate the courage and value of midwives globally, and wish everyone a Happy International Day of Midwives 2024!
bat climate change, as midwives and their practice deliver safe and environmentally sustainable health services and are first responders when climate disasters hit.
The Wellbeing Foundation Africa Midwives promote and advocate the standards and frameworks of the International Confederation of Midwives in our mission as continuous providers of safe, quality and ecologically sound health and wellbeing services, especially in the face of the climate crisis, which carries specific threats for women and girls, as hotter temperatures can lead to pregnancy complications and worsen maternal-health issues including premature births.
Midwives are instrumental in ensuring that health services are more mobile and can urgently reach women, yet a global shortage of nearly one million midwives and a lack of international commitment to invest limits their capacity, while further reinforcing the latest data that every two minutes a woman or girl dies during pregnancy, childbirth or its aftermath.
By replenishing and ramping up investing in midwifery education, training and services, and scaling midwifery-delivered care, we aim to contribute to saving 4.3M women and newborns annually by 2035, and to the Global Midwifery Acceleration Roadmap, jointly developed by UNFPA, UNICEF, World Health Organisation and International Confederation of Midwives and global partners, to be launched at the World Health Summit.
Midwives are the providers of culturally sensitive health care, as leaders in their communities, and emergency responders, representing the single-most effective way to achieve safe motherhood and avoid preventable maternal deaths. Today I celebrate the courage and value of midwives globally, and wish everyone a Happy International Day of Midwives 2024!
View this post on Instagram
FROM May 1st, 2024
It is wonderful to wish everyone a happy International Worker's Day and a great new month as I support an exciting new workstream initiative, Unifying Midwifery In Africa: Reimagine, Reignite, Rise! It was my pleasure to virtually provide the opening goodwill remarks to the Summit on Unifying Midwifery in Africa for the African Mother, Child and Adolescent, convened in Accra, Ghana, by a 12-member Steering Committee co-chaired by Centre for Health Development and Research-CEHDAR, bringing together colleagues from over 29 African countries, the USA and the Caribbean, including the Nigeria delegation led by the Wellbeing Foundation Africa, to empower African Midwives. The recent State of the World’s Midwifery Report has established that when midwives are educated to international standards, and midwifery includes the provision of family planning, it could avert more than 80% of all maternal deaths, stillbirths and neonatal deaths. Achieving this impact also requires midwives to be licensed, regulated, fully integrated into health systems, and working in interprofessional teams. When midwives are equipped with the necessary education, resources, and support, they have the power to achieve global, regional, and national Reproductive maternal, newborn, child and adolescent health goals. Together, midwives and allies will seek to employ a human-centred consultative process to deliberate and align around key issues influencing midwifery professional development in Africa and the potential impact of a continental coordinating body, while providing an avenue for African midwife leaders and stakeholders to recommend a roadmap and strategic actions for determining the way forward in uniting midwifery in Africa towards improving outcomes for mothers and families. I was honoured to deliver my expertise, experience and passion for midwifery, as the Wellbeing Foundation Africa represents our Nigerian collective, and defines the strategic directions to mobilise African midwives in culturally adapting the global health agenda to align with regional and national-level evidence-based interventions and promote the African maternal, newborn, child and adolescent health agenda for 2030 and beyond.
FROM April 26th, 2024
I was delighted to receive a special invitation and participate in the Unveiling of "The Godmothers; Mentorship Series," a joint initiative of the Gender Strategy Advancement International and She Forum Africa, alongside eminent multi-sectoral women leaders such as Dr Amina Aminu Dorayi, Ene Obi, Former Senator Biodun Olujimi, and Dr Peju Adenusi, and upcoming young women, introduced to nurture co-leadership skills and strengthen emerging voices that can further shape the narrative around women's inclusion, particularly, in the build-up to the next election cycle. Inspired by the vision of consciously and intentionally establishing safe learning and sharing space to build intergenerational trust and foster co-leadership, this refreshing platform envisages inspiring accountability and self-leadership for women now and women of the future. I was pleased to support and share my experiences in building more women's confidence to enter the political space as a result of safe spaces which empower and engender regardless of background or political affiliations. By capturing critical conversations and enabling them to evolve as community-owned, community-driven activations of emerging voices, I applaud the inaugural meeting, and congratulate my dear and very senior mentee Inimfon Etuk, her co-creator Adaora, and the entire She Forum Africa and Gender Strategy Advancement International team!
FROM April 25th, 2024
Yesterday in Abuja, as Nigeria and Africa Member of the International Steering Council for the International Conference on Population and Development ICPD25 and ICPD30, and as a Friend of UNFPA, I welcomed my dear colleague, sister and friend, Dr Natalia Kanem, Executive Director of UNFPA and United Nations Under-Secretary-General, once again to Nigeria as we marked a major milestone, in launching the 2024 State of the World Population #SWOP Report, Interwoven Lives, Threads of Hope, Ending Inequalities in Sexual and Reproductive Health and Rights. Coming together to weave a path forward, and ensure that the next 30 years of progress includes everyone, the report highlight that while progress has been made, it is not being done so fast enough, nor far-reaching enough. Gender-based violence remains rampant in nearly every country and community, and there has been zero reduction in maternal mortality since 2016 globally, with the current lifetime risk of a Nigerian woman dying during pregnancy, childbirth, postpartum or post-abortion care about 1 in 22, and many African women still unable to exercise decisions on their health, an imperative human right. As a core frontline community stakeholder committed to achieving the ICPD Programme of Action, the Wellbeing Foundation Africa is committed to; zero unmet needs for family planning and services, zero preventable maternal and infant deaths, zero sexual and gender-based violence including early and forced marriage, as well as ending female genital mutilation, through advocating for and implementing programming which emphasises the importance of keeping girls in school, prioritises family planning, reduces inequality in health access, works towards combating HIV/AIDS, and fosters wellbeing spaces which are lowering maternal and infant mortality rates globally. Our vision for the future must be a future for all, and as it gains momentum, in which strengthening the rights and welfare of individuals reinforces those of the collective, I commend and congratulate key leaders, Honourable Nasir Isa Kwarra, Chairman, National Population Commission Nigeria, United Nations Resident and Humanitarian Coordinator represented by the Country Representative UNICEF Nigeria, Ms Christian Munduate, H.E. Professor Muhammad Ali Pate CON, in his capacity as Coordinating Minister of Health and Social Welfare and representing Their Excellencies the President Bola Ahmed Tinubu GCFR and the Vice President, Senator Kashim Shettima CON respectively, Chairman, Senate Committee on Population, Senator Mustapha Musa, His Royal Highness the Emir of Shonga, Royal Fathers and Traditional Rulers Development Partners, H.E. Richard Montgomery the British High Commissioner, H.E. Jamie Christoff, Canadian High Commissioner in Nigeria, all members of the Diplomatic Community, and Friends of UNFPA, for their solidarity at this pivotal point in history towards faster progress in ending marginalization and discrimination.
FROM April 24th, 2024
Last Friday, I was delighted to provide a virtual Goodwill Message to the Women in Healthcare Forum, taking place in collaboration with the Women in Healthcare Network during the Medic West Africa Conference in Lagos on #FrontlineFriday. Under the theme “POW(H)ER CONNECT: Building Bridges, Breaking Barriers,” the mutual mission to connect, inform, and inspire women in the healthcare industry is vital, providing a platform for networking, mentorship, education, and advocacy, empowering women to reach their full potential and break down barriers within the field. Women make up 70% of the global health and social workforce, providing essential health services for around 5 billion people worldwide, and according to The Lancet, in Nigeria nearly all midwives, 87% of nursing personnel, and 65% of medical doctors are women, yet women’s contributions to health and the health labour market remain markedly undervalued, and they are vastly underrepresented in senior health leadership positions. Women in health tend to be clustered into lower status, low paid, and often unpaid roles. The healthcare development agenda in Nigeria and across Africa must better value women’s contributions to the population’s physical, social and mental wellbeing. Alongside this, equity issues pertaining to decent work free from all forms of discrimination is necessary for all United Nations member states to address if the 15 million health worker shortfall to achieve Universal Health Care is to be redressed in an inclusive and sustainable way. Where Women Lead in Health, Transformation Tends to Follow; I extend a heartfelt congratulations to Dr. Dupe Elebute-Odunsi and all the founding members of the Women in Healthcare Network Nigeria for their dedication, vision, and unwavering commitment to engendering women in the healthcare sector. I wish you all a Happy NewWeek, may it be filled with productivity and meaningful connections for impact! WATCH THE SPEECH
FROM April 24th, 2024
 As I virtually round up my observation of the 2024 Spring Meetings of the World Bank Group and the International Monetary Fund taking place this week in Washington DC, I am honoured to be invited to contribute to the Women Political Leaders breakfast conversation titled “Her Health, Our Priority: A Demand for Equity”, supported by Bayer, in the context of the spring meetings.
Women’s health remains a global imperative, and despite significant progress in recent decades, gender disparities and inequalities persist, affecting access to healthcare services, research funding, and leadership representation. The conversation, ‘Her Health, Our Priority: A Demand for Equity’ seeks to address these imbalances and ensure fair, equitable access to healthcare for all women and girls.
Good health is a key aspect of wellbeing and a fundamental human right, and the World Bank’s Science of Delivery investigates on how to create the right incentives for high-quality healthcare service delivery throughout #LMICs as poor health places high costs on individuals, households, firms, and governments.
The Wellbeing Foundation Africa recognises that long term improvements in personal, social, health and economic education, alongside enterprise and employment opportunities, have a positive impact on the health of women and girls, and that of their families and communities. Through strengthening and expanding essential health services for women, including nutrition and wellbeing, improving policies, and promoting more positive attitudes and behaviour towards girls education and women’s health, The Wellbeing Foundation Africa designs and implements programmes which address the constraints to women’s access to care, while ensuring women are empowered.
As I virtually round up my observation of the 2024 Spring Meetings of the World Bank Group and the International Monetary Fund taking place this week in Washington DC, I am honoured to be invited to contribute to the Women Political Leaders breakfast conversation titled “Her Health, Our Priority: A Demand for Equity”, supported by Bayer, in the context of the spring meetings.
Women’s health remains a global imperative, and despite significant progress in recent decades, gender disparities and inequalities persist, affecting access to healthcare services, research funding, and leadership representation. The conversation, ‘Her Health, Our Priority: A Demand for Equity’ seeks to address these imbalances and ensure fair, equitable access to healthcare for all women and girls.
Good health is a key aspect of wellbeing and a fundamental human right, and the World Bank’s Science of Delivery investigates on how to create the right incentives for high-quality healthcare service delivery throughout #LMICs as poor health places high costs on individuals, households, firms, and governments.
The Wellbeing Foundation Africa recognises that long term improvements in personal, social, health and economic education, alongside enterprise and employment opportunities, have a positive impact on the health of women and girls, and that of their families and communities. Through strengthening and expanding essential health services for women, including nutrition and wellbeing, improving policies, and promoting more positive attitudes and behaviour towards girls education and women’s health, The Wellbeing Foundation Africa designs and implements programmes which address the constraints to women’s access to care, while ensuring women are empowered.



 Welcoming the first ever Health Day at #COP28, discussing Heat & Health with the Bayer AG Team in the ICC Pavilion, Blue Zone; continuing co-creation collaborations established with multi-sectoral leaders, as we contribute to the #WBG goal to support countries in delivering quality and affordable health services to 1.5 billion people by 2030.
Welcoming the first ever Health Day at #COP28, discussing Heat & Health with the Bayer AG Team in the ICC Pavilion, Blue Zone; continuing co-creation collaborations established with multi-sectoral leaders, as we contribute to the #WBG goal to support countries in delivering quality and affordable health services to 1.5 billion people by 2030.
FROM April 16th, 2024
On the 10-year mark of the Chibok abductions this week, as 90 girls remain in captivity, and the country recovers from another abduction of schoolchildren in Kaduna State in March of this year, I support the UNICEF action plan to secure children's education in Nigeria, as the new report released states that just 37% of schools across 10 states have early warning systems in place to identify threats, such as school attacks, while calling for government accountability, and renewed commitment to rehabilitation efforts for survivors.
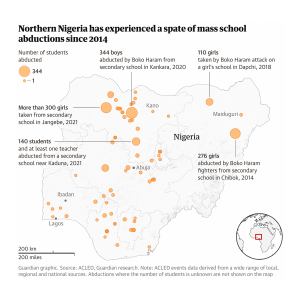 With child abductions becoming increasingly frequent in the last 10 years, with conflict-related violence leading to more than 1,680 children abducted while at school and else
where; 180 children killed due to attacks on schools; an estimated 60 school staff kidnapped and 14 killed; and more than 70 attacks on schools, according to verified reports by the United Nations, and given the alarming statistics in the ‘Minimum Standards for Safe Schools (MSSS) Monitoring Report,’ it is evident that our efforts to safeguard our children's futures in Nigeria must be amplified, addressing not only the symptoms but also the root causes of this crisis.
Despite initial assurances, the ongoing captivity of some of the Chibok girls serves as a stark reminder of the need for greater accountability and action of political will to ensure all schools across all states have the resources and tools to fully implement the #MSSS, focusing on the most vulnerable regions to close the critical gaps in safe school infrastructure, strengthen law enforcement and security measures to protect educational institutions and communities from attacks and abductions, prioritise education and child protection in national policies and budget allocations to create a safer, more inclusive environment for all Nigerian children, and ensure the continuity of education and learning when schools are shut through multiple learning pathways such as digital platforms.
The lack of tangible domestic intelligence, knowledge sharing and learning, transparency and deterrent measures to effectively address the scourge of abductions, despite the Safe Schools Initiative, is deeply disheartening and underscores the urgent need for greater accountability and measurable justice. I will continue to insist that the establishment of a register of victims of forced disappearance is imperative at the global, regional, and national levels, for governments to fulfil their obligations under international law, uphold human rights standards, and demonstrate their commitment to combating impunity.
Furthermore, comprehensive rehabilitation must be at the forefront as we strive to support survivors in rebuilding their lives, including programs which address the physical, emotional, and psychological needs to ensure long-term recovery and wellbeing, alongside concrete steps to tackle the insecurity and militancy in the region.
Education is a fundamental right and a crucial pathway in achieving peace and prosperity, yet for too many Nigerian children, it remains unsafe and unattainable. As we analyse and assess the past 10 years, we must pledge to protect children and promote the recovery of those who suffer abuses, and call on the federal government, including the military, to ensure the prosecution of those who have overseen the widespread abduction, torture and murder of children and girls, while highlighting the need to invest more substantially in education and take concrete steps to reduce the barriers that deny many children access to school.
With child abductions becoming increasingly frequent in the last 10 years, with conflict-related violence leading to more than 1,680 children abducted while at school and else
where; 180 children killed due to attacks on schools; an estimated 60 school staff kidnapped and 14 killed; and more than 70 attacks on schools, according to verified reports by the United Nations, and given the alarming statistics in the ‘Minimum Standards for Safe Schools (MSSS) Monitoring Report,’ it is evident that our efforts to safeguard our children's futures in Nigeria must be amplified, addressing not only the symptoms but also the root causes of this crisis.
Despite initial assurances, the ongoing captivity of some of the Chibok girls serves as a stark reminder of the need for greater accountability and action of political will to ensure all schools across all states have the resources and tools to fully implement the #MSSS, focusing on the most vulnerable regions to close the critical gaps in safe school infrastructure, strengthen law enforcement and security measures to protect educational institutions and communities from attacks and abductions, prioritise education and child protection in national policies and budget allocations to create a safer, more inclusive environment for all Nigerian children, and ensure the continuity of education and learning when schools are shut through multiple learning pathways such as digital platforms.
The lack of tangible domestic intelligence, knowledge sharing and learning, transparency and deterrent measures to effectively address the scourge of abductions, despite the Safe Schools Initiative, is deeply disheartening and underscores the urgent need for greater accountability and measurable justice. I will continue to insist that the establishment of a register of victims of forced disappearance is imperative at the global, regional, and national levels, for governments to fulfil their obligations under international law, uphold human rights standards, and demonstrate their commitment to combating impunity.
Furthermore, comprehensive rehabilitation must be at the forefront as we strive to support survivors in rebuilding their lives, including programs which address the physical, emotional, and psychological needs to ensure long-term recovery and wellbeing, alongside concrete steps to tackle the insecurity and militancy in the region.
Education is a fundamental right and a crucial pathway in achieving peace and prosperity, yet for too many Nigerian children, it remains unsafe and unattainable. As we analyse and assess the past 10 years, we must pledge to protect children and promote the recovery of those who suffer abuses, and call on the federal government, including the military, to ensure the prosecution of those who have overseen the widespread abduction, torture and murder of children and girls, while highlighting the need to invest more substantially in education and take concrete steps to reduce the barriers that deny many children access to school.
FROM March 22nd, 2024
This World Water Day, I am delighted to highlight the progress we have made in activating the Wellbeing Foundation Africa UN Water Conference commitments, actioning the critical importance of safe drinking water, sanitation and hygiene as fundamental human rights for dignity, stability and good health, while advocating for the sustainable management of freshwater resources, to address the global water crisis, in support of the United Nations Sustainable Development Goal 6: Water and Sanitation for All by 2030.
The World Health Organization states that 50% of healthcare facilities worldwide lack basic hygiene, while approximately 32% of healthcare facilities in Africa do not have access to hand hygiene facilities at the points of care. The joint report from UNICEF and WHO reveals that 839 million individuals and 38% of schools continue to lack essential hygiene facilities across the continent. In urban regions, 50% of the population lacks access to these services, compared to 70% in rural areas, highlighting significant disparities. Water scarcity and contamination pose significant challenges to communities around Africa and the globe and repercussions of this crisis are dire, affecting health, education, livelihoods, and overall socio-economic development.
 As featured in The Reckitt Social Impact Investment Report 2023, to address these statistics, and improve outcomes, the Wellbeing Foundation Africa and Dettol Nigeria Hygiene Quest Programme, generously supported by the partnership with the global hygiene brand Reckitt and their commitments to the Clean Naija initiative, provides access to clean water while building long-lasting hygiene habits and community behavioural change. Throughout the next 24 months of Phase 2 programming, WBFA midwives, nurses and healthcare workers will increase the impact and focus on students at schools, mothers and healthcare workers at healthcare facilities, and community members across Lagos, Abuja, and Kwara State.
By recognizing safe drinking water, sanitation, and hygiene as fundamental human rights, we acknowledge the intrinsic value of water in ensuring human dignity and wellbeing. Moreover, we commit to addressing disparities and inequities in access, ensuring that no one is left behind. This inclusivity is not just a moral imperative but also a pragmatic approach towards building resilient and sustainable societies.
Sustainable Development Goal 6 provides a comprehensive framework for action, encompassing targets related to water quality, water use efficiency, water governance, and the protection of ecosystems. Achieving these targets demands innovation, investment, and concerted efforts at all levels. It requires embracing nature-based solutions, investing in infrastructure, promoting water stewardship, and fostering behavioural change.
Beyond meeting basic needs, water plays a pivotal role in driving economic growth and fostering peace and stability. Access to reliable water and sanitation services is essential for industries, agriculture, and energy production, underpinning economic activities and livelihoods. Moreover, water scarcity can exacerbate social tensions and conflict, particularly in regions where resources are scarce.
As featured in The Reckitt Social Impact Investment Report 2023, to address these statistics, and improve outcomes, the Wellbeing Foundation Africa and Dettol Nigeria Hygiene Quest Programme, generously supported by the partnership with the global hygiene brand Reckitt and their commitments to the Clean Naija initiative, provides access to clean water while building long-lasting hygiene habits and community behavioural change. Throughout the next 24 months of Phase 2 programming, WBFA midwives, nurses and healthcare workers will increase the impact and focus on students at schools, mothers and healthcare workers at healthcare facilities, and community members across Lagos, Abuja, and Kwara State.
By recognizing safe drinking water, sanitation, and hygiene as fundamental human rights, we acknowledge the intrinsic value of water in ensuring human dignity and wellbeing. Moreover, we commit to addressing disparities and inequities in access, ensuring that no one is left behind. This inclusivity is not just a moral imperative but also a pragmatic approach towards building resilient and sustainable societies.
Sustainable Development Goal 6 provides a comprehensive framework for action, encompassing targets related to water quality, water use efficiency, water governance, and the protection of ecosystems. Achieving these targets demands innovation, investment, and concerted efforts at all levels. It requires embracing nature-based solutions, investing in infrastructure, promoting water stewardship, and fostering behavioural change.
Beyond meeting basic needs, water plays a pivotal role in driving economic growth and fostering peace and stability. Access to reliable water and sanitation services is essential for industries, agriculture, and energy production, underpinning economic activities and livelihoods. Moreover, water scarcity can exacerbate social tensions and conflict, particularly in regions where resources are scarce.
 Conversely, effective water management can be a catalyst for cooperation and peacebuilding. Transboundary water resources often transcend political boundaries, necessitating collaborative approaches for their sustainable management. By fostering dialogue, building trust, and sharing benefits equitably, water can become a source of cooperation rather than conflict.
The 2024 edition of the United Nations World Water Development Report UNWWDR calls attention to the complex and interlinked relationships between water, prosperity and peace, emphasising that only through the power of united partnerships between the private sector, public sector and governments, can we prioritise financial innovation in water infrastructure as per the World Bank Strategic Framework and the policy, research and development needed to lay the principal foundations of a more water resilient and hygiene harmonious future aligned with the Water Action Agenda.
In doing so, we not only pave the way for a more prosperous and equitable future but also contribute to a world where water becomes a symbol of peace, cooperation, and shared prosperity. Together, let us turn the tide on the global water crisis and usher in an era of water security and sustainable development for all.
Conversely, effective water management can be a catalyst for cooperation and peacebuilding. Transboundary water resources often transcend political boundaries, necessitating collaborative approaches for their sustainable management. By fostering dialogue, building trust, and sharing benefits equitably, water can become a source of cooperation rather than conflict.
The 2024 edition of the United Nations World Water Development Report UNWWDR calls attention to the complex and interlinked relationships between water, prosperity and peace, emphasising that only through the power of united partnerships between the private sector, public sector and governments, can we prioritise financial innovation in water infrastructure as per the World Bank Strategic Framework and the policy, research and development needed to lay the principal foundations of a more water resilient and hygiene harmonious future aligned with the Water Action Agenda.
In doing so, we not only pave the way for a more prosperous and equitable future but also contribute to a world where water becomes a symbol of peace, cooperation, and shared prosperity. Together, let us turn the tide on the global water crisis and usher in an era of water security and sustainable development for all.

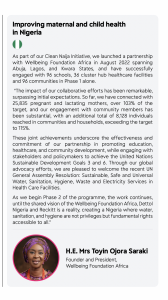
FROM March 8th, 2024
On this International Women's Day, as we inspire inclusion and equitable investments, Nigeria's commendable efforts to strengthen public health through the introduction of the Human Papillomavirus Vaccine (HPV) into routine immunisation, targeting 7.7 million girls, is a monumental stride forward. This initiative, set to be the largest single-round HPV vaccination campaign in the African region, holds promise in combating the virus responsible for nearly all cases of cervical cancer and will accelerate the progress of the global health agenda. As we commend this noteworthy endeavour, I, in my capacity as Founder & President of The Wellbeing Foundation Africa, a distinguished member of the Africa REACH Leadership Council, and the Inaugural Global Health Ambassador for the World Health Organization Foundation, am acutely aware of the profound impact such policies can have on the health and wellbeing of young girls and women. However, while we celebrate this health investment and progress, it is imperative to broaden our focus beyond solely immunisation efforts and shine a light on interconnected groups integral to providing the immunisation and bolstering sustainability in our healthcare systems – midwives, nurses, caregivers and community health workers (CHW), the majority of whom are women, as 67% of the global health and social care workforce are women according to the World Health Organization (WHO). The WHO has identified the need to increase equitable access to healthcare workers by 2030. Many countries with limited health resources have established midwives and women community health workers to be a point of connection between communities and the health system, addressing the need for grassroots-based care, equity of access and health coverage gaps. In most countries, CHWs are female and have a uniquely valuable social and cultural role, just as midwives are also mostly female and have an essential life-saving role for women and newborns. Midwives, nurses and CHWs play pivotal roles in vaccination efforts, particularly in combating HIV transmission, while also addressing Sexual and Reproductive Health and Rights (SRHR) concerns. Midwives and nurses, often serving as frontline healthcare providers, are integral in administering vaccinations, including those aimed at preventing HIV transmission from mother to child. For example, our Wellbeing Foundation Africa Midwives implement the Prevention of Mother-to-Child Transmission (PMTCT) programming within our Mamacare360 antenatal and postnatal classes, ensuring that pregnant women living with HIV receive necessary vaccinations and interventions to protect their infants. Additionally, midwives and nurses provide education and support to mothers regarding the importance of vaccinations for themselves and their children, while also addressing SRHR issues with women and girls such as support for family planning, contraception, information about sexually transmitted infections (STIs), and ensuring access to reproductive health services, thus contributing significantly to improving SRHR outcomes. CHWs, especially women CHWs serve as vital connectors between healthcare facilities and communities, promoting vaccination awareness and facilitating access to services. Often, as trusted members of the community, they advocate for vaccine uptake and provide personal social and health education about the benefits of vaccination, while also addressing SRHR concerns within communities. In the context of HIV, both midwives, nurses and CHWs are instrumental in the implementation of HIV vaccination programmes, such as administering vaccines for hepatitis B, which can significantly reduce the risk of HIV transmission. They also provide essential support and guidance to individuals living with HIV, emphasising the importance of adherence to vaccination schedules and other preventive measures. The roles of midwives, nurses and CHWs in vaccination efforts, particularly concerning HIV, are indispensable in advancing public health goals and promoting comprehensive SRHR services. A commentary published by the National Library of Medicine highlights that while PMTCT programs historically emphasised preventing HIV transmission from mother to child, there's a pressing need to prevent HIV in women of reproductive age, prevent unintended pregnancies in women living with HIV and enhance maternal and sexual and reproductive health services. Our public health strategies and policies must embrace this 360 approach, acknowledging the unique health challenges faced by women throughout their reproductive years, and engendering our midwives, nurses and women CHWs to support them. Recognising the indispensable roles of midwives, nurses, caregivers and CHWs, I, together with my fellow Africa REACH Leadership Council members, issue a heartfelt call to action, urging governments not only to prioritise maternal vaccines but also to provide unwavering support to these dedicated individuals and the crucial work they do in vaccine administration and uptake. We as WBFA and Africa REACH assert that self-sufficiency in vaccine production is essential for the nation, highlighting the need to strengthen Primary Healthcare Centres (PHCs) to fulfil their role in keeping people well and addressing uncomplicated ailments. The recent announcement on HPV vaccination is a positive step, but it is just the beginning. The alarming situation of cervical cancer and breast cancer as leading causes of death for women in Nigeria underscores the urgency for a more integrated approach. I continue to advocate and express my concern over the limited availability of resources and diagnostic tools, emphasising the need for a more comprehensive healthcare infrastructure to alleviate screening challenges, which not only impede early detection and treatment but also exacerbate the burden of preventable diseases on women's health. This International Women's Day, let us collectively advocate for comprehensive legislation, policies, sustainable financing, and ongoing global support are essential to fortify the efforts of these frontline female heroes, not just today but every day! Signed, Her Excellency Toyin Ojora Saraki
FROM February 27th, 2024
As an inaugural member of the Africa REACH Leadership Council, convened and chaired by H.E. Monica Geingos, and dedicated to advancing the health and wellbeing of children, adolescents, and young people in the fight against HIV/AIDS, I am honoured to reflect on our journey as we mark the one-year anniversary of our African-led, African-focused efforts to fulfil the promise of an AIDS-free generation in Africa. This milestone is a testament to our collective dedication, resilience, and unwavering commitment to health for all. From the formal launch at the African Union Heads of States Summit and the Organisation of African First Ladies for Development General Assembly in Addis Ababa in February 2023, Africa REACH, guided by our Strategic Plan 2023-2025, has forged formidable partnerships within the HIV response community with allies such as the African Union Commission, AIDS Watch Africa, Elizabeth Glaser Pediatric AIDS Foundation, ViiV Healthcare, and Desmond Tutu Health Foundation, to actively engage in advocacy at both national and continental levels, positioning Africa REACH as a catalyst for change, from funding community-led initiatives across Africa to initiating policy change at the highest levels. As we review the past twelve months, we recognise that our mission demands continuous innovation and a relentless pursuit of progress to end AIDS in children and young people in Africa by 2025, and as we aim to achieve the promises of the Abuja Declaration, through ensuring the pledge that each African nation allocates 15% of their annual budgets to the health sector.
FROM February 27th, 2024
The promise of a more equitable world, as outlined in the United Nations Sustainable Development Goals, hinges significantly on the health and rights of women and children. However, this promise remains unfulfilled, marked by gaping inequities which fuel global health crises. Without addressing these disparities, our aspiration for a healthier, safer, and fairer world by 2030 will remain fleeting. Despite a 38% decline in the global maternal mortality ratio from 2000 to 2020, the pace of reduction falls short of the target needed to achieve the Sustainable Development Goal of 70 maternal deaths per 100,000 live births. In Nigeria, the situation reflects this global trend, with maternal mortality rates remaining unacceptably high. Data from Nigeria underscores the urgency of the situation, with an estimated 1047 maternal deaths per 100,000 live births, the third highest in Africa(1). This stark reality emphasises the pressing need for accelerated action to address maternal health disparities and improve outcomes for mothers and newborns across the country. The landscape of maternal and newborn health in Nigeria is characterised by both challenges and triumphs, and while progress has been made, particularly through the efforts of dedicated healthcare professionals, policymakers, and international partners, exemplified by initiatives such as the Federal Government's National Emergency Maternal and Child Health Intervention Centre #NEMCHIC and State Emergency Maternal and Child Health Intervention Centres #SEMCHIC, which serve as catalysts for change at both national and grassroots levels, the persistence of high mortality rates underscores the need for sustained community action on the frontlines, which the Wellbeing Foundation Africa champions as the leading non-governmental organisation advocating to reach the most vulnerable populations, and implementing programming for quality maternal, newborn and child healthcare. Central to these efforts is the promotion of community midwifery, which plays a vital role in delivering essential care to expectant mothers, particularly in rural areas. The Wellbeing Foundation Africa Midwives, trained and supported by WBFA, not only provide the World Health Organization recommended antenatal and postnatal classes through Mamacare360, alongside other clinical services but also serve as trusted members of their communities, working with adolescent in bolstering Personal, Social, Health and Economic #PSHE and Water, Sanitation and Hygiene #WASH, education, while addressing socio-cultural factors that impact maternal, newborn, child and adolescent wellbeing. The Wellbeing Foundation Africa has been instrumental in driving progress for initiatives such as Basic Emergency Obstetric and Newborn Care #BEmONC and Emergency Obstetric and Newborn Care #EmONC, a set of seven key obstetric services, or ‘signal functions,’ a life-saving intervention, introduced by the WHO, UNICEF, and UNFPA in 1997 as an organising framework for the delivery of evidence-based clinical services, as a critical component of any programme to reduce maternal and newborn mortality, with skilled birth attendants providing these services within the context of community-focused and facility-based health systems, enabling timely prevention of and intervention for these complications and saving the lives of mothers and newborns(2). Supported by community midwifery and strategic partnerships, WBFA is committed to providing universal access across Nigeria to EmONC, which is considered essential to reduce maternal mortality and requires that all pregnant women and newborns with complications have rapid access to well-functioning facilities that include a broad range of service delivery types and settings(3). Receiving care at health facilities is crucial for maternal and newborn health, but it involves more than just access. Factors such as the organisation of facilities, the quality of care provided, and the availability of trained staff and essential equipment play pivotal roles. Efficient management of obstetric emergency situations relies on addressing these factors comprehensively. However, it's essential to acknowledge that success in maternal health programmes require facility readiness but also addressing the three delays: delay in seeking care, delay in reaching care, and delay in receiving care. The strategic partnership between the Wellbeing Foundation Africa, the United Nations Population Fund, exemplified this, as together, we have continuously orchestrated transformative advocacy and policy campaigns, rooted in the essence of SDG 3, Good Health and Well-Being, to tackle all three delays, as without doing so, the effectiveness of any safe motherhood programming will be limited. Given these essential evidence based learnings, the Wellbeing Foundation Africa is looking forward to implementing our new programme, Advanced Emergency Obstetrics and Newborn Care competency-based curriculum for resident doctors in obstetrics and gynaecology at the National Postgraduate Medical College of Nigeria, in partnership with our long-standing allies, the esteemed Liverpool School of Tropical Medicine in 2024. The overall goal of the project is to improve the availability of quality advanced EmONC at national and sub-national hospitals by strengthening the capacity of the National Postgraduate Medical College of Nigeria to deliver advanced EmONC competency-based curriculum to resident doctors in Obstetrics and Gynaecology, taking significant strides towards strengthening Nigeria's healthcare workforce. A project of the Global Health Workforce Programme Grant, funded by the UK Department of Health and Social Care and managed by the Tropical Health and Education Trust and Ducit Blue, the programme has the ambition of achieving more resilient health systems for post-pandemic recovery and supporting progress toward Universal Health Coverage, and will engage experts from the Royal College of Obstetricians and Gynaecologists and experienced master trainers in advanced EmONC from LSTM. The objectives of the project include engaging with stakeholders in post-graduate medical education in OBGYN to agree and adapt the training package for revision courses and examination OSCE, identifying host institutions in Abuja and Lagos to establish one advanced EmONC Centre of Excellence (CoE) in each site, establishing a sustainable system for operating the CoE for postgraduate OBGYN revision courses in advanced EmONC, supporting the NPMCN in providing training to residents and ensuring quality assurance of the training at the CoE, and evaluating the programme for accountability and dissemination purposes. Post-training, health workers will be equipped with the knowledge and skills to provide timely and appropriate care for pregnant women and newborns, including identifying and managing complications, conducting safe deliveries, and providing postpartum care. The Advanced EmONC training programme is expected to impact maternal and child health outcomes in Nigeria significantly, reducing the risk of maternal and newborn deaths will improve overall health outcomes for women and children in the region. The programme's success will be testament to the commitment and collaboration of the Federal Ministry of Health and Social Welfare, national and international partners, and the dedicated health workers in Nigeria. Alongside this, the commitment shown by the NEMCHIC and SEMCHIC demonstrates a crucial political will to extend the gains achieved in Primary Health Centers, where the seven skills and drills are most needed. This concerted effort is essential for ensuring that maternal and newborn health initiatives are effectively implemented at the sub-national level with policy and advocacy at the national level, thereby making significant strides towards reducing maternal and newborn mortality rates throughout Nigeria. The greatest lifetime risk for a mother and her baby occurs during childbirth, therefore as we continue our work in achieving the 2030 Agenda, sustained investment in community midwifery, alongside strategic partnerships and training-led, data-driven interventions, is essential to overcoming the barriers to maternal and newborn health in Nigeria. By honouring the promise of motherhood and ensuring access to quality care for every woman and child, we can transform the landscape of maternal and newborn health for generations to come across Africa. _______________________________________________ (1) World Health Organization, UNICEF, United Nations Population Fund and The World Bank, Trends in Maternal Mortality: 2000 to 2020 WHO, Geneva, 2023. (2) World Health Organization. Making pregnancy safer: the critical role of the skilled attendant: a joint statement by WHO, ICM and FIGO. World Health Organization, 2004. (3) Campbell, Oona MR, and Wendy J. Graham. "Strategies for reducing maternal mortality: getting on with what works." The Lancet 368.9543 (2006): 1284-1299.
FROM February 16th, 2024
I was delighted to join and provide a goodwill keynote message at the Nigeria Launch of the Global Health Workforce Programme in Abuja yesterday, alongside the Wellbeing Foundation Africa Team, hosted by the Federal Ministry of Health and Social Welfare Nigeria, in partnership with The Tropical Health and Education Trust - THET, and Ducit Blue Solutions. With the announcement of 33 Health Partnerships as successful grantees of the Global Health Workforce Programme across Ghana, Kenya and Nigeria, funded by the UK Department of Health and Social Care, the Global Health Workforce Programme will develop the health workforce, supporting them to build more resilient health systems for post-pandemic recovery and to make progress towards universal health coverage. In addressing critical health partners, stakeholders, and the 10 successful grant partnerships from Nigeria, including the Wellbeing Foundation Africa and the Liverpool School of Tropical Medicine - LSTM Partnership, I emphasised the importance of fostering local ownership and sustainability, as each partnership will advance programmatic outcomes, such as enhancing health workforce leadership capacity in alignment with strategic health workforce initiatives, advocating for a reduction in gender disparities, and improving both the quantity and quality of training opportunities for healthcare professionals. Highly skilled, resilient staff are the backbone of a strong health service, and the grants launched today will vastly impact the performance of health systems in Nigeria, having a knock-on effect on boosting global pandemic preparedness and reducing health inequalities globally, as over one billion people have no access to qualified health workers. The Launch was also marked by Goodwill Messages from the Representatives of the Hon. Coordinating Minister of Health and Social Welfare, Prof Muhammad Ali Pate, represented by Dr Chris Isokponu, Director of Health Planning, Research and Statistics, British High Commissioner H.E. Richard Montgomery, represented by Dr Ebere Anyachukwu, Health Adviser, Foreign Commonwealth and Development Office Nigeria, and Country Director WHO Nigeria, Dr Walter Kazadi Mulumbo, and Head, Health Systems Strengthening, Dr Nwakaego Chukwukaodinaka, respectively.
FROM February 12th, 2024
With the goal of "Empowering Africa: Unveiling the Hidden Drivers Shaping Tomorrow," I am honoured to have delivered my keynote address at the 10th Annual St Andrews Africa Summit, a commendable student-led and university-supported initiative dedicated to the challenges and opportunities we face on the continent. I am particularly heartened by the summit's focus on women and children's health alongside science and technology, especially as we commemorated the United Nations International Day of Women and Girls in Science, yesterday, emphasising women’s leadership in science to foster a new era for sustainability, while driving socio-economic development. From improving health to combating climate change, women and girls play a critical role in the science and technology communities, and it is essential that their participation is strengthened, especially since STEM is widely regarded as critical to national economies across Africa. I urged each student to seize the opportunity to be inspired, to learn, and to commit to action, as we are reminded of the transformative impact that collective action can have. Through platforms like such, we can foster open and respectful political dialogue, inspire technical innovation, and mobilise sustainable resources, leading to the unveiling of the hidden drivers shaping tomorrow's Africa, a future defined by hope, resilience, prosperity, and boundless opportunity. Watch the Keynote: [video width="1200" height="1200" mp4="https://toyinsaraki.org/wp-content/uploads/2024/02/Keynote.mp4"][/video] Written Keynote: Ladies and gentlemen, esteemed guests, and students of St. Andrews, It is with immense pleasure that I join you today on this momentous occasion, as we gather for the 10th annual St. Andrews Africa Summit. For a decade now, the St. Andrews Africa Summit has served as a platform for dialogue, collaboration, and action on the pressing issues facing Africa—a testament to the unwavering commitment of this student-led initiative and university-supported endeavour towards a more empowered Africa. As the Founder-President of the Wellbeing Foundation Africa, and Inaugural Global Health Ambassador for the World Health Organization, I am deeply honoured today to join you in exploring this year's theme: "Empowering Africa: Unveiling the Hidden Drivers Shaping Tomorrow." This theme resonates profoundly with the challenges and opportunities we face on the continent, and I commend the organisers for their foresight in selecting such a vital topic, especially as 18 African countries, a third of the population in Africa, head to the polls in 2024. The importance of democratic governance cannot be overstated. Democracy empowers citizens, especially our youth to participate in the decision-making process, ensuring their voices are heard and their needs addressed. With a flourishing youth population, the voices and votes of young people have the power to drive meaningful change and pave the way for a more inclusive and prosperous Africa. As we reflect on the journey of the St. Andrews Africa Summit over the past decade, we are reminded of the transformative impact that collective action can have on shaping the future of our continent. It is through platforms like this one today, in which we can foster open and respectful political dialogue, inspire technical innovation, and mobilise sustainable resources to ensure Africa prospers. I am particularly heartened by the focus on women's and children's health, empowerment, and socio-economic development—a cause that lies at the very heart of the Wellbeing Foundation Africa’s mission. For too long, women and children have borne the brunt of inequality across Africa, while being denied access to essential and quality healthcare, education, and economic opportunities. Yet, as we gather here, we stand on the cusp of change—a change that begins with each and every one of us. At the core of the Wellbeing Foundation Africa’'s initiatives lies a commitment to holistic healthcare, education, and advocacy. Through strategic programming, advocacy and global partnerships, WBFA tackles the root challenges of maternal, newborn and child health while uplifting and empowering communities to build a healthier, brighter future. Beyond policies and programmes, it is our collective will and determination that will truly drive progress. It is the belief that every individual in Africa has inherent worth and potential—that no one should be left behind—that will propel us forward on this journey of empowerment and transformation. As we embark on this summit, I urge each and every one of you to seize this opportunity to be inspired, to learn from one another, and to commit to action. For it is through our joint efforts that we will unveil the hidden drivers shaping tomorrow's Africa—a future defined by hope, resilience, and boundless opportunity. Together, let us empower Africa and unleash its full potential. Thank you.
FROM February 4th, 2024
My sincere condolences to the resilient nation of Namibia as they mourn the loss of President H.E. Dr. Hage G. Geingob, announced by Vice President Nangolo Mbumba, this Sunday morning. During this sad time as we mourn the loss of a greatly beloved and respected African leader, my thoughts and prayers are especially with my dear sister and friend, H.E. Monica Geingos, and their family. President Geingob's lifetime of steadfast dedication to the progress of Namibia, as their first elected leader, longest serving Prime Minister, and a key figure in the development of~ the constitution, has left an enduring legacy of visionary leadership, liberation efforts and unwavering commitment to the betterment of his nation, through an all-of-government egalitarian effort at poverty eradication, leadership transparency, gender equality and economic prosperity resonated not only within Namibia but reverberate across the continent and beyond. May the everlasting impact of President Geingob's impeccable integrity be a guiding light, inspiring generations to come. May the grace of God bestow upon his family and the entire nation of Namibia the collective strength, unity and peace as they navigate this profound loss. H.E. Toyin Saraki Founder & President The Wellbeing Foundation Africa Leadership Council Member: Concordia Summit & AfricaReach
FROM February 1st, 2024
I am delighted to congratulate a dear friend, Dr Dupe Elebute-Odunsi MBBS (Lagos), MD (Lond), FRCP, FRCPath, Co-Founder, Marcelle Ruth Cancer Centre, Founder-Chair, Women in Health Care Network Nigeria, and all the Founding Members of WIHCN which was launched yesterday in Lagos. Globally and at home in Nigeria, 70% of the health workforce is powered by our female gender, yet less than 35% of health leadership roles are held by women, thus, I heartfully welcome WIHCN's encouraging vision to #connect, #inform and #inspire women in the healthcare industry in Nigeria to become the best they can be individually, and in the long term, positively impacting the delivery of healthcare in our beloved country. I look forward to WIHCN's future impact in challenging the obstacles of women attaining and succeeding in leadership roles, gender disparity in obtaining financial support for business ventures, and then building focused mentorship programs to encourage the return and retention of our talented younger generation to pursue their health sector careers here at home in Nigeria. Joining the Honourable Coordinating Minister For Health and Social Welfare, Professor Muhammad Ali Pate CON, Dr Salma Ibrahim-Anas, Special Adviser to the President on Health, Dr Uju Rochas-Anwukah - Special Assistant on Public Health, Office of the Vice President, Special Guests of Honour, Dr Olajide Idris and Hon Abike Dabiri-Erewa OON, Chair, Nigerians In Diaspora Commission, stakeholders and supporters in observing the launch, I extended the best wishes of The Wellbeing Foundation Africa to all WIHCN Members as the network initiates and pursues it's warmly anticipated goals
FROM January 31st, 2024
I started this week by honouring the invitation of CCI France-Nigeria to observe their January Breakfast Meeting discussion: 'A Bird's Eye View Of The Nigerian 2024 Economy'. Joining Laurent Favier, Consul General of France to Nigeria who delivered the welcome address, Mr Taiwo Oyedele, Chairman, Presidential Fiscal Policy and Tax Reform Committee, learned legal luminary Dr Olisa Agbakogba SAN, Christian Mulamula, Head of Office, International Finance Corporation Nigeria, and many distinguished panellists sharing their viewpoints and experience, I appreciated the enlightening opportunity to engage extended by Alhaji Usman Mohammed, Chairman, Board of Directors, CCI France-Nigeria.
FROM January 30th, 2024
On World Neglected Tropical Diseases Day, I echo the World Health Organisation on calling for global and community leaders to unite and act to address the inequalities which drive Neglected tropical diseases, and make sustainable investments to bring health and wellbeing to the estimated 1.62 billion people affected in vulnerable cycles of disease and marginalisation. As World Leprosy Day was observed yesterday, a disease caused by infection with a slow-growing bacterium, which currently occurs in more than 120 countries, with more than 200 000 new cases reported every year, it is a reminder that this #NTD, like all others, is completely preventable, can be easily cured if not neglected, and in many cases, can be fully eliminated from countries. As community trusted caretakers and healthcare providers, the Wellbeing Foundation Africa actively works to raise the awareness, and profile of suffering, on neglected tropical diseases, to garner support towards their control, elimination and eradication, in line with the programmatic targets set out in the World Health Organization NTD Road Map 2021−2030 and the commitments of the 2022 Kigali declaration on Neglected Tropical Diseases. As The Wellbeing Foundation Africa re-commits to Ending Neglected Tropical Diseases Together Towards 2030, there must be a shift towards accountability, accelerating programmatic action, collaboration and multisectoral action, strengthening country capacity and ownership, and mobilising resources through long-term financing. 📸: Private viewing of the exhibition Reframing Neglect at Cromwell Place in London, hosted by The End Fund and supported by Reaching the Last Mile.
FROM January 25th, 2024
The Wellbeing Foundation Africa Davos Delegation was honoured to join Kearney, FemTechnology, and senior executives from established global organisations to support an open letter highlighting the gender inequity in healthcare. Redesigning healthcare with women in mind: an open letter supports the World Economic Forum Global Alliance for Women’s Health, a newly formed community to convene and connect on next steps, in which The Wellbeing Foundation Africa is has submitted commitments to, to prioritise, protect, and promote the health of women and closing the women’s health gap. A huge undertaking, this letter is addressed to all those within the healthcare ecosystem whose innovations have impact and decisions have power: from pharma, biotech, and medtech firms to investors, tech companies, and consumer health players serving women and girls. The parity can only be achieved with the involvement of players across the entire healthcare value chain, and with collaborative support, we hope to make this 2024 World Economic Forum Annual Meeting the start of our journey together toward a new global healthcare system that serves women better. Through shaping the public health agenda with increased advocacy and awareness, overhauling medical education by expanding both national school and higher education curriculums, raising the stakes on research and development by increasing the volume of clinical and policy research trials on women’s health conditions, building women-centric integrated care pathways that are accessible and easy to navigate, covering all patient touchpoints and providing women with more control over their own health, getting serious about data by ensuring gender-specific data sets are collected, accelerating investment by boosting funding for academic research development, we can make the necessary and long overdue change needed. Together, let us Rethink what equitable healthcare means, Resync all stakeholders around this new mission and Regenerate healthcare systems to root equity at their core. From Davos, Switzerland at the 54th Annual World Economic Forum, reported by Zelia Bukhari (Global Health Advocacy and Policy Manager, Global Davos Delegation, The Wellbeing Foundation Africa).
FROM January 24th, 2024
Learning for Lasting Peace On the occasion of the United Nations, UNESCO International Day of Education, I am reflecting on how the foundation of a more peaceful, just, and sustainable society is laid through education, a force which permeates every facet of daily life and opportunity. As climate change, democratic erosion, persistent inequalities and conflict escalate on a global scale, education emerges as a powerful tool to both address these pressing issues and prevent these challenges in the future, as when education is effectively shaped and implemented, it becomes a long-term investment with increasing returns. Therefore, it is imperative to actively reaffirm the Wellbeing Foundation Africa’s dedication to the cause of peace throughout Nigeria and Africa, emphasising the pivotal role that education plays in this pursuit. Learning for peace is a transformative process, and through The Wellbeing Foundation Africa’s Adolescent Skills and Drills Personal Social Health Education-PSHE, WASH Programming which takes place not only in schools but also throughout communities, as according to UNICEF one in every five of the world's out-of-school children is in Nigeria, WBFA enables learners to gain essential knowledge, values, attitudes, skills, and behaviours, thereby empowering them to serve as catalysts and advocates for peace, health and wellbeing in their schools, homes and communities. Today, The Wellbeing Foundation Africa commemorated #EducationDay at schools in Abuja FCT, Kwara and Lagos State, with a specific focus on educating adolescents and teachers to prevent gender-based violence and build social cohesion to combat dropout rates, and absenteeism in schools. While I was First Lady of Kwara State, the Education Sector Support Programme began in 2008, a partnership between the United Kingdom’s Department for International Development and the Kwara State and Nigerian Government, to develop effective planning, financing and delivery systems to improve the quality of schools, teaching and learning, especially in delivering health education services. WBFA continues to utilise the statistics shared to track indicators, as ESSPIN embedded an integrated school improvement programme at scale, building the capacity of state and district staff, teachers, and school-based management committee members to improve education in primary schools across Kwara State. Successfully contributing to achieving the Sustainable Development Goals 3, 4, 5, and 6, and the UNESCO Recommendation on Education for Peace, Human Rights and Sustainable Development, and the report of the International Commission on the Futures of Education, the integration of PSHE is instrumental in creating a generation of well-informed and responsible global citizens, especially in the face of uncertainties.
FROM January 23rd, 2024
A history of collaboration & mutual respect It is an honour and a privilege to extend my felicitations to Her Majesty Queen Mary of Denmark on the ascension of His Majesty King Frederick X to the throne. I have long admired and respected Her Majesty Queen Mary of Denmark’s dedication to her duties on behalf of the Danish monarchy, and her compassionate and impactful advocacy and actions. As Patron of the United Nations Population Fund since 2019, HM Queen Mary assiduously and steadily supports the agency's work to promote maternal health and safer motherhood in more than 150 developing nations. A member of the International Committee of Women Leaders for Mental Health, and as a patron supporting over 30 charitable organisations including the European Regional Office of the World Health Organisation WHO-EMRO, the Danish Refugee Council and Julemærkefonden, she also founded her award-winning social organisation, the Mary Foundation, in 2007. Becoming Her Royal Highness Crown Princess upon her 2004 marriage to then Crown Prince Frederik, Mary was made a Rigsforstander in 2019, which allows her to act as regent when the monarch is abroad. She became the first Australian-born queen consort upon the abdication of her mother-in-law, Queen Margrethe II, on 14 January 2024. HM Queen Mary's unwavering support for maternal health aligns seamlessly with The Wellbeing Foundation Africa’s mission to enhance the health and wellbeing of women and children across Nigeria. As champions of impactful and sustainable development, we share the values of compassionate leadership in fostering positive change on a local and global scale, to promote a brighter, healthier, future for all. As I felicitate with the Kingdom of Denmark and my Wellbeing Foundation Africa's Partners, UNFPA, and Maternity Foundation Denmark, I take this opportunity to recognise Denmark's commendable historical standing as the first nation to recognise, regulate and therefore respect and elevate the midwifery profession, and the nation's continued unflinching support for the ICPD25 efforts globally.
FROM January 19th, 2024
From Davos, Switzerland at the 54th World Economic Forum: The Wellbeing Foundation Africa Delegation was thrilled to join in launching forthcoming research by the McKinsey Health Institute and the World Economic Forum with leaders across the public, private, social, and philanthropic sectors for an action-oriented convening to explore the latest data powering the effort to draw awareness to the women's health gap. The report titled "Closing the Women's Health Gap: A $1 Trillion Opportunity to Improve Lives and Economies," emphasizes that investments addressing the women’s health gap would add years to life and life to years – while potentially boosting the global economy by $1 trillion annually by 2040. When discussing the challenges in women’s health, a common rejoinder is that women, on average, live longer than men. But this neglects the fact that women spend 25% more of their lives in debilitating health. Closing the women's health gap would allow 3.9 billion women to lead healthier, higher-quality lives. The report identifies four primary areas that need addressing to close the health gap: Science, Data, Care Delivery, and Investment, to move forward, the report suggests action on five fronts: investing in women-centric research, strengthening the collection of sex-and gender-specific data, increasing access to women-specific care, creating incentives for investment in women's health innovation, and implementing policies supporting women's health. Closing the women's health gap is a moral imperative, as addressing these gaps would reduce the time women spend in poor health by almost two-thirds, adding an average of seven days of healthy living for each woman annually. Together, we have a chance to lift millions of women out of poverty, improve future generations' health, and foster healthy ageing. We cannot succeed when half of us are held back. Reported by Zelia Bukhari (Global Health Advocacy and Policy Manager, Global Davos Delegation, The Wellbeing Foundation Africa).
View this post on Instagram
FROM January 16th, 2024
As the 54th Annual Meeting of the World Economic Forum convenes in Davos this week under the theme Rebuilding Trust, I am reflecting on the learnings and dialogue from last year, and how it is crucial now more than ever to focus on the fundamental principles of driving transparency, consistency and accountability in a world of constant transformation. Especially as we take on the agreement from COP28 at Dubai-UAE, it is evident that urgent action is needed to combat the climate crisis, for the health of the planet and its people. Throughout the week, it is vital to collaborate on how to accelerate progress and improve health outcomes, looking at how climate change affects health, how to close the women’s health gap and how digital tools can transform healthcare, especially #AI, all which will be captured in three key reports, anticipated to launch at the end of the World Economic Forum 24. Embracing the youth voice is also essential in repairing trust with the next generation, as we work towards building a healthy world for them to inherit, and scale up life-saving and life-changing investments for adolescents while honouring commitments to tackle inequalities and create future opportunities. Fundamental to the long-term global health strategy are open platforms for dialogue, stronger private-public sector partnerships, agile policy frameworks and effective deployment of innovative technologies that can lead to practical and implementable gains. The Wellbeing Foundation Africa Davos Delegation to 54th World Economic Forum, will be aiming to instil a measure of collective agency, as together, we work towards restoring wellbeing and trust at three fundamental levels: into the future, within societies and among nations.
View this post on Instagram
FROM December 12th, 2023
Today, I was honoured to join Nigeria’s National Population Commission Nigeria, and UNFPA Nigeria Partners in commemorating the Fourth Anniversary of the Nairobi Summit on ICPD25+4: Accelerating The Promise. In my Stakeholders Goodwill Keynote delivered virtually, and contained in the Wellbeing Foundation Africa Progress Report, I emphasized the pivotal importance and transformative impact of addressing issues of population management and development with particular attention on women, girls and young people. Observing the 4th Anniversary under the theme - “Sexual and Reproductive Health Justice Cannot Wait: All Rights, Women, Girls & Young People, Act Now,” Nigeria has remained committed to realising the three (3) transformative results expressed as Zero Preventable Maternal Death, Zero Unmet Need For Family Planning, and Zero Harmful Practices that are against women and girls, including Gender-Based Violence. The Nairobi Summit, on whose International Steering Committee I serve, created an enduring platform for effective and productive engagements for advancing the implementation of the Programme of Action of the International Conference on Population and Development, the 2030 Agenda and its 17 Sustainable Development Goals.
FROM December 8th, 2023
Championing Climate-Resilient WASH Innovation Ahead of World Climate Day, and as I rounded up my COP28 UAE engagements on Wednesday, I was honoured to share the Wellbeing Foundation Africa's frontline impact and learnings on WASH with DP World at the Climate Challenge Lab, Innovation Zone, Madinat Jumeirah, Dubai. In my Fireside Chat with Ayla Bajwa, Senior Vice-President of Group Sustainability at DP World, we discussed the escalating frequency and severity of extreme weather events, and how it becomes increasingly important to address the convergence of climate change and WASH, including the role WASH plays in health. I shared a deep dive into the current landscape of climate-resilient WASH best practices, and the innovative strategies, technologies, and policy frameworks, all aimed at empowering communities to adapt and thrive in the face of climate-related adversity, implemented at the Wellbeing Foundation Africa. In alignment with the insights shared at the 2023 UN Water Conference, which I attended and spoke at earlier this year with longstanding WASH partners Reckitt, and the corresponding Water Action Agenda, I highlighted the need to enhance the impact of frontline programming which works towards achieving Sustainable Development Goal 3, 6, and 17. Spotlighting the contributions made by funders, the private sector, practitioners, and other stakeholders, I very much valued the experience brought to this important discussion, through the additional panel, moderated by Kevin Holliday, Managing Director, C3, featuring Tim Wainwright, Chief Executive, Water Aid UK, Pawan Borle, Co-Founder & International Advisor, Maithri Aquatech and Cheryl Hicks, Senior Advisor, CEO Water Mandate, WASH4Work Global Compact, as we navigate the ever-evolving terrain of climate-resilient WASH, ensuring unwavering access to clean water, sanitation, and hygiene, even in the face of the challenges posed by our changing world.
FROM December 7th, 2023
Sustainable & Gender Inclusive Trade as An Engine of Economic Growth & Prosperity! On the conclusion of Gender Day and Trade Day COP28 UAE, I was honoured to join the High-Level Reception in the Blue Zone, to explore the critical interplay between trade, gender and climate solutions as drivers for equitable economic development. Hosted by DP World, distinguished leaders such as DP World Group Chairman and CEO, Mr. Sultan Ahmed Bin Sulayem, Director-General of the World Trade Organization, Dr. Ngozi Okonjo-Iweala, and Former U.S. Secretary of State, The Hon. Hillary Clinton shared their visionary perspectives centred on a collective commitment to fostering an environment where the flow of trade becomes a catalyst for sustainable change. Trade is the lifeblood for many, including women, young people and entrepreneurs, opening the doors to opportunity and connectivity for all, while fostering resilient and thriving communities. Together, we must prioritise the amplification of diverse voices and inclusive policies to drive tangible change in our pursuit.
FROM December 6th, 2023
Catalysing Gender Equity in Climate Finance: Accelerating Progress at the Intersection of Climate, Gender & Health Taking place in the World Green Economy Organization WGEO Pavilion COP28 UAE Blue Zone, I was honoured to launch the USAID’s Climate Gender Equity Fund (CGEF), with committed founding members Reckitt, Amazon and Visa Foundation. Focused on scaling climate finance that advances gender-responsive climate solutions, I shared programmatic insights on the health gap in the climate and gender nexus, detailing how pivotal health-focused funding is, and calling to action for strategically aligned and interested funders to join the Climate Gender Equity Fund and increase access to finance for gender-responsive climate initiatives. The climate crisis continues to have a disproportionate health impact on women and girls. Research shows that women face more climate-related health issues than their male counterparts, carry additional burdens as primary carers in their households, and often place their needs last. Women and girls are also uniquely equipped to serve at the frontlines of climate mitigation and adaptation. Research demonstrates that women entrepreneurs are not only more likely to innovate to address social needs, but they also generate more revenue per dollar invested and produce a greater return. Together, we must support the development of climate mitigation and adaptation businesses and solutions by directly funding climate-smart women-led and women-benefiting investments.
FROM December 6th, 2023
I was pleased to join my Wellbeing Foundation Africa partner Reckitt for a roundtable discussion on tackling the spreading vector threat with new research insights from academic ally London School of Hygiene & Tropical Medicine, to converse regarding the choices we need to make as the global policymakers, health workers, and private-sector industry committed to ending the growing threat of vector-borne disease, in our changing climate. Currently, 80% of the world’s population is at risk of one or more vector-borne diseases as a result of climate change and human behaviour which is multiplying new and more disease organisms, spreading them to new places, and becoming resistant to insecticides, putting many families at risk. I was thrilled to test new virtual reality technology based on analysis by the London School of Hygiene & Tropical Medicine, to bring to life the real-world implications of the growing ‘pest threat’ and further inform how we can respond and adapt in the face of climate change, including how we minimise exposure, protect the most vulnerable populations, improve global monitoring and health education, and tackle the human behaviours that are worsening the spread.
FROM December 5th, 2023
Zero Malaria: Change The Story I was pleased to join Malaria No More UK, African Leaders Malaria Alliance and global health partners at #COP28 for a special pre-dinner reception at Goals House in Dubai which showcased a new campaign film directed by Grammy-award winner Meji Alabi, featuring Zero Malaria Ambassador David Beckham and Kenyan youth climate champion Ellyanne Wanjiku Chlystun Githae, with a special performance from Ugandan super-star children, The Ghetto Kids. With global crises and growing threats, the fight against malaria, one of humankind’s oldest and deadliest diseases, is becoming more challenging. Climate change is making malaria harder to predict and control. Throughout the evening, I joined leaders, such as my longtime ally and sister, Joy Phumaphi to discuss and address malaria’s impact on human health when taking action to tackle climate change, particularly as it takes the life of a child every minute. By sharing the human stories of children who are most impacted and highlighting the importance of creative communications and advocacy in overcoming the devastating impact of climate change on the spread of malaria, we can amplify our efforts to end the disease. 📷: Sam Churchill
FROM December 5th, 2023
COP28 to unite, act, and forge a healthier, more resilient future together! Returning to COP28 in Dubai, for the long-awaited and greatly welcomed first ever Health Day at the UN Climate Change Conference - United Arab Emirates (COP28 UAE), which featured the Climate and Health Ministerial Main Event, and the Reaching the Last Mile Forum! The 2023 Reaching the Last Mile Forum, anchored by the longstanding global health heritage of Chelsea Clinton of the Clinton Global Initiative, and attended by our own Nigerian Coordinating Minister of Health and Social Welfare, Professor Muhammad Ali Pate, who presented our national commitments, served as one of the most impactful platforms, delivering concrete commitments in support of effective climate-health action, under the patronage of His Highness Sheikh Mohamed bin Zayed Al Nahyan, President of the UAE, in collaboration with the Bill & Melinda Gates Foundation. Learning and listening to the Health Ministers, it was clear that we are globally committed to ending preventable diseases that affect the world’s poorest and most vulnerable communities and helping millions of children and adults live healthy, dignified lives, even in the face of climate change. The Wellbeing Foundation Africa’s long term commitments, focusing on areas where we can have maximum impact and prompt action to foster change, call for active partnership, innovative financing, and the development of new areas for the progress of the climate-health nexus, focused on improving the sustainability of health system infrastructure.
FROM December 5th, 2023
Measurably Improving Health & Wellbeing through the Arts! As the Inaugural Global Health Ambassador of the WHO Foundation, I was honoured to address the high-level private dinner, following the COP28 Health Day Closing, co-hosted by Community Jameel and the WHO Foundation, featuring the partnership launch of the Jameel Arts Health Lab. I joined my dear brother WHO Deputy-General, DrTedros, CEO of WHO Foundation Anil Soni, Co-Director of the Jameel Arts & Health Lab and WHO Arts and Health Lead, Christopher Bailey, Chief of Operations, High-Level Climate Champions, Lisa Larsen, and Director of Community Jameel, George Richards, to amplify and advocate for action at the nexus of wellbeing, climate and relief, recovery and peace. Focused on overlooked and underserved communities, including those who are suffering from the climate crisis, the Jameel Arts & Health Lab aims to coordinate and amplify scientific research into the effectiveness of the arts in improving health and wellbeing. Leveraging data, artist-led advocacy and a global “Healing Arts” campaign, the Lab seeks to drive policy implementation across 193 UN member states. The dinner was graciously hosted by Fady Jameel, Vice Chairman of Community Jameel, who opened his family’s home in Dubai to us, for a celebration of collaboration, innovation, and unwavering commitment to global health, provided a setting conducive to fostering meaningful collaboration and catalysing impactful change across the globe.
FROM December 4th, 2023
Healthy Futures on Health Day at COP28! In welcoming the first ever Health Day, taking place at COP 28 UAE, I was pleased to speak with Bill Anderson, CEO, Bayer, Dr Naveen Rao, SVP Health Initiative, Rockefeller Foundation and Dr Sally Uren, CEO, Forum for the Future on the Beyond 1.5°C: Challenges and Solutions in Protecting Human Health on a Warming Planet Panel, moderated by Claus Runge, Senior Vice President, Global Head of Market Access, Public Affairs & Sustainability at Bayer Pharmaceuticals, Bayer AG, hosted in the International Chamber of Commerce (ICC) Pavilion, Blue Zone. Projected rises in average temperature and in frequency, intensity and duration of heat waves will increasingly impact human health. Already today, on a planet still below the 1.5°C warming threshold, health consequences of the steady increase in temperature are devastating, with Africa counting between 12,000 and 19,000 heat-related child deaths per year. The strain heat places on our health carries various implications, as it can create cumulative physiological stress, exacerbating respiratory and cardiovascular diseases, while also deeply impacting women’s health, intensifying heat flashes during menopause or disrupting a woman’s reproduction cycle. It can also erode broader healthcare infrastructure through power outages as well as water scarcity, and similar to other dimensions of climate change, heat affects those most vulnerable, notably pregnant women, the elderly and children, ultimately exacerbating existing inequalities. As we head towards a warming trajectory beyond 1.5°C, our panel discussed how crucial it is to accelerate our efforts in protecting human health, through new approaches and accelerated collective action to data collection, policy implementation and the strengthening of locally-led heat resilient public health systems, encompassing equitable access to medicine, infrastructure and human capital, through a multi-stakeholder and public-private partnerships approach for effective action in heat and health.
FROM December 2nd, 2023
I was proud to join longstanding The Wellbeing Foundation Africa partners, Reckitt on their high-level roundtable to determine the next steps towards building equitable, sustainable, climate-resilient health systems and mobilise vital investment in the sector, held at Goals House, on the margins of COP28 UAE. Climate resilient health systems are the backbone of health equity, yet global health systems are under unprecedented strain. Progress towards health equity has stalled, with one in two people around the world still lacking access to basic healthcare. Coming together with a diverse group of health experts to explore how we can rethink healthcare delivery, I emphasised the need for investment in training more community health workers to adapt and mitigate the effects of climate change on the frontlines through behavioural change and climate literacy. Already one in four deaths are attributed to preventable environmental causes, with the World Health Organisation estimating at least 250,000 people will die each year due to climate change. The WorldBank estimates that up to 132 million people will fall into poverty by 2030 due to direct health impacts of climate change, and approximately 1.2 billion people will be displaced by 2050. As we mark the first ever Health Day at COP 28 today, we must be resolute in our determination to address the challenges posed to health by climate change and encourage ambitious investment in the health sector, to foster systems which can withstand the impact of climate change.
FROM December 2nd, 2023
On the occasion of COP 28, I was delighted to join the Reception on Building Partnerships to Deliver Climate Action in Cities, co-hosted by The King’s Foundation and Community Jameel at the Jameel Arts Centre in Dubai. Gathered with leaders working to build a collaborative response to climate action in cities, in the Commonwealth and beyond, the event resonated with inspiring objectives shared by Kris Murrin, CEO of The King’s Foundation, and George Richards, Director of Community Jameel. In conversation with Fady Jameel, Vice Chairman of Community Jameel, we shared our commitments in advancing science and learning for communities to thrive, and the importance of reducing poverty by ensuring that policy is informed by scientific evidence, research, outreach, and training. As we navigate the complex landscape of climate action, especially in cities, the exchange of ideas and the momentum created by such alliances are pivotal. I am invigorated by the dedication exhibited by all present, and I am inspired by the potential for impactful collaborations that transcend borders.
FROM December 1st, 2023
It was an honour to be invited by the COP28 UAE Presidency and the Sustainable Markets Initiative to join the reception to open the Business and Philanthropy Climate Forum in the presence of His Majesty King Charles III and His Highness Sheikh Mohamed bin Zayed Al Nahyan. Held concurrently with the heads of state-level World Climate Action Summit at the beginning of the two-week COP28 programme, the Business & Philanthropy Climate Forum #BPCF is COP28 UAE’s multi-stakeholder engagement platform for the Private Sector, dedicated to driving cross-sectoral advancements towards achieving net zero and nature-positive goals. This CEO high-level inclusive global gathering unites philanthropists and global business leaders, harnessing their dynamism, practical knowledge, wealth of resources, and capacity for delivering results to expedite climate and nature action. Together, we gathered and discussed the urgency to address our world's pressing climate challenges, while illuminating the crucial role of collaboration between nations, businesses, and philanthropic entities in forging a sustainable and resilient future for generations to come.
It was an honour to be invited by the COP28 UAE Presidency and the Sustainable Markets Initiative to join the reception to open the Business and Philanthropy Climate Forum in the presence of His Majesty King Charles III and His Highness Sheikh Mohamed bin Zayed Al Nahyan.
— Toyin Saraki (@ToyinSaraki) December 1, 2023
Held… pic.twitter.com/bJnWzUEtu7
FROM November 30th, 2023
During inclusive dialogue at the United Nations General Assembly 78, I was excited to discuss the future of development with my dear friend Matthew Swift, Co-Founder, Chairman, and CEO of the Concordia Summit, for The Swift Hour at Concordia 23! As a member of Concordia’s Leadership Council, I appreciated the platform for open dialogue, as we explored crucial topics, discussing global health, sustainable development, and empowering communities, especially through impactful partnerships. As the 2023 United Nations Climate Change Conference of Parties COP 28 begins today, I am especially proud to shed light on the mission of The Wellbeing Foundation Africa and its harmonisation with Africa’s foremost concerns, especially in the context of environmental conservation objectives and the intersection of CleanWater, Climate and Health. Watch the full interview:
FROM November 23rd, 2023
Abuja, Federal Capital Territory, November 23rd & 24th 2023 – The Nigeria Federal Ministry of Health and Social Welfare's Ministerial Roundtable on Mental Health marked a pivotal moment in Nigeria's journey toward mental health wellbeing under the theme "Achieving Universal Health Coverage For Mental Health In Nigeria; National Mental Health Act 2021 - from Act to Action." Convened by the Honourable Coordinating Minister of Health and Social Welfare, Professor Muhammad Ali Pate, and led by Dr Massey-Ferguson, National Coordinator, National Mental Health Programme, and the esteemed team at the Federal Ministry of Health, the roundtable garnered participation from a diverse array of national and imulti-lateral stakeholders and partners. During this landmark gathering, Her Excellency Toyin Saraki, Founder & President of the Wellbeing Foundation Africa reaffirmed in her Goodwill Statement, WBFAs steadfast dedication as a longstanding technical policy, advocacy, and planning partner. The Wellbeing Foundation Africa, which has developed and integrated Nigeria's Perinatal Mental Health Checklist within the National Primary Health Care Development Agency (NPHCDA) Maternal and Child Health MCH Handbook, values the shared commitment to improving access to primary, secondary and tertiary mental health and wellbeing services for all people in Nigeria, through the structured unification of national policy efforts towards achieving universal health coverage for mental health and encouragement of full implementation of the provisions of the National Mental Health Act of 2021. The Ministerial Roundtable witnessed the launch of crucial initiatives including the "National Mental Health Policy" and the "National Suicide Prevention Strategic Framework." Additionally, commendation was extended towards the resolution passed at the 64th regular session of the National Council on Health, endorsing the adoption and implementation of the National Suicide Prevention Strategic Framework across the 36 States of the Federation and FCT. Acknowledging the invaluable support of global health and development leaders and organisations, including the United Nations Deputy Secretary-General H.E. Amina J Mohammed, World Health Organization Director-General Dr Tedros Ghebreyesus, FIGO Director of Maternal and Neonatal Health Professor Bo Jacobsson, MOMENTUM Country and Global Leadership Program Director Dr Koki Agarwal of Jhpiego and USAID, and our Technical Working Group comprising representatives from UNICEF, UNFPA, Clinton Health Access Initiative, Johnson & Johnson, The Bill & Melinda Gates Foundation, among other policymakers, mental health practitioners, diplomatic community members, and development partners, underscores the collective effort toward Nigeria's pursuit of Sustainable Development Goals 3.4, 3.5, and 3.8. The urgency to revolutionise mental health care in Nigeria was highlighted, as Her Excellency Toyin Saraki remarked "That 1 in 4 Nigerians live with a mental health condition, with only 1 in 10 seeking and receiving adequate care. Robust policy implementation, frontline programming, and extensive awareness campaigns are essential to nurturing a society where mental wellbeing becomes a tangible reality for all.” The Wellbeing Foundation Africa extends its commitment to collaborating with stakeholders and supporting initiatives that advance mental health policies and holistic care practices, to reduce the prevalence of suicide and mental health conditions in the country. Together, with a shared vision, the goal is to pave the way for a mentally healthier Nigeria.
FROM November 17th, 2023
I was honoured to be invited by The Rt Hon Patricia Scotland KC, Secretary-General of The Commonwealth to speak at the Women Leaders Event - A Call for Action: Safeguarding the Wellbeing of Women and Children hosted at Marlborough House, ahead of the upcoming International Day for the Elimination of Violence Against Women, attended by Her Majesty, Queen Camilla. Joining champions such as Lady Dentaa Amoateng, MBE, HE Dr Fatima Maada Bio, First Lady Sierra Leone, HE Fatoumatta Bah-Barrow, First Lady The Gambia, HE Maryam Mwinyi, First Lady Zanzibar, HE Linda Rama, Spouse of the Prime Minister of Albania, Sarah Brown, Chair, Theirworld, Jane Randel, Founder NO MORE, Jude Kelly CBE, Founder The WOW Foundation, the event converged women leaders to examine the mental health and well-being of women and children. Erin Kenney, Director, Gender, Diversity, Equity, and Human Rights a.i. World Health Organisation, moderated the panel on Domestic Violence and Mental Health: Impact on Women and Children, including myself, Dr. Nabeel Goheer from PATH, Dr. Stephen Burrell from Durham University, Dr. Sharifa Al Emadi from Doha International Family Institute, and Cleopatra Christie from the Bahamas Crisis Centre. In my remarks I called upon this unique gathering of women leaders to ensure our targets include reaching the primary frontline tiers of universal basic education and universal health coverage, for the most vulnerable. According to WHO, one in four Nigerians, are living with a mental health disorder. I reflected on The Wellbeing Foundation Africa's frontline programmes supporting women and children's mental health, as WBFA midwives and school nurse-visitors, play crucial supporting roles as trusted community members, who witness the societal impact of domestic violence, recognizing it as a pervasive issue. Urgent action is needed to address this societal ill and align to achieve the United Nations Sustainable Development Goals.
FROM November 4th, 2023
I am incredibly honoured to receive the prestigious Private Sector Health Alliance of Nigeria's Global Health Advocate of the Year Award, at the PSHAN Alliance 2023 Annual Awards and Gala Night, held in Lagos, yesterday. I deeply appreciate this recognition, by the PSHAN Chair, Mr Aigboje Aig-Imoukhuede, the Distinguished Jury Members, all the inspirational nominees and award winners, and our national health contributing compatriots across Nigeria. I dedicate this wonderful award to the daily efforts of my amazing The Wellbeing Foundation Africa Teams across our frontlines in Nigeria and beyond, who work daily with unflinching dedication, to bring our advocacy into action, with transformative impact, embodying the decades-long unstintingly sustained charter of the Trustees and Governing Council of the WBFA. At the event dedicated to acknowledging the significant contributions of individuals, organisations, and institutions that have been instrumental in advancing healthcare and improving outcomes in Nigeria, I appreciate The Wellbeing Foundation Africa Lagos State Team for representing us, and I celebrate their nomination for Outstanding Philanthropy Award, which reflects our unwavering commitment to championing access to quality healthcare through #frontline programming across the Nation. I want to extend my deepest gratitude to all the voters who participated, and to PSHAN 2023 for their efforts and vision which align with our mission of creating a healthier and happier Nigeria.
FROM October 31st, 2023
I and the Wellbeing Foundation Africa Teams are thrilled to learn that we have been nominated in two separate categories of the Private Sector Health Alliance of Nigeria 2023 Awards! As we enter our 20th year of working for safer births for mothers and newborns, healthy nourished childhoods, clean water, sanitation and hygiene, and an upskilled health workforce, it is truly an honour to be recognised as being merited for outstanding contributions of remarkable individuals and organisations in the healthcare sector who have shown exceptional dedication, innovation, and a profound commitment to improving health and wellbeing. I congratulate all distinguished nominees in every category, as we all continue our dedicated contributions to the health and wellbeing of our amazing nation of Nigeria!
FROM October 26th, 2023
It was an honour to celebrate the academic excellence of Prof. Munir’deen Aderemi Ijaiya, a distinguished member of the University of Ilorin's Department of Obstetrics and Gynaecology. A dear friend to the Wellbeing Foundation Africa, it was a privilege to virtually witness on October 12th, the delivery of his lecture, "The Leaking Pipes as Avoidable Tragedy of Womanhood: The Odyssey of a Fistula Surgeon," during the 243rd Inaugural Lecture at this highly-respected and esteemed academic institution. Resonating perfectly with The Wellbeing Foundation Africa's mission, which is dedicated to enhancing the health and wellbeing of women and children in Africa, particularly focusing on maternal and newborn health, Prof. Ijaiya’s journey as a fistula surgeon sheds light on the challenges and successes in providing essential care and support to women during childbirth. Am exemplary individual whose relentless efforts have a significant impact on maternal and child health, #WBFA has witnessed Prof. Ijaiya's remarkable contributions to the success of our programming based on the vital role of accessible, high-quality healthcare services for pregnant women and newborns through Emergency Obstetric and Newborn Care and Neonatal Intensive Care Unit education. He has tirelessly worked to enhance the capacity and capability of healthcare professionals in this region, and under his leadership, the first #WBFA @LSTMNews CMNH EmONC Center of Excellence was established. This effort culminated in the creation of the second Center of Excellence and the first National Center of Excellence at the Kwara State College of Nursing and Midwifery, Ilorin, on May 31, 2022. Additionally, 12 localised clustered skills laboratories were established and donated by the programme at public health facilities across Kwara State. The WBFA takes pride in Professor Ijaiya's contributions to positioning Kwara State as a leading innovator in improving maternal and child survival and reducing birth injuries such as vesico-vaginal fistula #VVF in Nigeria. Kwara State is the first and only state to receive, lead, and successfully complete a whole-state global standard training program in EmONC. Prof. Ijaiya's dedication as a fistula surgeon and his involvement in the development of #EmONC and #NICU programmes have saved numerous lives, alleviated unnecessary suffering, and strengthened the healthcare system. The collaboration between The @WellbeingAfrica Foundation, Prof. Ijaiya, and the #UITH exemplifies the power of partnerships in advancing our shared mission of improving maternal and child health.
FROM October 24th, 2023
Welcoming A Cancer Shield for the People; A Monumental Step to Protect the Future Of 16.6 Million Nigerian Girls! Today on October 24th, Nigeria will embark on a historic journey, initiating a nationwide human papillomavirus HPV vaccination rollout and campaign. This marks a ground-breaking moment and the culmination of decades of dedicated multi-stakeholder advocacy efforts, as the vaccine is integrated into the national routine immunization schedule, and over the next three months, 16 of our 36 states will aim to immunize more than 7.1 million girls. By January 2024, the campaign will sweep across the entire nation, and by the end of 2025, Nigeria's goal is to have vaccinated 16.6 million girls aged nine to 14 against HPV, the virus responsible for nearly all Cervical Cancer cases, and which according to the World Health Organization, more than 10,000 Nigerian women die of each year. This marks the first time that the HPV vaccine will be offered free of charge to the people of Nigeria. Previously, it was only available through private clinics, at a cost of about $65 per dose, almost double the national minimum monthly wage. As all health facilities across Nigeria open their doors, offering the vaccine alongside other immunizations free of charge, as a long-term champion of Women Advocates for Vaccine Access, I have committed the Wellbeing Foundation Africa to promoting the factual dissemination of information which is vital in this endeavour. From educating on the cancer-preventing vaccine, to raising awareness in communities, WBFA is determined to protect our youth and eliminate cervical cancer from our future. I commend the Federal Ministry of Health and the National Primary Health Care Development Agency for their joint efforts with Gavi Alliance, UNICEF Nigeria, WHO Nigeria, and celebrate this milestone moment of Health For All. <blockquote class="instagram-media" data-instgrm-permalink="https://www.instagram.com/p/CyyR58So25d/?utm_source=ig_embed&utm_campaign=loading" data-instgrm-version="14" style=" background:#FFF; border:0; border-radius:3px; box-shadow:0 0 1px 0 rgba(0,0,0,0.5),0 1px 10px 0 rgba(0,0,0,0.15); margin: 1px; max-width:540px; min-width:326px; padding:0; width:99.375%; width:-webkit-calc(100% - 2px); width:calc(100% - 2px);"><div style="padding:16px;"> <a href="https://www.instagram.com/p/CyyR58So25d/?utm_source=ig_embed&utm_campaign=loading" style=" background:#FFFFFF; line-height:0; padding:0 0; text-align:center; text-decoration:none; width:100%;" target="_blank"> <div style=" display: flex; flex-direction: row; align-items: center;"> <div style="background-color: #F4F4F4; border-radius: 50%; flex-grow: 0; height: 40px; margin-right: 14px; width: 40px;"></div> <div style="display: flex; flex-direction: column; flex-grow: 1; justify-content: center;"> <div style=" background-color: #F4F4F4; border-radius: 4px; flex-grow: 0; height: 14px; margin-bottom: 6px; width: 100px;"></div> <div style=" background-color: #F4F4F4; border-radius: 4px; flex-grow: 0; height: 14px; width: 60px;"></div></div></div><div style="padding: 19% 0;"></div> <div style="display:block; height:50px; margin:0 auto 12px; width:50px;"><svg width="50px" height="50px" viewBox="0 0 60 60" version="1.1" xmlns="https://www.w3.org/2000/svg" xmlns:xlink="https://www.w3.org/1999/xlink"><g stroke="none" stroke-width="1" fill="none" fill-rule="evenodd"><g transform="translate(-511.000000, -20.000000)" fill="#000000"><g><path d="M556.869,30.41 C554.814,30.41 553.148,32.076 553.148,34.131 C553.148,36.186 554.814,37.852 556.869,37.852 C558.924,37.852 560.59,36.186 560.59,34.131 C560.59,32.076 558.924,30.41 556.869,30.41 M541,60.657 C535.114,60.657 530.342,55.887 530.342,50 C530.342,44.114 535.114,39.342 541,39.342 C546.887,39.342 551.658,44.114 551.658,50 C551.658,55.887 546.887,60.657 541,60.657 M541,33.886 C532.1,33.886 524.886,41.1 524.886,50 C524.886,58.899 532.1,66.113 541,66.113 C549.9,66.113 557.115,58.899 557.115,50 C557.115,41.1 549.9,33.886 541,33.886 M565.378,62.101 C565.244,65.022 564.756,66.606 564.346,67.663 C563.803,69.06 563.154,70.057 562.106,71.106 C561.058,72.155 560.06,72.803 558.662,73.347 C557.607,73.757 556.021,74.244 553.102,74.378 C549.944,74.521 548.997,74.552 541,74.552 C533.003,74.552 532.056,74.521 528.898,74.378 C525.979,74.244 524.393,73.757 523.338,73.347 C521.94,72.803 520.942,72.155 519.894,71.106 C518.846,70.057 518.197,69.06 517.654,67.663 C517.244,66.606 516.755,65.022 516.623,62.101 C516.479,58.943 516.448,57.996 516.448,50 C516.448,42.003 516.479,41.056 516.623,37.899 C516.755,34.978 517.244,33.391 517.654,32.338 C518.197,30.938 518.846,29.942 519.894,28.894 C520.942,27.846 521.94,27.196 523.338,26.654 C524.393,26.244 525.979,25.756 528.898,25.623 C532.057,25.479 533.004,25.448 541,25.448 C548.997,25.448 549.943,25.479 553.102,25.623 C556.021,25.756 557.607,26.244 558.662,26.654 C560.06,27.196 561.058,27.846 562.106,28.894 C563.154,29.942 563.803,30.938 564.346,32.338 C564.756,33.391 565.244,34.978 565.378,37.899 C565.522,41.056 565.552,42.003 565.552,50 C565.552,57.996 565.522,58.943 565.378,62.101 M570.82,37.631 C570.674,34.438 570.167,32.258 569.425,30.349 C568.659,28.377 567.633,26.702 565.965,25.035 C564.297,23.368 562.623,22.342 560.652,21.575 C558.743,20.834 556.562,20.326 553.369,20.18 C550.169,20.033 549.148,20 541,20 C532.853,20 531.831,20.033 528.631,20.18 C525.438,20.326 523.257,20.834 521.349,21.575 C519.376,22.342 517.703,23.368 516.035,25.035 C514.368,26.702 513.342,28.377 512.574,30.349 C511.834,32.258 511.326,34.438 511.181,37.631 C511.035,40.831 511,41.851 511,50 C511,58.147 511.035,59.17 511.181,62.369 C511.326,65.562 511.834,67.743 512.574,69.651 C513.342,71.625 514.368,73.296 516.035,74.965 C517.703,76.634 519.376,77.658 521.349,78.425 C523.257,79.167 525.438,79.673 528.631,79.82 C531.831,79.965 532.853,80.001 541,80.001 C549.148,80.001 550.169,79.965 553.369,79.82 C556.562,79.673 558.743,79.167 560.652,78.425 C562.623,77.658 564.297,76.634 565.965,74.965 C567.633,73.296 568.659,71.625 569.425,69.651 C570.167,67.743 570.674,65.562 570.82,62.369 C570.966,59.17 571,58.147 571,50 C571,41.851 570.966,40.831 570.82,37.631"></path></g></g></g></svg></div><div style="padding-top: 8px;"> <div style=" color:#3897f0; font-family:Arial,sans-serif; font-size:14px; font-style:normal; font-weight:550; line-height:18px;">View this post on Instagram</div></div><div style="padding: 12.5% 0;"></div> <div style="display: flex; flex-direction: row; margin-bottom: 14px; align-items: center;"><div> <div style="background-color: #F4F4F4; border-radius: 50%; height: 12.5px; width: 12.5px; transform: translateX(0px) translateY(7px);"></div> <div style="background-color: #F4F4F4; height: 12.5px; transform: rotate(-45deg) translateX(3px) translateY(1px); width: 12.5px; flex-grow: 0; margin-right: 14px; margin-left: 2px;"></div> <div style="background-color: #F4F4F4; border-radius: 50%; height: 12.5px; width: 12.5px; transform: translateX(9px) translateY(-18px);"></div></div><div style="margin-left: 8px;"> <div style=" background-color: #F4F4F4; border-radius: 50%; flex-grow: 0; height: 20px; width: 20px;"></div> <div style=" width: 0; height: 0; border-top: 2px solid transparent; border-left: 6px solid #f4f4f4; border-bottom: 2px solid transparent; transform: translateX(16px) translateY(-4px) rotate(30deg)"></div></div><div style="margin-left: auto;"> <div style=" width: 0px; border-top: 8px solid #F4F4F4; border-right: 8px solid transparent; transform: translateY(16px);"></div> <div style=" background-color: #F4F4F4; flex-grow: 0; height: 12px; width: 16px; transform: translateY(-4px);"></div> <div style=" width: 0; height: 0; border-top: 8px solid #F4F4F4; border-left: 8px solid transparent; transform: translateY(-4px) translateX(8px);"></div></div></div> <div style="display: flex; flex-direction: column; flex-grow: 1; justify-content: center; margin-bottom: 24px;"> <div style=" background-color: #F4F4F4; border-radius: 4px; flex-grow: 0; height: 14px; margin-bottom: 6px; width: 224px;"></div> <div style=" background-color: #F4F4F4; border-radius: 4px; flex-grow: 0; height: 14px; width: 144px;"></div></div></a><p style=" color:#c9c8cd; font-family:Arial,sans-serif; font-size:14px; line-height:17px; margin-bottom:0; margin-top:8px; overflow:hidden; padding:8px 0 7px; text-align:center; text-overflow:ellipsis; white-space:nowrap;"><a href="https://www.instagram.com/p/CyyR58So25d/?utm_source=ig_embed&utm_campaign=loading" style=" color:#c9c8cd; font-family:Arial,sans-serif; font-size:14px; font-style:normal; font-weight:normal; line-height:17px; text-decoration:none;" target="_blank">A post shared by Toyin Saraki (@toyinsaraki)</a></p></div></blockquote> <script async src="//www.instagram.com/embed.js"></script>
FROM October 21st, 2023
This week, I was honoured to join Prince's Trust International's Africa Advisory Board and business leaders for a discussion on opportunities for young people in Africa, attended by The Trust’s President and Founder His Majesty The King. Together we discussed the need to bridge the jobs, skills and experience gaps faced by young people in Africa.
PTIs 2023 Impact Report
[3d-flip-book id="2233" ][/3d-flip-book]
View this post on Instagram
FROM October 12th, 2023
How can improving farmer health and wellbeing enhance resilience? Last Friday, I was honoured to address the third annual OpenAg Symposium: Food Futures in a Changing Climate, held at the Saïd Business School at the University of Oxford. Organised and hosted by the Oxford India Centre for Sustainable Development and Somerville College Oxford, in partnership with UPL Global, one of the leading suppliers of sustainable agriculture products and solutions. With opening remarks by The Rt Hon Patricia Scotland KC, Commonwealth Secretary-General and a keynote address by Helen Browning OBE, the symposium engaged the meaning of resilience across agricultural stakeholders. Joining Dr. Shobhana Nagraj, Post-doctoral Clinical Researcher in the Health Systems Collaborative group at the NDM Centre for Global Health Research, Dr. Kate Lamont, Senior Lecturer in Veterinary & Animal Science at the Centre for Epidemiology & Planetary Health, and Duncan Williamson, Global Strategic Lead for Food Systems at Forum for the Future, our panel specifically focused on enhancing resilience to improve farmer health and wellbeing. Presenting to a diverse group of academia, policy, industry, and NGO leaders in the Rhodes Auditorium, I highlighted the inextricable link between climate change, poverty and health, we considered a whole-systems approach to improve farmer wellbeing, from climate-sensitive health risks, their exposure pathways, and vulnerability factors, to the importance of enhancing the adaptive capacity and resilience of health and agricultural systems. Looking ahead to COP28 and Health Day, it is vital to explore the context-specific needs and priorities of rural communities, and interventions which will deliver lasting change in agriculture, with an examination of how policy reform can promote resilient, sustainable farming, alongside farmer and societal welfare. I deeply appreciate Mr. Jai Shroff, Chairman & Group CEO of UPL, Mr. Vikram Shroff, Vice-Chairman & Co-CEO of UPL, and Baroness Royall of Blaisdon, Principal of Somerville College, for their kind invitation; Farmer health and resilience are the roots of a flourishing future!
FROM October 11th, 2023
Investing In Girls' Rights, Leadership, and Wellbeing! On this International Day of the Girl, I join the global celebration of the rights and empowerment of girls and young women, as #DayOfTheGirl serves as a reminder of the incredible potential that girls hold as change agents, driving progress toward gender equity, opportunity, and equality. In particular, I am thrilled to highlight the significant impact of the Wellbeing Foundation Africa's Personal Social and Health Education Skills PSHE-WASH programming, which is actively working to close the gender gap within educational settings, with remarkable improvement in girls' participation and successful completion of our PSHE-WASH offerings. The remarkable results of the concluded Phase 1 programming reached the lives of 9,321 children in 96 schools, and I am delighted to share that Phase 2 is set to achieve even greater scale, targeting 248,000 children across 620 schools, aiming to meet the urgent need for increased attention and resources in the critical areas that empower girls to realise their rights and reach their full potential. The Wellbeing Foundation Africa's PSHE-WASH programs, generously supported by Reckitt, stand as a testament to our commitment to respond to girls' calls for change. WBFA recognises that it is imperative for the global community to move beyond mere reaffirmations of commitments and invest boldly in the actions required to bring about real change. It is heartening to witness the proactive involvement of many girls who are already championing solutions and driving positive change in their communities. Together with our government and private sector partners, #WBFA envisions a world where girls have the agency to shape government policies and spending, inform the rules and norms by which businesses operate, and direct the priorities for new research and innovations. This vision is not an isolated example but rather the norm we aim to establish. To discover resources that can contribute to improving gender equality and empowering the rise of every woman and girl, we invite you to explore the WBFA's #WGGDT (Women, Girls, and Gender Development Targets) below. Together, let's continue to support and uplift girls everywhere, ensuring they have the opportunities and support needed to make a difference in the world.
Women, Girls, and Gender Development Targets: Making Women a Priority
The Foundation acknowledges the fundamental necessity of gender equality and the empowerment of all women and girls. Throughout our multi-layered strategy of research, advocacy, policy development, community engagement, philanthropy and education, we have prioritized women, adolescent girls, and children within our various programs mainly focusing on maternal and infant health, as well as sexual, reproductive, mental, and social health in order to empower and strengthen girls and women from birth to old age.
This policy document is guided by items 1-5 of the Girl Declaration; 1-10 of the G7 Recommendations for Action from the Gender Equality Advisory Council (2019)4; and 2, 3, 4, 7, 9 10 and 11 of the Nairobi Statement on ICPD25: Accelerating the Promise.
Through this policy, WBFA commits to the following goals:
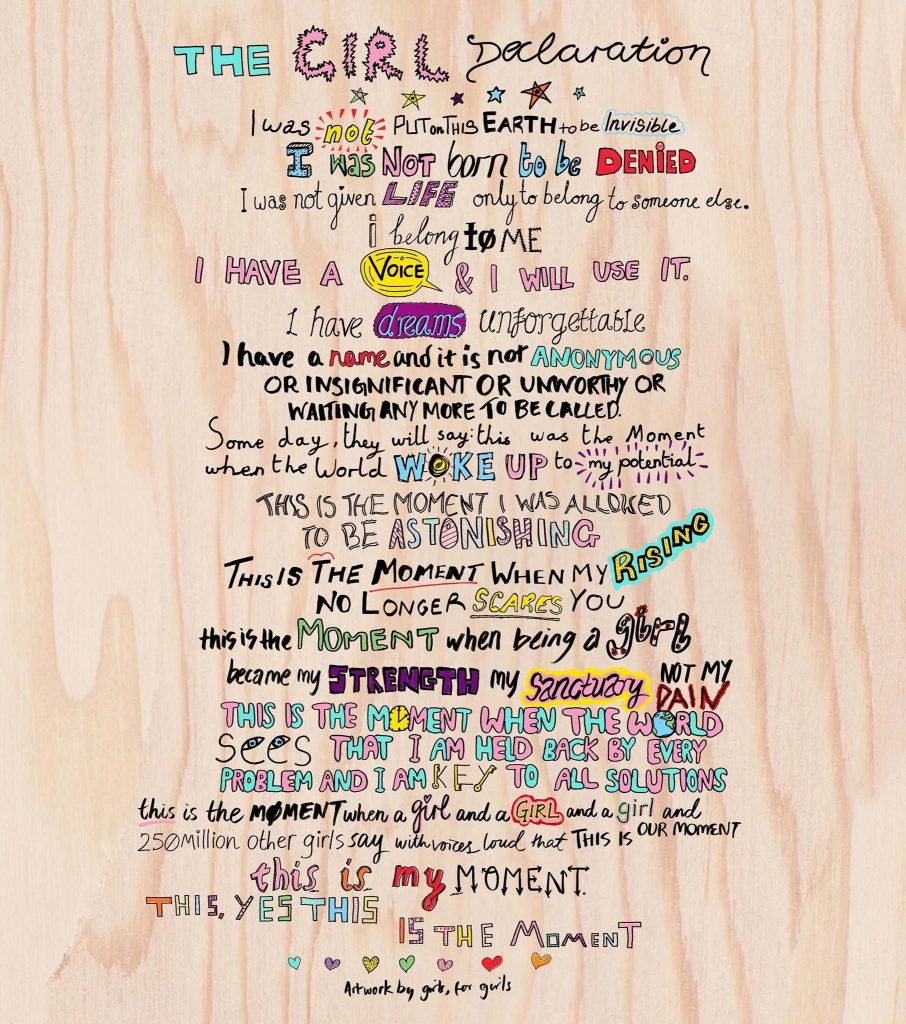
FROM October 4th, 2023
Congratulations to Her Highness Sheikha Shamma bint Sultan bin Khalifa Al Nahyan, a truly determined young woman, for her visionary commitment to the vital advocacy and action of The Climate Tribe. I spent a truly engaging evening with Her Highness Sheikha Shamma bint Sultan bin Khalifa Al Nahyan at the launch of The Climate Tribe, which she has founded as a UAE-based social enterprise dedicated to inspiring climate action through dynamic storytelling, immersive community engagement, and radical collaboration, at Goals House in New York City, on the sidelines of the United Nations General Assembly and Climate Week NYC 2023. Bridging the local and the global, we were joined by industry leaders, entrepreneurs, creatives and climate advocates at the dinner co-hosted by DP World, Global Impact Partner for the initiative. Her Highness shared how The Climate Tribe aims to highlight the journeys and achievements of changemakers, innovators and philanthropists from around the world to galvanise communities in the UAE, while shining a light on the inherent sustainable practices, ecological heritage and natural wonders of the Middle East. Especially ahead of COP28, which is set to take place from 30 November until 12 December 2023, at the Expo City, Dubai, I look forward to witnessing the impact which will stem from The Climate Tribe as we tackle the borderless challenge of climate change and equitable health.
FROM October 3rd, 2023
Yesterday truly marked a great day for health, a great day for scientific advancement and a great day for the cause of vaccines! I am hugely encouraged by the announcement from Director-General Dr Tedros Adhanom Ghebreyesus and the esteemed World Health Organization - WHO, regarding the recommendation of a second vaccine, named R21/Matrix-M, aimed at preventing malaria in children at risk of contracting this debilitating disease. Given the overwhelming demand for the RTS, S vaccine, the introduction of the R21 vaccine stands as a pivotal addition, enabling us to safeguard a larger number of children at a swifter pace. This, in conjunction with the deployment of insecticide-treated nets (ITNs) and various environmental interventions, signifies a substantial stride towards realising our vision to End Malaria and inching closer to a world free from the scourge of malaria. During the United Nations General Assembly (UNGA78), I also took the opportunity to wish the World Health Organization a productive 75th birthday, as we converged with Dr Tedros, Reckitt and WHO Climate & Health Special Envoy Dr Vanessa B Kerry at the Goals House, working together for The Road to COP28 under the committed leadership of the United Arab Emirates 🇦🇪 H.E. Sultan Al Jaber, towards the First-Ever Health Day: Advancing a Bold Vision For Action, Equity & Accountability. I commend Dr Tedros on the historic UN declaration approved by World Leaders on Pandemic Prevention, Preparedness and Response. The United Nations Member States have demonstrated that even at this time of division and polarisation, it’s still possible for countries to come together to agree on a shared response to shared threats. My unwavering commitments to the WHO continue in my role as a Special Adviser to the World Health Organisation Africa Region (WHOAFRO) and in my efforts to champion the endeavours and impact of the WHO Foundation, where I serve as the Inaugural Global Health Ambassador. It is abundantly clear that we have no future but a shared future, and a better future for global health and wellbeing actions!
FROM September 28th, 2023
Ensuring Safer Births for Women and Newborns - Everywhere I was grateful to be the Guest of Honour at the Maternity Foundation Denamark’s high-level reception during the week of United Nations General Assembly 78, celebrating their launch in the United States. Joining my long-time fellow Maternal, Newborn and Child Health advocates and midwife champions, Anna Frellsen, CEO and Dr. Franka Cadée, Director of Global Initiatives, Maternity Foundation, I praised their innovative mobile health solutions, including the Safe Delivery App, which the Wellbeing Foundation Africa midwives are utilizing to access direct and instant evidence-based and up-to-date clinical guidelines, to support their everyday work. Maternal health is a fundamental human rights issue. The launch of Maternity Foundation Inc. in the United States marks a significant milestone, especially in advocating and acting for the care of women of Black, Asian and Minority Ethnicities - BAME. We cannot rest until every woman, regardless of her background or circumstances, has access to safe and high-quality maternal healthcare. I look forward to further collaborating with the Maternity Foundation, and their digital solutions, and learning programmes, to continue to build midwifery knowledge and skills, and work to end preventable maternal morbidity and harm. “When women thrive, all of society benefits, and succeeding generations are given a better start in life.” - Kofi Annan, Former Secretary-General of the United Nations.
FROM September 26th, 2023
ICPD30: Celebrating Milestones, Inspiring Action at United Nations General Assembly 78 As a member of the ICPD25 International Steering Committee, I was honoured to join UNFPA Leaders at the Ministerial Briefing on #ICPD25 at the UN Headquarters, ahead of the thirtieth anniversary of the ICPD in 2024 ICPD30, to build momentum for the review of implementation on the margins of the 78th High-Level Week of the United Nations General Assembly in New York. Co-hosted by the Governments of Bulgaria and Sweden, and with remarks delivered by Dr. Natalia Kanem, UNFPA Executive Director, H.E. Mariya Gabriel the Deputy Prime Minister of Bulgaria and Minister of Foreign Affairs, Johan Forssell, Minister for International Development Cooperation and Foreign Trade of Sweden, and Ms. Diene Keita, UNFPA Deputy Executive Director-Programme, we discussed what is at stake, to explore ways to participate in the review process and mobilise support for the ICPD Agenda, as we must remain ever vigilant against backtracking, and insistent on progress. Shortly after, the High-Level Commission on the Nairobi Summit on ICPD25 Follow-up concluded its work by launching a report championing a universal, unifying call for sexual and reproductive justice. ‘Sexual and Reproductive Justice Cannot Wait: All Rights, All People, Acting Now’ published on Friday, is the commission’s final report, urging diverse movements for justice, including those advocating for youth, gender equality and climate, to join forces in driving the changes needed around the world. Outlining the path forward, to meet the 12 core Nairobi commitments and achieve three transformative zeros: zero unmet need for contraception, zero preventable maternal deaths, and zero gender-based violence and harmful practices, we must prioritise the power and safety of the 1.8 billion youth 1point8billion Partnership for Maternal, Newborn & Child Health, and ensure sustainable investment in Adolescent and Youth Sexual and Reproductive Health and Rights Services. The Wellbeing Foundation Africa believes that when adolescents successfully transition into adulthood healthily, it broadens the range of opportunities for their future, and their communities. Together, we must ensure they realise their rights and choices.
FROM September 25th, 2023
Embracing the Power of Youth and Unity at the 78th United Nations General Assembly! It has been an incredible experience at the 78th United Nations General Assembly, where aside from the high-level meetings with dignitaries, I also had the privilege of meeting, listening to, and connecting with numerous remarkable youth from Nigeria and across our beautiful continent of Africa. The energy, passion, and determination of these young individuals have left an indelible mark on my heart and ignited a renewed sense of purpose. During our interactions, we discussed a myriad of pressing global issues, ranging from sustainable development goals to gender equality, healthcare access, climate change, and much more. Their depth of understanding and unwavering dedication to these causes are nothing short of inspiring. Their voices are not just heard, they resonate with clarity and conviction, echoing the aspirations of a brighter, more equitable future for all. One of the most humbling yet heartening aspects of our encounters was how these young leaders recounted how they had drawn spontaneous inspiration from the work of the Wellbeing Foundation Africa. Today the world has 1.8 billion youth aged 10 - 24, more young people than at any time in history, who will need improved Policies and investments to meet their needs; a key focal theme of the WHO PMNCH 1.8 Billion Young People For Change Campaign asking young people what they want for their health and wellbeing, and building demand for decision makers to transform their answers into policies, investments and actions from world leaders. I look forward to continuing to foster these connections, nurture their ambitions, and encourage the support and resources to bring their visions to fruition.
FROM September 24th, 2023
Fostering Community Wellbeing: Learning from Qatar's Healthcare Excellence I was honoured to reconnect with a very dear sister, mentor and ally, Her Excellency Dr. Hanan Al Kuwari, the Minister of Public Health of Qatar, at the Permanent Mission of the State of Qatar to the @UnitedNations in New York. Dr. Hanan's exceptional leadership, both in the Ministry of Public Health Qatar and as Chair of the World Health Organization - WHO Executive Board, has been significantly instrumental in advancing global health. Qatar has set a remarkable example in building a world-class healthcare system, and I am deeply impressed by their commitment to quality and excellence for all. Their investment in healthcare worker's training and their dedication to creating a nation of wellbeing is truly commendable. As we continue our mission at the Wellbeing Foundation Africa to improve healthcare in Nigeria and beyond, there is much we can learn from Qatar's incredible achievements. We look forward to exploring opportunities for collaboration and replenishing knowledge exchange to enhance the standard of care and enhance the standard of living for our communities. Thank you, Dr. Hanan, for your inspiring work and for paving the way for healthier futures.
FROM September 24th, 2023
Unlocking Hope: Advancing Universal Health Coverage with a Focus on Breast Cancer Collaboration in Africa I was pleased to join the Business Council for International Understanding #BCIU in partnership with Roche, as a roundtable participant in support of the United Nations High-Level Meeting on Universal Health Coverage on the margins of the Seventy-Eighth Session of the United Nations General Assembly. “Women-Centered Care: Combating the Breast Cancer Burden in Africa (Investment in Noncommunicable diseases – Universal Health Coverage)”, featured 30 stakeholders from multilateral organisations, development groups, civil society, NGOs, and global governments, focused on how to further advance the Non-Communicable Diseases Presidential Group’s vision and how the resolutions made by Heads of State at the High-Level Meeting on Universal Health Coverage can approach breast cancer initiatives as credible demonstrations of Noncommunicable diseases integration into Universal health coverage. In discussions with Roche, International Finance Corporation and World Bank Group, we recognised our joint vision of expanding coverage and affordability of quality health services throughout Africa, with public-private partnerships and health financing strategies aimed at strengthening healthcare worker's training and timely screening and care for breast cancer, combating the statistic that in Africa, 1 in 2 women die five years after receiving a breast cancer diagnosis. The Wellbeing Foundation Africa is committed to driving the learnings highlighted in our 2018 ground-breaking WBFA, Amref Health Africa and Takeda Oncology ‘Rapid Assessment of the Prevention and Control of Cancer in Nigeria’ report, the first independent national research on cancer provisions in the country, which found that Nigeria has a severe shortage of health personnel for cancer care, a dearth of specialists in particular in rural communities and a lack of a well-coordinated chain of supply of drugs and the requisite infrastructure. Together, we hope to improve the standard of care through the broader context of women’s health, as it has the potential to improve survival rates to 80%-90%, and accelerate progress to Universal health coverage.
FROM September 23rd, 2023
Impactful and Sustainable Investment in Africa to Achieve the 2030 Agenda! I appreciate the Milken Institute and African Philanthropy Forum's invitation to address influential philanthropists, funders, and foundations, fostering dialogue and cooperation to make a tangible impact on the world's most pressing issues. "The Unique Role of Philanthropy in Tackling the SDGs," delved into the immense potential of philanthropy in advancing the United Nations’ Sustainable Development Goals. The session explored how initiatives at the nexus of health, education, socio-economic empowerment, and community livelihoods, as well as partnerships and systemic thinking, can contribute to achieving these goals. In sharing my frontline insight on growing The Wellbeing Foundation Africa from a passion-borne initiative to a structured glocal institution, I espouse my views that philanthropy is uniquely suited to address deeply entrenched global challenges while partnership networks and collaboration in the philanthropic space are essential components of a shared journey towards a sustainable future. Recognising that the future of our world lies in Sub-Saharan Africa, where the birth rates are the highest across the globe, I found a like-mind in the hugely visionary Milken Institute Chairman, Mr Michael Milken, who also emphasised that to create transformative philanthropic impact, Africa must be included, during his address at this welcomed the African Philanthropy Forum and Milken institute event hosted on the sidelines of the United Nations General Assembly 78.
FROM September 22nd, 2023
Unlocking Global Prosperity: A Call to Action for Sustainable Supply Chains Good Trade Summit 2023 I was honoured to address the Good Trade Summit 2023 hosted by the Business Council for International Understanding and International Trade Centre, where global cooperation, sustainability, and policy's role in shaping sustainable supply chains took centre stage. Achieving Sustainable Development Goals, especially in health action, demands global cooperation and private-sector engagement. This is crucial in Nigeria, where sustainable supply chains impact livelihoods and economic development. International Trade Centre's 'Unified Strength, Collective Impact' is a catalyst for positive change, promoting empowerment, collaboration, and digital transparency across global value chains. Empowering businesses to drive the Sustainable Development Goals agenda, amplifying small businesses' voices, and encouraging women and youth innovation to contribute to value chains are key steps, with the government and the private sector supporting through microfinancing, mentorship, and sponsorship, fuelling economic growth SDG8.
FROM September 22nd, 2023
Transformational Action in Water During United Nations General Assembly 78 and the United Nations Climate Week. I was thrilled to be a panellist on Transformational Action in Water, hosted by Reckitt at Goals House, alongside Water Action Global Leaders, Henk Ovink, Former Dutch Special Envoy on Water, Matt Damon, Co-Founder Water.org & Water Equity, Vedika Bhandarkar, COO, Water.org, Joel Kolker, Water and Finance Lead, World Bank, and moderated by my dear friend and #WASH partner, Patty O’Hayer, Global Head Communications & Government Affairs at Reckitt. I shared evidenced knowledge and evaluated learnings from the Wellbeing Foundation Africa and Dettol Nigeria Hygiene Quest programme which is leading our Clean Naija commitments to teaching proper handwash hygiene habits and reducing open defecation, sepsis, trachoma and diarrheal disease burdens across schools, households and health care facilities for the betterment of communities. Through transformative action, the Wellbeing Foundation Africa and Dettol Nigeria Hygiene Quest goes beyond the basics, encompassing the creation of a holistic ecosystem that promotes health, hygiene, and intergenerational development through our Sanitation Angels in schools, hospitals and communities. I particularly appreciated the opportunity to collaborate in knowledge sharing with this gathering of minds from the public, private, and third sectors, all dedicated to fostering collaboration in the water sector; indeed a testament which will further our Nigeria activation of shared commitments to achieving the United Nations Sustainable Development Goals 6 and 3 and ensuring access to clean water and sanitation for all.
FROM September 22nd, 2023
Business Fights Poverty: Catalysing Female Entrepreneurship I was honoured to serve as Moderator for the WiNFUND NFT Catalysing Female Entrepreneurship, taking place at this year’s Business Fight Poverty Global Goals Summit, a critical gathering focused on re-energising business partnerships for a more equitable and resilient future. The inspiring opening remarks from Zahid Torres Rehman, CEO, Business Fights Poverty, and insightful contributions of Patty O'Hayer, Global Head Government Affairs & Co-Founder of WiNFund, Reckitt, Corinne Hart, Senior Gender Advisor and Team Lead, Energy, Environment and Climate, USAID, Corinne Momal-Vanian, Executive Director, Kofi Annan Foundation, Pradeep Kakkattill, Founder, HIEX and Co-Founder, WiNFUND served to powerfully validate the importance of economically empowering gender-centred investments towards Sustainable Development Goals 5, 8, 10 and 17. Joined virtually by the pioneer cohort of WiNFUND Entrepreneur Winners, Dr. Shamim Nabuuma Kaliisa, CEO & Co-Founder, Chil Femtech Center Inc, Belinda Shaw, Chair & Founder, Cape Biologix, Adeola Ayoola, CEO & Co-Founder, Famasi Africa, Dr. Mercy Ashaba, CEO & Co-Founder, Peleyta Health, Judith Oketch, CEO & Founder, Ambulex Solutions Ltd, and Olivia Koburongo, Director Quality & Operations, MamaOpe Medicals, the session was a remarkable moment and platform to hear directly from those at the forefront of the innovation ecosystem, and share valuable insights in scaling women-led innovators for planetary, societal, and economic impact. At this one year milestone since the WiN Fund's launch at the United Nations General Assembly 2022, it's hugely encouraging that the WiNFUND has received over 300 applications from 7 countries across Africa, and it was a great pleasure to congratulate its six African female entrepreneurs who are making groundbreaking strides with their innovative start-ups, saving lives in their communities and beyond. In the shared belief in the power of collaboration to fight poverty, drive equity and build resilience, the Business Fights Poverty 2023 Global Summit was hosted on the sidelines of the United Nations General Assembly 78 at the New York headquarters of Barclays Bank.
FROM September 21st, 2023
Goalkeepers Accelerating Progress Towards SDG’s Agenda 2030 Ahead of the Goalkeepers events on the sidelines of the United Nations General Assembly, it was a pleasure to unite with longstanding allies, our Bill & Melinda Gates Foundation global colleagues during our thoughtful bilateral meeting with Dr. Rasa Izadnegahdar, who leads the Maternal, Newborn, Child Health Discovery and Tools portfolio within the Gender Equality Division, and Dr. Sanjana Bhardwaj, who leads Policy and Advocacy work related to family planning, maternal, newborn, and child health, nutrition, and primary health care systems. With decades of collaboratively impactful programming implemented through BMGF support, most notably the Wellbeing Foundation Africa and partners Alive and Thrive Maternal Infant and Young Child Feeding project in Lagos and Kaduna States, and because further progress is possible, but not inevitable, I commend and appreciate the Bill & Melinda Gates Foundation's strategy of continued investment in building capacity of frontline midwifery and nursing, to deliver health and wellbeing Sustainable Development Goal 3. Currently, across the world, approximately 800 women a day still die in childbirth. This means that the day a woman gives birth is the day she is most likely to die. I was inspired at the opening of Goalkeepers 2030, by all the winners of the Goalkeepers Global Goals Campaign Award, and the highlighting of new innovations that can save nearly 2 million more mothers and babies by 2030. Goalkeepers is dedicated to accelerating progress toward the United Nations Sustainable Development Goals Agenda 2030, through using powerful stories and data. Through driven partnership, we can aim to create a better 2030, by the numbers.
FROM September 20th, 2023
Genuine and Trusted Thought Leadership at the Annual Concordia Summit 2023 As a Concordia Summit Leadership Council Member, I was honoured to join council members and welcome our newest member, H.R.H. Prince Abdulaziz Bin Talal Bin Abdulaziz Al Saud, Chairman of the Arab Gulf Programme for Development. Alongside H.E. Madame Monica Geingos, First Lady of the Republic of Namibia, Cherie Blair CBE, KC, Former UK First Lady and Co-Founder & Chair of Omnia Strategy LLP, H.E. José Barroso, Chair of Gavi, the Vaccine Alliance and other incredible members comprised of former heads of state, leaders of industry, and policy experts, we contribute our practical experience at every level of government and business. Offering strategic guidance in expanding the Concordia community, and advising programming, ahead of the opening of Concordia Summit 2023 on the margins of the United Nations General Assembly 78, I look forward to the continuing impactful programming and growth of this trusted convening.
FROM September 20th, 2023
I was deeply privileged to join the Solve MIT Challenge Finals 2023 as the opening panellist on a day of unparalleled live pitches, bringing together global investors, philanthropists and other cross-sector leaders who are making transformational impacts across the world, on the margins of UN General Assembly 78. Having been an MIT Solve Challenge Judge for several years, I commended this program for unearthing the best solutions to specific, actionable challenges, through open innovation, and convening a community of change-makers, as I conversed with Cythia Barnhart, Provost, MIT, Sarah Chandler, VP of Environment & Supply Chain Innovation, Apple, Ilan Goldfajn, President, IDB, Hala Hanna, Executive Director, Solve, Moderator Lysa John, Secretary-General, CIVICUS, Johanna Mair, Academic Editor, Stanford Social Innovation Review, Neela Montgomery, Board Partner, Greycroft, Emilian Popa, CEO, Ilara Health 2 solve.mit.edu, and David Sengeh, Chief Minister, Sierra Leone, to support the best possible solutions in health, sustainability, learning, and economic prosperity. A rise in technology-enabled and locally-led solutions is critical for progress on development, the health and climate crisis, and a better future for all.
FROM September 19th, 2023
The Global Goal of Equitable and Inclusive Quality Education for Every Child and Young Person by 2030 I was delighted to join supporters of global education at the TheirWorld and Global Business Coalition for Education dinner, hosted by Rt Hon Gordon Brown, United Nations Secretary-General’s Special Envoy for Global Education, WHO Ambassador for Global Health Financing and Former Prime Minister of the United Kingdom, Sarah Brown, Chair of Theirworld, Executive Chair of the Global Business Coalition for Education, and Roger Federer, Founder and President of the Board Roger Federer Foundation, to mark the United Nations 2023 Sustainable Development Goals Summit and the halfway point to achieving SDG 4 on the occasion of United Nations General Assembly 78. It was essential to discuss ending the global education crisis and unleashing the potential of future generations, through ensuring all young people have the best start in life, a safe place to learn, and skills for the future. Joined by Her Excellency Mia Mottley, Prime Minister of Barbados, Dr Ngozi Okonjo-Iweala, Director General of the World Trade Organization, Rt Hon Andrew Mitchell, MP, Minister of State in the Foreign, Commonwealth & Development Office, United Kingdom and other esteemed global leaders, it is with unwavering dedication and collaboration, we can achieve #SDG4 and provide boundless equitably for our children through learning.
FROM September 19th, 2023
Yesterday I joined the Representatives of H.E. William Ruto, President of Kenya and H.E. Alain Berset, President of Switzerland, H.E. Amina J. Mohammed, UN Deputy Secretary-General, Mr. Roger Federer, former Professional Tennis Player and Founder and Board President of the Roger Federer Foundation, Ms. Laura Frigenti, CEO, GPE, Ms. Catherine Russell, ED, UNICEF and Ms. Temilade Salami, The Global Partnership for Education Youth Leader, in addressing the Investing in Education Systems for Sustainable Development and Children’s Wellbeing panel, a high-Level event at the UN Headquarters during United Nations General Assembly 78 co-hosted by The Global Partnership for Education, The Roger Federer Foundation, The Government of Kenya, UNICEF and co-sponsored by the Government of Switzerland. Coming together with global influencers and champions from UN Member States, other UN multilateral bodies, civil society, foundations, and youth movements, we discussed the need to increase political will to drive progress towards #SDG4 through crucial investments in education systems and collaborative efforts across sectors and stakeholders. Thank you to Global Partnership for Education and UNICEF for Education, for this timely platform to discuss how investing in children’s wellbeing through education is an equalizer and the way forward to transform society through attaining all other United Nations.
FROM September 18th, 2023
I have commenced engagements at the 78th United Nations General Assembly High-Level Week alongside The Wellbeing Foundation Africa Global Delegation, informed and inspired by this year's United Nations General Assembly 2023 theme, rebuilding trust and reigniting global solidarity. During the Sustainable Development Goal Action Weekend at UN headquarters, I was pleased to be accompanied by data partners Hologic as I participated in the UN Women 2023 Generation Equality Midpoint event, to encourage the mobilisation of sustained attention to, and investment in, gender equality. In light of the concerning stagnation and regression observed in over 30% of the SDG targets, it becomes imperative that we forge partnerships with a wide array of stakeholders, including government entities, civil society organisations, youth associations, philanthropic foundations, and the private sector, as this shared responsibility is pivotal to our collective progress.
FROM August 21st, 2023
As we convene this week for World Water Week 2023 in Stockholm and virtually, the theme "Seeds of Change" aptly encapsulates the innovative solutions sprouting on the horizon of water conservation and management.
In the face of mounting water scarcity and the challenges posed by climate change, the world has increasingly recognized the urgency of safeguarding our most precious resource - water. I recall the journey towards a water-wise world, in particular when I engaged in 2019 with the Stockholm International Water Institute, discussing the challenges that frontline health workers face without access to water, sanitation and hygiene, and pledged through the Wellbeing Foundation Africa, to their water commitments, which laid the groundwork for activating the intersects between climate and health for our foundational transformative water, sanitation and hygiene change programming.

 In the years since World Water Week 2019, remarkable strides have been made, propelled by the Wellbeing Foundation Africa's WASH For Wellbeing Strategy, frontline programming, global advocacy efforts, and the evolution of water policies and commitments at the national level, exemplified by Nigeria's approach of emphasising sanitation, through the Federal Government’s 2018 Clean Naija Initiative supported by multi-sector CSR and CSO partners, and the highly welcomed Presidential decision to revise the nomenclature and responsibilities of the Federal Ministry of Water Resources to integrate and activate - “and Sanitation”.
The 2019 Stockholm International Water Institute commitments, and collective action since, through promotion of the United Nations and World Health Organization Resolution 64/292 which recognises the human right to water and sanitation, and acknowledges that clean water and sanitation are essential to the realisation of equitable human health, marked a turning point in addressing global water challenges. These commitments highlighted the necessity of collective action and innovation to ensure water security for all. The global community acknowledged the need to explore innovative solutions that extend beyond traditional water management methods. This paved the way for a wave of initiatives, collaborations, and policies aimed at nurturing a sustainable relationship with water.
In the years since World Water Week 2019, remarkable strides have been made, propelled by the Wellbeing Foundation Africa's WASH For Wellbeing Strategy, frontline programming, global advocacy efforts, and the evolution of water policies and commitments at the national level, exemplified by Nigeria's approach of emphasising sanitation, through the Federal Government’s 2018 Clean Naija Initiative supported by multi-sector CSR and CSO partners, and the highly welcomed Presidential decision to revise the nomenclature and responsibilities of the Federal Ministry of Water Resources to integrate and activate - “and Sanitation”.
The 2019 Stockholm International Water Institute commitments, and collective action since, through promotion of the United Nations and World Health Organization Resolution 64/292 which recognises the human right to water and sanitation, and acknowledges that clean water and sanitation are essential to the realisation of equitable human health, marked a turning point in addressing global water challenges. These commitments highlighted the necessity of collective action and innovation to ensure water security for all. The global community acknowledged the need to explore innovative solutions that extend beyond traditional water management methods. This paved the way for a wave of initiatives, collaborations, and policies aimed at nurturing a sustainable relationship with water.

 The Wellbeing Foundation Africa has since actualised its commitments, emerging as a premier thematic non-state grassroots and on the ground implementer of #WASH and wellbeing. The foundation's comprehensive approach through the Primary and Adolescent PSHE WASH and WBFA Dettol Nigeria Hygiene Quest programming, combining education, community engagement, and sustainable infrastructure, has led to tangible impact in water access and hygiene practices for over 43,194 mothers, schoolchildren and community members in 96 schools and 96 communities and a further 35 health care facilities with a clustered saturation model of beneficial change.
By empowering local communities to become stewards of their water resources, WBFA’s innovative practice sows the seeds of change at the fundamental level. Characterised by our proliferation of escalating impactful water, sanitation and hygiene education, and integrating the reduction of open defecation and fighting malaria through control of vector borne transmission through improved sanitation management of drainage water resources, the holistic elevation of communal wellbeing drives positive behavioural and social change intergenerationally, and works towards achieving key targets, highlighting the tangible outcomes of this dynamic cross-sector seeds for action now, towards the 2030 goals, specifically Goal 3: ensure healthy lives and promote well-being for all at all ages, and Goal 6: ensure access to water and sanitation for all.
The Wellbeing Foundation Africa has since actualised its commitments, emerging as a premier thematic non-state grassroots and on the ground implementer of #WASH and wellbeing. The foundation's comprehensive approach through the Primary and Adolescent PSHE WASH and WBFA Dettol Nigeria Hygiene Quest programming, combining education, community engagement, and sustainable infrastructure, has led to tangible impact in water access and hygiene practices for over 43,194 mothers, schoolchildren and community members in 96 schools and 96 communities and a further 35 health care facilities with a clustered saturation model of beneficial change.
By empowering local communities to become stewards of their water resources, WBFA’s innovative practice sows the seeds of change at the fundamental level. Characterised by our proliferation of escalating impactful water, sanitation and hygiene education, and integrating the reduction of open defecation and fighting malaria through control of vector borne transmission through improved sanitation management of drainage water resources, the holistic elevation of communal wellbeing drives positive behavioural and social change intergenerationally, and works towards achieving key targets, highlighting the tangible outcomes of this dynamic cross-sector seeds for action now, towards the 2030 goals, specifically Goal 3: ensure healthy lives and promote well-being for all at all ages, and Goal 6: ensure access to water and sanitation for all.
 Nigeria's journey towards water resilience from the 2018 declaration of a State Of Emergency in water, sanitation and hygiene, to the 2023 focus on water resources for effective sanitation, demonstrates the transformative power of national policies. Recognizing the interplay between water, health, and development, Nigeria has now set its feet and hands on the path and pipes of pursuing practical and innovative approaches to water management, especially through the inclusion of sanitation. By integrating traditional and cultural understanding, with modern innovation, the nation can pave the way for sustainable agricultural practices, efficient water distribution, and resilient infrastructure in hygiene.
As we gather for World Water Week 2023, the theme "Seeds of Change'' serves as a reminder that innovation is the cornerstone of a water-wise and water-secure world. Through dynamic and groundbreaking solutions, sharing success stories, and fostering collaboration, we can ensure discussions surrounding precision agriculture and water-saving technologies to nature-based solutions and policy innovations, take place holistically, and lead to flourishing measures including the achievement of the United Nations Sustainable Development Goals across sectors and borders.
Through cultivating these seeds of change, we continue to collaborate, innovate, and invest in a water-secure world for ourselves and generations yet to come. The path to water resilience is illuminated by our shared commitment to change - one drop, one innovation, and one policy at a time.
Nigeria's journey towards water resilience from the 2018 declaration of a State Of Emergency in water, sanitation and hygiene, to the 2023 focus on water resources for effective sanitation, demonstrates the transformative power of national policies. Recognizing the interplay between water, health, and development, Nigeria has now set its feet and hands on the path and pipes of pursuing practical and innovative approaches to water management, especially through the inclusion of sanitation. By integrating traditional and cultural understanding, with modern innovation, the nation can pave the way for sustainable agricultural practices, efficient water distribution, and resilient infrastructure in hygiene.
As we gather for World Water Week 2023, the theme "Seeds of Change'' serves as a reminder that innovation is the cornerstone of a water-wise and water-secure world. Through dynamic and groundbreaking solutions, sharing success stories, and fostering collaboration, we can ensure discussions surrounding precision agriculture and water-saving technologies to nature-based solutions and policy innovations, take place holistically, and lead to flourishing measures including the achievement of the United Nations Sustainable Development Goals across sectors and borders.
Through cultivating these seeds of change, we continue to collaborate, innovate, and invest in a water-secure world for ourselves and generations yet to come. The path to water resilience is illuminated by our shared commitment to change - one drop, one innovation, and one policy at a time.
FROM August 10th, 2023
As the High-Level Political Forum took place last month under the auspices of the UnitedNations ECOSOC, to which The Wellbeing Foundation Africa holds Special Consultative Status, the theme of accelerating recovery and full implementation of the 2030 Agenda continues to resonate as we look ahead to United Nations General Assembly (UNGA) 2023. With only seven years remaining to effect transformative change, the recently released Sustainable Development Goals Report 2023: Special Edition provides a powerful call to action, presenting a candid assessment based on the latest data. Collaboration and accountability are critical among Member States, political leaders, public institutions, and stakeholders as we navigate innovative regulatory measures that align private sector governance models with the SDGs to serve as catalysts for substantial action during the pivotal moments of the upcoming 2023 SDG Summit scheduled for this September. [video width="1920" height="1080" mp4="https://toyinsaraki.org/wp-content/uploads/2023/08/y2mate.is-The-SDG-Report-2023-Special-Edition-zF361a019zA-1080pp-1691667667.mp4"][/video] Overview Video - The Sustainable Development Report 2023: Special Edition While the report highlights existing gaps and urges the world to redouble its efforts, I am pleased that it also emphasises the potential for success through the utilisation of technologies, resources, and knowledge. According to the report, global child mortality rates show a significant decline, as between 2015 and 2021, the global under-5 mortality rate fell by 12%, and the global neonatal mortality rate fell by about 10%. While child mortality has declined in all regions, sub-Saharan Africa continues to face the highest rates, with 1 child in 14 dying before reaching age 5. To achieve the target by 2030, progress needs to accelerate in 54 countries, nearly 75% of which are in sub-Saharan Africa. The Wellbeing Foundation Africa is channelling efforts to leave a lasting health and wellbeing legacy which achieves SDG 3 through on-the-ground interventions and programming focused on reducing maternal and child mortality, ensuring access to essential healthcare services, promoting safe birthing practices, and providing capacity-building programs for midwives, nurses, and healthcare workers while advocating for leading Maternal Newborn and Child Health (MNCH) policies. Together, the global community can reignite progress towards achieving the Sustainable Development Goals and create a brighter future for all.
FROM August 2nd, 2023
World Breastfeeding Week: Empowering Mothers To Embrace Zero Water For Early And Exclusive Breastfeeding Bridges WASH for Optimal Health!
As the Wellbeing Foundation Africa celebrates World Breastfeeding Week across our frontline program locations this week, I am hugely encouraged by the uptick of national awareness, actions and year-round engagement since the WBFA and Federal Ministry of Health Core CSO Partners allied to launch our #MaternalMonday Baby Friendly Initiatives in 2011 - We all still agree that the 10 Steps To Successful Breastfeeding start with washing hands!


 Yesterday's WBW2023 Launch Activities at the WBFA started at Abuja in supporting the Federal Ministry of Health, Nigeria policy reinforcement kick-off to enable working parents to succeed in our joint Zero Water early and exclusive breastfeeding campaigns, originally implemented and through the Alive And Thrive Partners - FHI360, Unicef, Save The Children and The Wellbeing Foundation Africa. The WBFA Endowed Mamacare Antenatal, Postnatal Education, and Neonatal Intensive Care Unit Programming, continue building a community of best lactation practices across Nigeria, at scale.
Yesterday's WBW2023 Launch Activities at the WBFA started at Abuja in supporting the Federal Ministry of Health, Nigeria policy reinforcement kick-off to enable working parents to succeed in our joint Zero Water early and exclusive breastfeeding campaigns, originally implemented and through the Alive And Thrive Partners - FHI360, Unicef, Save The Children and The Wellbeing Foundation Africa. The WBFA Endowed Mamacare Antenatal, Postnatal Education, and Neonatal Intensive Care Unit Programming, continue building a community of best lactation practices across Nigeria, at scale.


 To support working parents in their efforts to breastfeed exclusively and successfully, paid parental leave (including maternity and paternity leave) is essential. This allows for equitable distribution of childcare and domestic responsibilities, reducing the gender gap. It is important to take collective action to improve working conditions and provide relevant support for breastfeeding.
To support working parents in their efforts to breastfeed exclusively and successfully, paid parental leave (including maternity and paternity leave) is essential. This allows for equitable distribution of childcare and domestic responsibilities, reducing the gender gap. It is important to take collective action to improve working conditions and provide relevant support for breastfeeding.


 The Wellbeing Foundation Africa, in partnership with Dettol Nigeria Hygiene Quest, is taking bold frontline action to transform health facilities into safe and hygienic havens for mothers through our dedicated team of #SanitationAngels. Our WBFA Midwives are interlocutors and lactation counsellors who emphasise and teach on maternal health and hygiene, establishing the understanding and importance of a clean environment. By promoting, teaching and delivering key knowledge and #WASH for wellbeing best practices, we not only empower mothers but also safeguard the health of future generations, by reducing the risk of waterborne diseases and preventing the spread of infections and transmission of germs that could compromise the health of breastfeeding mothers and their infants.
Ensuring that every healthcare facility, household and community can support mothers to embrace the precious journey and power of breastfeeding to nurture, nourish their newborns to thrive essentially requires a holistic approach to health and wellbeing, and unity in addressing environmental management of Water, Sanitation, and Hygiene.
The Wellbeing Foundation Africa, in partnership with Dettol Nigeria Hygiene Quest, is taking bold frontline action to transform health facilities into safe and hygienic havens for mothers through our dedicated team of #SanitationAngels. Our WBFA Midwives are interlocutors and lactation counsellors who emphasise and teach on maternal health and hygiene, establishing the understanding and importance of a clean environment. By promoting, teaching and delivering key knowledge and #WASH for wellbeing best practices, we not only empower mothers but also safeguard the health of future generations, by reducing the risk of waterborne diseases and preventing the spread of infections and transmission of germs that could compromise the health of breastfeeding mothers and their infants.
Ensuring that every healthcare facility, household and community can support mothers to embrace the precious journey and power of breastfeeding to nurture, nourish their newborns to thrive essentially requires a holistic approach to health and wellbeing, and unity in addressing environmental management of Water, Sanitation, and Hygiene.
FROM July 31st, 2023
Keeping Promises, Accomplishing Change - Milestone Moments in Women Delivering Maternal Health
On Maternal Monday today, I recall marking the 20th anniversary of the Safe Motherhood Initiative in 2007. History was made as the 1st Women Deliver Conference began in London that October, bringing together nearly 2,000 advocates, researchers, policymakers, and global leaders from 115 countries to assess progress in preventing maternal deaths and promoting child survival. The conference, with its theme of "Keeping Promises, Accomplishing Change," garnered attention globally and showcased the determination of individuals and nations to tackle the pressing issues of maternal health.
With strong support from world leaders, including the British Prime Minister at the time, The Right Honourable Gordon Brown HonFRSE, who emphasised the significance of investing in women as the most productive strategy for achieving the Millennium Development Goals, Women Deliver cemented the core strategies for improving maternal health, and reframed it as a basic human right and an integral strategy for achieving just development, reducing poverty, and ensuring environmental sustainability.

 The Wellbeing Foundation Africa's decades of work from the United Nations MDGs to Sustainable Development Goals (SDGs), celebrated last week's 6th Women Deliver Conference, and the first in Africa, taking place in Kigali, Rwanda, which exemplified transforming promises into action. With advocacy efforts intensified, the political will to address maternal health is growing stronger while also addressing a broader range of women's issues, such as family planning, reproductive rights, and gender-based violence. Women Deliver 2023 was instrumental in sparking dialogues and driving meaningful change by engaging policymakers, grassroots organisations, and communities.
The Wellbeing Foundation Africa's decades of work from the United Nations MDGs to Sustainable Development Goals (SDGs), celebrated last week's 6th Women Deliver Conference, and the first in Africa, taking place in Kigali, Rwanda, which exemplified transforming promises into action. With advocacy efforts intensified, the political will to address maternal health is growing stronger while also addressing a broader range of women's issues, such as family planning, reproductive rights, and gender-based violence. Women Deliver 2023 was instrumental in sparking dialogues and driving meaningful change by engaging policymakers, grassroots organisations, and communities.


 Tangentially, the United Nations Food Systems Summit +2 Stocktaking Moment, which took place in Rome, Italy, at the Food & Agriculture Organization of the United Nations (FAO) premises, highlighted the critical importance of nutrition for women, and its pivotal role in creating sustainable and resilient food systems, unlocking a cascade of positive impacts, from enhancing maternal health to empowering communities and driving economic growth.
A testament to the power of collective action towards a world where women's rights are upheld, and gender equality is the norm, we move into the future and inspire new generations of leaders, carrying the spirit of Women Deliver with us, continuing to keep promises and actively accomplishing change, until every woman's voice is heard, and every woman's rights are respected.
Tangentially, the United Nations Food Systems Summit +2 Stocktaking Moment, which took place in Rome, Italy, at the Food & Agriculture Organization of the United Nations (FAO) premises, highlighted the critical importance of nutrition for women, and its pivotal role in creating sustainable and resilient food systems, unlocking a cascade of positive impacts, from enhancing maternal health to empowering communities and driving economic growth.
A testament to the power of collective action towards a world where women's rights are upheld, and gender equality is the norm, we move into the future and inspire new generations of leaders, carrying the spirit of Women Deliver with us, continuing to keep promises and actively accomplishing change, until every woman's voice is heard, and every woman's rights are respected.
FROM July 27th, 2023
As The Wellbeing Foundation Africa and Dettol Nigeria Hygiene Quest Partnership celebrate the success and impact of programming generously supported by the dedication of the global hygiene brand Reckitt commitments to the #CleanNaija Initiative, I am delighted to share our results! The Wellbeing Foundation Africa has completed the first phase of WASH programming across schools, communities, and healthcare facilities. We have witnessed how access to soap, clean water, proper sanitation facilities, and adequate hygiene practices are essential components of human dignity and the cornerstones of healthier and more prosperous societies. Since the launch of the programme in August 2022 in Abuja, Lagos, and Kwara States, our team has made significant progress in reaching out to the target population. We have successfully engaged with 96 schools, 36 healthcare facilities and 96 communities. The impact of our efforts has been remarkable, surpassing initial expectations. We have reached 9,321 students, over 101% of the set target, connected with 25,835 pregnant and lactating mothers, over 103% of the target, and our engagement with community members has been substantial, with a total of 8,128 individuals reached, exceeding the target to 115%. These achievements underscore the effectiveness and commitment of our team in promoting education, healthcare, and community development, while engaging with stakeholders and policymakers to achieve the United Nations Sustainable Development Goals. The work continues until the shared vision of the Wellbeing Foundation Africa, Dettol Nigeria and Reckitt, is a reality, creating a Nigeria where water, sanitation, and hygiene are not privileges but fundamental rights accessible to all, as clean hands save lives.
FROM July 13th, 2023
Yesterday on Malala Day, we marked a significant milestone in the journey towards addressing girls' education. It has been exactly ten years since Malala Yousafzai, on her 16th birthday, took to the podium before the United Nations on 12 July 2013, with an unwavering determination and a voice which resonated globally, calling upon world leaders to take action and safeguard the freedom of girls to pursue education, a right for which she had nearly lost her life just a year prior. During Malala's 3rd visit to Nigeria, her words echoed with the same courage and power as she addressed a gathering of champions, young advocates, and esteemed civil society elders in Abuja at the UN House. The impact of her passionate advocacy, coupled with the tangible efforts and actions of the Malala Fund, remains evident in the lives of countless girls who have benefited from their mission of implementing and protecting every girl’s right to 12 years of free, safe, and quality education. It was an absolute honour and privilege to collaborate and participate in the momentous event themed "Addressing a Decade of Work for Girls' Education" as we gathered intergenerationally to reaffirm our support for the Malala Fund and our collective commitment to upholding the United Nations' steadfast dedication to girls' education in Nigeria. Let us remember that education is not merely a privilege, but an essential human right. It is the key that unlocks the boundless potential within every girl, regardless of her circumstances. Investing in her education is an investment in a flourishing society, where girls are empowered to overcome adversity, shatter glass ceilings, and be the next generation of leaders. May the legacy of Malala's remarkable journey inspire us all to persevere, innovate, and advocate tirelessly for girls' education. Together, let us ensure that the transformative power of education reaches every corner of Nigeria, lighting the path toward a future where every girl can thrive and contribute to a more prosperous Africa.
FROM June 26th, 2023
Pregnancy is a time of immense physical and emotional change, with heightened vulnerability, and as the rise in opioid abuse increases worldwide, it is necessary to address the growing concern of substance abuse amongst pregnant women, often intertwined with mental health challenges. The intersection of substance abuse and mental health in pregnancy presents unique barriers which require a comprehensive understanding and compassionate approach. In the Position Paper - The Rise in Opioids Abuse, I explore the complexity of addiction, stress and pregnancy, highlighting the importance of frontline holistic wellbeing programming, based in the framework and research by the @WHO Guide for Integration of Perinatal Mental Health in Maternal and Child Health Services, @UnitedNations #UNODC Integrated Opioid Strategy, and @The_Lancet_ Public Health Opioid Overdose Crisis: Time for a Radical Rethink to achieve #SDG3: Ensure Healthy Lives and Promote Well-Being for All at All Ages. By understanding and researching, the @WellbeingAfrica Foundation can further implement integrated care models, promoting community outreach and education, fostering collaboration, and investing in training; creating a supportive environment where pregnant women receive the quality and respectful care they need for a physically and mentally healthy pregnancy and a brighter future for their children. The destigmatisation and raising of awareness allows healthcare providers, policymakers, and society at large to work together to create a conducive environment where pregnant women in need are treated and protected. You can learn more by reading The Rise in Opioids Abuse below: The Rise in Opioids Abuse Paper
FROM June 22nd, 2023
8 Billion Lives, Infinite Possibilities: The Case for Rights and Choices Last week at Abuja, Nigeria, I was delighted to be represented by the Wellbeing Foundation Africa Senior Leads, at the launch of the UNFPA State of World Population Report 2023, led by UNFPA Nigeria in collaboration with the National Population Commission, and with the Federal Ministry of Health Nigeria, UN Nigeria agencies, and partners from the diplomatic, humanitarian, and development sectors in attendance. As leading advocates of the United Nations Sustainable Development Goals: SDG 3 Good Health and Well-Being and SDG 5 Gender Equality, guided by the Nairobi Statement on ICPD25, WBFA shared our continued commitment to unlocking the infinite possibilities within each of the 8 billion lives on this planet, through their programming which focuses on prioritising maternal, newborn and child health, providing comprehensive access to health services, education and support, empowering generations to achieve their full potential and lead fulfilling lives. This landmark report at the milestone of 8 billion explores how the understanding of global population trends impacts sexual and reproductive health and rights worldwide, and calls on the reframing of narratives surrounding population growth, urging global leaders to consider women's rights and their ability to freely make their own reproductive choices. Together, to ensure a resilient and equitable future, universal access to sexual and reproductive health services, and policies that center genderequality are necessary, to uphold the human rights of all people and make certain no one is left behind. 📸: With Dr. Natalia Kanem, UNFPA Executive Director, 2023 UN_Water Conference
FROM June 20th, 2023
Hope Away From Home - A World Where Refugees Are Always Included! Today on World Refugee Day, we honour people who have been forced to flee, and champion their right to seek safety, build support for their economic and social inclusion, and advocate for solutions to their challenges. The refugee situation continues to be a persistent difficulty on the African continent due to complex factors. In Nigeria, insurgency and conflict have created over 3.1 million internally displaced persons forced to flee their homes in the North-East, with Nigeria also being home to over 85,000 refugees and asylum-seekers from neighbouring countries. When refugee women are forced to flee, they are often separated from their community network of family and friends. This foundation of support is vital to many women during pregnancy and childbirth, but displaced women often feel isolated. Globally, 41% of all those #ForcedToFlee are children, and since 2018, over 1.9 million children have been born as refugees. In a key expansion of our longstanding disaster response and relief efforts, the Wellbeing Foundation Africa #midwives, in partnership with UNHCR Nigeria, began providing our continuous weekly #Mamacare360 antenatal, intrapartum and postnatal classes for women, mothers, their children and families at the Adagom Refugee Settlement in Cross River State in 2021, not only keeping people healthy, but also offering kindness, education and empowerment during a time of uncertainty. The skills and compassion of the #WBFA midwives are critical in #IDP Camps especially, fostering inclusion, and hope away from home. In activation of our UNHCR Partnerships Africa 36 Million Solutions: Africa Private Sector commitments, and aligned with the UNHCR's mission to safeguard the rights and wellbeing of all, WBFA stands #WithRefugees, as they have the right of protection from what they fear, deserve opportunities to rebuild their lives and must be given respect for their courage. #WorldRefugeeDay
FROM June 16th, 2023
I am delighted to congratulate a truly dedicated Health Champion, Dr Salma Ibrahim Anas, on the announcement of her appointment as Special Adviser on Health to His Excellency President Bola Ahmed Tinubu GCFR! Dr Salma’s appointment as the President's first choice in the health sector is a clear indication of the trust and confidence placed in her abilities, reflecting the recognition of her expertise and the significant contributions made to the healthcare system in Nigeria. Indeed, this opportunity to serve the Nation, and humanity, is a well merited upliftment, alongside Dr Salma's long standing focus on Family Health and Health Systems Strengthening. As mentioned by the Nigerian Health Watch; there are few people that could be more prepared for a role at the national level than Dr Salma, as she is affectionately known by those who know her. She has worked at all levels of the Federal Ministry of Health, at the state level as Commissioner of Health in Borno State from 2011 to 2015 to her role leading the Department of Hospital Services, NEMSAS (Nigeria Emergency Medical Services and Ambulance Scheme) and the Cancer Programme. She worked for many years for UN organisations, United Nations Population Fund (UNFPA), and the World Health Organization (WHO), in addition to leading a large DFID-funded project, MNCH2. She has seen the health sector from every possible angle, has worked directly with Ministers and Governors, has been part of the donor community defining agendas, and therefore understands the very difficult fiduciary responsibilities of working in our Nigerian context. Dr Salma’s appointment is impactful in working towards a world that values women as leaders in global health and catalysts for better health for all. Through building gender equal leadership in global and national health and going beyond gender parity to Gender Transformative Leadership, we increase the wellbeing and livelihoods of women, their families, and their communities, progress on equity, create stronger health systems for the delivery of higher quality care, allowing us to achieve the Sustainable Development Goals. I have no doubt that Dr Salma’s visionary approach, coupled with her commitment to evidence-based practices, will revolutionise the Nigerian health sector and usher in positive transformations, with her passion for public health and dedication to improving healthcare delivery being an inspiring and motivating force for others to strive for excellence. Hearty congratulations Dr Salma! 📸: 16 May 2022, Wellbeing Foundation Africa Panel At The Pathfinder International & She Forum Africa “Partnerships for Goals: Advancing the Gender Agenda for Sustainable Development
FROM June 15th, 2023
Longer lives are one of humanity's greatest achievements, and as the world’s population is ageing, it is necessary to ensure that our quality of life increases. As we commemorate the United Nations World Elder Abuse Awareness Day #WEAAD today, I join the global collaboration of the World Health Organization, Department of Economic and Social Affairs #UNDESA, Office of the United Nations High Commissioner for Human Rights #OHCHR, United Nations Population Fund #UNFPA, UN WOMEN, with support from the International Network for the Prevention of Elder Abuse #INPEA, to highlight the five priorities for the UN Decade of Healthy Ageing 2021–2030, which prevents and responds to abuse of older persons, contributing to the improvement of their health, wellbeing and dignity. My Wellbeing Foundation Africa aims to improve the lives of older people, their families and the communities in which they live, by aligning with the Sustainable Development Goals, therefore contributing to achieving the Decade’s goals through our programming, direct frontline action, partnerships, and by advocating for the Healthy Ageing Collaborative. Too many people around the world experience worse health than they should because of unsupportive environments that prevent them from maximising their later years. By shifting the way healthcare thinks, feels, and acts towards ageing, we can cultivate transformative age-friendly environments, create integrated and responsive healthcare systems and services, and ensure access to long-term care for older people who need it. #AddingLifeToYears Population ageing is set to become one of the most significant societal changes of the twenty-first century, with implications for nearly all sectors. Older individuals make valuable contributions to development, and their abilities should be integrated into healthcare policies and programming at all levels, fulfilling their enormous potential when leading healthy and abuse-free lifestyles.
FROM June 14th, 2023
It was a pleasure to be joined by High Commissioner, His Excellency Ambassador Sarafa Tunji Ishola of the Nigeria High Commission to the United Kingdom, and his amiable wife, Dr Mrs Bolanle Ishola, as Special Guests Of Honour at my Wellbeing Foundation Africa partner Reckitt, and the Health Innovation and Investment Exchange, exclusive and intimate event at the Lio London, organised in support of their non-profit, the WiNFUND. A remarkable evening with musical performances by Kalpee, TayylorMade and Afropop sensation Yemi Alade, the new Global Ambassador of #WiNFUND - it was a pleasure to discuss the importance of engendering female-led health innovations with real-world impact. Healthcare is a fundamental human right, but globally, 1 in 2 people lack access to it. Meanwhile, about 70% of healthcare workers are women, and women-led start-ups deliver 35% better returns on investments, yet only 2% of funding goes to women-led enterprises. The WiNFUND exists to disrupt that status quo by directly investing in women-led start-ups working to improve community access to healthcare across Africa. Connecting with other holders of WiNFUND NFTs, the unique digital artworks that are helping to revolutionise access to healthcare in Africa, while also creating a community of innovators, investors and supporters to champion the next generation of Africa’s women healthcare entrepreneurs, we applauded the model of combining grassroots movements, tech innovation, and the expertise of frontline workers, empowered by the use of unique NFTs (non-fungible tokens) as funding, to enable the WiNFUND to provide investment, business support and mentoring for female entrepreneurs developing leading healthcare solutions. I am proud to support the WiNFUND, to enable equitable access to investments and accelerate women-led health enterprises, increasing economic resiliency! To learn more, visit www.winfundnft.org
FROM June 8th, 2023
Immediate Kangaroo Mother Care: this may be the best 'medicine' in newborn care!
Over the past two decades, although there has been a significant decrease in child mortality rates, newborn mortality rates have not experienced the same decline. Unfortunately, today, approximately 1.6 million infants born prematurely or with low birth weight pass away within the first month.
Consequently, it is crucial to identify effective measures that can improve outcomes for newborns.
Ever since I first saw the incredible benefits of Kangaroo Mother Care, when assisting premature newborn triplets in 2006 being cared for under the expert guidance of the superbly experienced Professor Olugbenga Mokuolu, I have borne witness to the positive outcomes of physical proximity demonstrated in the effectiveness of the simple yet impactful kangaroo mother care (KMC).
This intervention involves placing the baby on the mother's chest immediately after birth and then facilitating prolonged skin-to-skin contact while emphasising breastfeeding. This powerful approach has numerous benefits for both the baby and the mother; through regulating the baby's body temperature, promoting stable heart and respiratory rates, enhances breastfeeding initiation and duration, saving numerous infants' lives worldwide.
My Wellbeing Foundation Africa champions breastfeeding and kangaroo mother-care in partnership with Medela Cares, empowering mothers and babies to establish lactation within neonatal intensive care unit’s across Nigeria. Containing the optimal and essential nutrients, antibodies, and growth factors that support the development of #NICU babies, while also protecting them against infections and diseases, breast truly is best. Breastfeeding also promotes the bonding and emotional connection between the baby and their mother, as the close physical contact stimulates the release of oxytocin, the "love hormone," fostering a sense of security, comfort and emotional wellbeing.
Also recently highlighted in an article by the Gates Foundation, #KMC immediately after birth could save 150,000 more lives each year globally. My Wellbeing Foundation Africa #frontline midwives, nurses and healthcare workers recognise and utilise the transformative potential of #KMC through providing continued education, training, and support in the #NICU setting, ensuring that every infant not only survives but thrives.
As our collaborative efforts advance healthcare practices but also establish sustainable change within communities, we can create a brighter future for the most vulnerable among us and ensure that every newborn receives the nurturing support they deserve.
At the Gates Foundation, Hema Magge, a senior program officer and a paediatrician/researcher, wants to see more widespread use of KMC, regardless of the pandemic. She calls KMC an “utterly human and humane intervention, but with all of the scientific data behind it. That’s what makes it so powerful.” She also understands its challenges. Here she shares her views on the subject:
 One of my favourite photos is from the years I spent working with the Rwanda Ministry of Health to establish some of the country’s first rural neonatal intensive care units, or NICUs. The photo shows a midwife I knew named Claudine, along with a mother and her tiny baby laying across her chest—skin to skin, the two of them wrapped together in a blanket. The baby, born early, has a feeding tube to receive her mother’s milk despite being unable to breastfeed. The midwife embraces the mother warmly. Though the mother has just gone through a difficult birth, she gazes at the camera with a look of joy. This is what the first days of getting to know your child should feel like—full of love, support, and solidarity.
One of my favourite photos is from the years I spent working with the Rwanda Ministry of Health to establish some of the country’s first rural neonatal intensive care units, or NICUs. The photo shows a midwife I knew named Claudine, along with a mother and her tiny baby laying across her chest—skin to skin, the two of them wrapped together in a blanket. The baby, born early, has a feeding tube to receive her mother’s milk despite being unable to breastfeed. The midwife embraces the mother warmly. Though the mother has just gone through a difficult birth, she gazes at the camera with a look of joy. This is what the first days of getting to know your child should feel like—full of love, support, and solidarity.
 This is a wonderful example of the power of kangaroo mother care (KMC), which supports a natural and powerful human process that provides warmth, bonding, and physiological stability. It’s adaptable and can be used alongside oxygen therapy, intravenous fluids, and even more intensive respiratory support. And it has been shown repeatedly to be extremely effective in reducing mortality in preterm and low-birth-weight babies—more effective, even, than some high-tech interventions such as incubators.
Lessons from the kangaroo mother care ward
I will confess that when I first encountered KMC more than a decade ago, I was a bit sceptical. The issue wasn’t KMC itself. I believed that keeping babies close to their mothers after birth, with skin-to-skin contact and breastfeeding, was protective on many levels. But there was a sense back then that the global development community was promoting KMC as a cheap fix in places where “modern” neonatal care wasn’t available. To me, it felt like a way to avoid confronting the injustice of under-resourced health systems in poor countries. In well-equipped hospitals, small or sick babies were whisked from their parents, supported with the latest technology, and put in incubators. At the time, I felt we should be talking more about how to ensure universal access to high-tech neonatal units like those where I trained in the United States.
I was also disheartened by what I saw in many KMC wards. Often, I’d see babies wrapped in blankets, not on a caregiver’s chest. Why weren’t the nurses putting the babies in the kangaroo position? And when mother and baby were wrapped KMC style, I sometimes got the sense that the mothers weren’t comfortable, that they felt trapped. I knew they wanted the best for their babies; so why weren’t they embracing this lifesaving practice?
I started to dig deeper, listen, and learn. I spoke with the mothers, and they taught me so much. Some felt scared to hold their tiny baby or were concerned that the baby would be cold without clothes. Others weren’t sure the baby would be safe wrapped onto them, especially if the baby was hooked up to oxygen or IV tubes. How could she provide skin-to-skin contact continuously after birth when her own body needed to recover? How could she go to the bathroom? Or prepare her own meals (since hospitals didn’t provide them)? Or get rest when hospital policies didn’t allow even her husband to visit? When I visited mothers at home after discharge, I understood how hard it must have been to stay in the hospital with a preterm infant for days or weeks when she had other children at home who needed her.
I listened to the nurses, too, and began to understand the time and energy required to care for 15 babies as the sole nurse while also addressing the mothers’ concerns, fears, and needs. I began to see how caring for a baby in an incubator—where it’s easy to monitor vital signs, change IVs, and conduct labs—could feel more straightforward in some situations. Suddenly what was billed as a “simple solution” became much more complex. For me, it was a lesson. Properly using KMC would require a culture change. Health systems would have to be redesigned to preserve the bond between mother and baby and keep them together even when the baby needs additional medical support. Infrastructure and policies would need to change. And most of all, mothers would need to be treated with dignity.
Many trials have demonstrated the clinical, nutritional, and developmental benefits of KMC, but there still has been a reluctance to use it, especially with the smallest and sickest infants.
[caption id="attachment_2011" align="alignleft" width="329"]
This is a wonderful example of the power of kangaroo mother care (KMC), which supports a natural and powerful human process that provides warmth, bonding, and physiological stability. It’s adaptable and can be used alongside oxygen therapy, intravenous fluids, and even more intensive respiratory support. And it has been shown repeatedly to be extremely effective in reducing mortality in preterm and low-birth-weight babies—more effective, even, than some high-tech interventions such as incubators.
Lessons from the kangaroo mother care ward
I will confess that when I first encountered KMC more than a decade ago, I was a bit sceptical. The issue wasn’t KMC itself. I believed that keeping babies close to their mothers after birth, with skin-to-skin contact and breastfeeding, was protective on many levels. But there was a sense back then that the global development community was promoting KMC as a cheap fix in places where “modern” neonatal care wasn’t available. To me, it felt like a way to avoid confronting the injustice of under-resourced health systems in poor countries. In well-equipped hospitals, small or sick babies were whisked from their parents, supported with the latest technology, and put in incubators. At the time, I felt we should be talking more about how to ensure universal access to high-tech neonatal units like those where I trained in the United States.
I was also disheartened by what I saw in many KMC wards. Often, I’d see babies wrapped in blankets, not on a caregiver’s chest. Why weren’t the nurses putting the babies in the kangaroo position? And when mother and baby were wrapped KMC style, I sometimes got the sense that the mothers weren’t comfortable, that they felt trapped. I knew they wanted the best for their babies; so why weren’t they embracing this lifesaving practice?
I started to dig deeper, listen, and learn. I spoke with the mothers, and they taught me so much. Some felt scared to hold their tiny baby or were concerned that the baby would be cold without clothes. Others weren’t sure the baby would be safe wrapped onto them, especially if the baby was hooked up to oxygen or IV tubes. How could she provide skin-to-skin contact continuously after birth when her own body needed to recover? How could she go to the bathroom? Or prepare her own meals (since hospitals didn’t provide them)? Or get rest when hospital policies didn’t allow even her husband to visit? When I visited mothers at home after discharge, I understood how hard it must have been to stay in the hospital with a preterm infant for days or weeks when she had other children at home who needed her.
I listened to the nurses, too, and began to understand the time and energy required to care for 15 babies as the sole nurse while also addressing the mothers’ concerns, fears, and needs. I began to see how caring for a baby in an incubator—where it’s easy to monitor vital signs, change IVs, and conduct labs—could feel more straightforward in some situations. Suddenly what was billed as a “simple solution” became much more complex. For me, it was a lesson. Properly using KMC would require a culture change. Health systems would have to be redesigned to preserve the bond between mother and baby and keep them together even when the baby needs additional medical support. Infrastructure and policies would need to change. And most of all, mothers would need to be treated with dignity.
Many trials have demonstrated the clinical, nutritional, and developmental benefits of KMC, but there still has been a reluctance to use it, especially with the smallest and sickest infants.
[caption id="attachment_2011" align="alignleft" width="329"] Mothers over machines[/caption]
The Gates Foundation funded a trial to see if this benefit could be extended safely to infants weighing just 1 to 1.8 kilograms (around 2 to 4 pounds) who were thought to first require incubator stabilization. As it turned out, the trial had to be stopped early because immediate KMC was saving so many more lives than the standard of care.
My experience in Rwanda, coupled with the volumes of research, made me think more deeply about how health systems in wealthy countries have evolved over the years toward a model of separating small and sick infants from their mothers. In a typical NICU, there isn’t even a place for a parent to sit or lie with a baby on their chest. A mother’s life-sustaining warmth, heartbeat, and gentle breathing are replaced with machines. This is happening more frequently in poor countries, too. But it’s clear to me now that in applying this scientific lens—or what we thought was scientific—we are disrupting the natural human experience. We’re also not providing the best possible care to preterm infants. Now both rich and poor countries have the challenge of undoing this harm.
Mothers over machines[/caption]
The Gates Foundation funded a trial to see if this benefit could be extended safely to infants weighing just 1 to 1.8 kilograms (around 2 to 4 pounds) who were thought to first require incubator stabilization. As it turned out, the trial had to be stopped early because immediate KMC was saving so many more lives than the standard of care.
My experience in Rwanda, coupled with the volumes of research, made me think more deeply about how health systems in wealthy countries have evolved over the years toward a model of separating small and sick infants from their mothers. In a typical NICU, there isn’t even a place for a parent to sit or lie with a baby on their chest. A mother’s life-sustaining warmth, heartbeat, and gentle breathing are replaced with machines. This is happening more frequently in poor countries, too. But it’s clear to me now that in applying this scientific lens—or what we thought was scientific—we are disrupting the natural human experience. We’re also not providing the best possible care to preterm infants. Now both rich and poor countries have the challenge of undoing this harm.
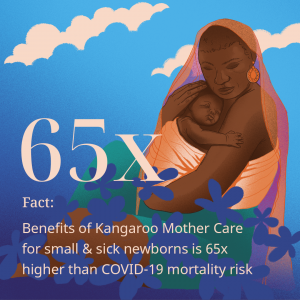 KMC and COVID-19
Certainly, COVID-19 has seriously disrupted maternal, newborn, and child health care, with both maternal mortality and stillbirths rising sharply in some settings. But this disruption has also presented opportunities, not only by exposing the fragile nature of maternal and child health—and health care systems more broadly—but by doing something to stop preventable deaths. KMC is an entry point into reimagining how to provide person-centred, comprehensive care for small and sick newborns and their mothers. The foundation is now working with WHO, UNICEF, and other global partners to support integration of KMC.
I’m optimistic that more and more doctors and nurses will recognize the transformational power of KMC. I saw it happen in Rwanda. Step by step, the hospital team started to address the issues the mothers and nurses identified. They began rethinking the physical design of neonatal units and care delivery processes and recognizing the caregivers’ expertise.
KMC and COVID-19
Certainly, COVID-19 has seriously disrupted maternal, newborn, and child health care, with both maternal mortality and stillbirths rising sharply in some settings. But this disruption has also presented opportunities, not only by exposing the fragile nature of maternal and child health—and health care systems more broadly—but by doing something to stop preventable deaths. KMC is an entry point into reimagining how to provide person-centred, comprehensive care for small and sick newborns and their mothers. The foundation is now working with WHO, UNICEF, and other global partners to support integration of KMC.
I’m optimistic that more and more doctors and nurses will recognize the transformational power of KMC. I saw it happen in Rwanda. Step by step, the hospital team started to address the issues the mothers and nurses identified. They began rethinking the physical design of neonatal units and care delivery processes and recognizing the caregivers’ expertise.
 Bolstered by the power of community and shared experience, they began realising the vision of KMC. I also see it happening in some of the best-resourced medical centres, including NICUs here in Seattle that are incorporating KMC into their care of premature infants, learning from experiences in Africa, Asia, and South America.
That vision is what I see in the photo. My friend Claudine was a clinical provider, ally, and advocate for baby and mother together. The mother felt respected and had her needs prioritised while nurturing her baby’s health. When the right tools are in place, you can walk into a KMC unit and see mothers and health care workers smiling. We just have to listen to the experts—mothers and caregivers—to do it right.
Bolstered by the power of community and shared experience, they began realising the vision of KMC. I also see it happening in some of the best-resourced medical centres, including NICUs here in Seattle that are incorporating KMC into their care of premature infants, learning from experiences in Africa, Asia, and South America.
That vision is what I see in the photo. My friend Claudine was a clinical provider, ally, and advocate for baby and mother together. The mother felt respected and had her needs prioritised while nurturing her baby’s health. When the right tools are in place, you can walk into a KMC unit and see mothers and health care workers smiling. We just have to listen to the experts—mothers and caregivers—to do it right.
FROM May 26th, 2023
This week at the Seventy-Sixth World Health Assembly, I was proud to join PMNCH, as their oldest country partner and board overseer, to ensure the practical actions countries and partners can take to improve the health and rights of women, children and adolescents across the life-course with the urgency and priority it deserves. Prior to the public discussion on the PMNCH Partners Born Too Soon: Decade of Action on Preterm Birth, my bilateral with Executive Director, Helga Fogstad of Partnership for Maternal, Newborn and Child Health, focused on the consensus building needed to promote the health and wellbeing of women, children and adolescents, based on the energy, evidence, data, practices and dialogue needed for every mother, baby and child to not only survive, but thrive throughout their life course. Deep discussions continued at the live PMNCH strategic event, Lives in the Balance: Maternal, Newborn and Child Health, featuring Bo Jacobsson, Co-Chair, MNCH workstream, Director, Maternal and Newborn Health, International Federation of Gynecology and Obstetrics, Anshu Banerjee, Director, Maternal, Newborn, Child and Adolescent Health and Ageing, Joy Phumaphi, Co-chair, Partner Engagement in Countries Committee, PMNCH, Executive Secretary of the African Leaders Malaria Alliance, John Mangwiro, Deputy Minister of Health and Child Care, Zimbabwe, Martin Chungong, Secretary-General, Inter-parliamentary Union, Michele Sumilas, Assistant to the Administrator, Bureau for Policy, Planning, and Learning, USAID, Naoko Kozuki, Director, Research and Innovation for Sexual, Reproductive, Maternal Health, International Rescue Committee and Steven Lauwerier, Acting Director, Health, UNICEF. The Born Too Soon: Decade of Action report, recently launched at the first biennial International Maternal Newborn Health Conference, has equipped us with the latest learnings that must be replicated on a wider scale. One common theme that continues to arise is the vitality of concerted multi-stakeholder collaboration and cooperation that is necessary to advance this agenda.
FROM May 23rd, 2023
Partnerships Making a Difference. I am honoured to present my 2022 Global Office and Philanthropy Annual Report, a testament to our unwavering commitment to The Wellbeing Foundation Africa mission of improving health and wellbeing across Nigeria and the world, in alignment with achieving the United Nations Sustainable Development Goals, from birth to age. As we reflect on our year, it is crucial to acknowledge the prevailing challenges and the progress made in addressing them. As we progress, we are confronting the failures within health systems head-on. My Global Office and Philanthropy remains steadfast in its dedication to addressing the root causes of and improving the overall wellbeing of the most vulnerable populations. Through supporting the Wellbeing Foundation Africa’s innovative reproductive, maternal, newborn, child, and adolescent health and nutrition programming, advocacy campaigns, and strategic partnerships, we have made significant inroads in equipping communities with knowledge, access to quality healthcare, and the tools needed. Ingrained in our decades of research, awareness and implementation, we look forward to advancing the promise, and meeting our global goals and targets. You can download my 2022 Annual Report or read it below. [3d-flip-book id="2039" ][/3d-flip-book]
FROM May 15th, 2023
According to the “Born Too Soon” report released by the United Nations agencies and partners recently, of every 10 babies born, 1 is preterm, and every 40 seconds, 1 of those babies dies. Produced by the WHO, UNICEF, in association with PMNCH - Partnership for Maternal, Newborn & Child Health and LSTM - Liverpool School of Tropical Medicine News, Born too soon: decade of action on preterm birth, sounds the alarm on what is a silent emergency of preterm births, long under-recognized in its scale and severity, which is impeding progress in improving the health and survival of children around the world. As we commemorate the United Nations International Day of Families today, it is clear that action is needed urgently to improve the prevention of preterm birth, alongside better care for affected babies and their families, as preterm birth rates have not changed in any region in the world in the past decade, with 152 million vulnerable babies born too soon from 2010 to 2020. Preterm birth is now the leading cause of stillbirths and child deaths, accounting for more than 1 in 5 of all deaths of children occurring before their 5th birthday. Preterm survivors can face lifelong health consequences, with an increased likelihood of disability and developmental delays. My The Wellbeing Foundation Africa and WBFA Midwives can heartfully attest that too often, where babies are born determines if they survive. The gaping inequalities related to ethnicity, reach, income, and access to quality care, alongside the impacts of conflict and climate change determine the likelihood of preterm birth, death, and disability. Sub-Saharan Africa has one of the highest rates of preterm birth, and preterm babies in this region face the highest mortality risk, with only 1 in 10 preterm babies surviving in low-income countries, compared to more than 9 in 10 in high-income countries. By empowering our WBFA Midwives, we have witnessed first-hand through our Mamacare360 Programming that women who receive midwife-led continuity of care provided by professional and educated midwives, regulated to international standards are: 16% less likely to lose their baby and 24% less likely to experience preterm birth. The WBFA-Medela Cares Lactation and Human Milk Initiative for mothers of infants in the Neonatal Intensive Care Unit programme is a strategic initiative built and scaled on evidence-based best practices aimed at improving the use of Own Mothers Milk in the NICU led by our WBFA midwives. Breastfeeding is one of the most effective ways to ensure child health and survival because breastmilk provides all the energy and nutrients that the infant needs for the first months of life. Research has shown that 47% of the deaths of children under 5 years occur in the first 28 days of life, and these deaths are a result of preventable diseases that can be avoided through improved nutrition with the mother's milk. Yet, we still need a clear global agenda for action, which highlights country investment and healthcare worker and parent-led activism, to advocate for access to better care, policy change and more support. Measuring the impact of the WBFA and EWEC supported Every Newborn Action Plan 2014-2020, and the ongoing 2020-2025 WHO ENAP Agenda as IMNHC 2023 took place last week, I urge the health community to increase the mobilisation of resources, accelerate implementation, integrate across sectors, and drive local innovation and research.
FROM April 24th, 2023
The Big Catch-Up on Vaccinations to ensure our world is fit for every child! As World Immunization Week 2023 begins, The UNICEF State of the World’s Children 2023, For Every Child, Vaccination Report highlights the collective action needed to protect people, and especially children, from vaccine-preventable diseases. We must now commit to the catch-up needed as millions of children during the pandemic missed out on vital vaccines, while we work to strengthen our primary health care systems to deliver the necessary immunization, emboldening happier and healthier communities that are protected. Immunization is one of the most impactful and cost-effective public health interventions available, and often brings children and families into contact with health systems, providing an opportunity for the delivery of other basic health services and laying the foundation for primary health care. Ensuring universal access to vaccines, creates a critical entry point for universal health coverage as well. 7 out of 10 children in Nigeria are not fully vaccinated by age two, with Nigeria being home to the second largest number of zero-dose children in the world. Nigeria must accelerate programming to meet the Sustainable Development Goal 3’s target of achieving more than 90% coverage of all basic vaccinations among children aged 12-23 months, and align the nation with WHO Global Vaccine Action Plan targets, as vaccine-preventable diseases like tuberculosis, measles and pneumonia continue to rank among the top killers of children under age five in the Global South. My The Wellbeing Foundation Africa implements exemplary community based and trusted programming, with strategic frontline investment in supporting robust universal immunization advocacy that reaches the most vulnerable, to expand access to vaccines to improve child health and survival. Through our flagship Mamacare360 programme, WBFA midwives address the importance of routine immunization to mothers, and the use of vaccines to protect their children, building trust and access to complete essential immunization, with the WBFA Universal Health Child Health Record Book serving as an immunization record, which improves immunization rates, building accountability and transparency. We are at a pivotal moment as we see the re-emergence of preventable diseases, and if we do not act now, millions of the world’s most vulnerable children will be left behind. Vaccination must be regarded as a national priority, as a national priority with multilateral support and global health diplomacy, as it protects not just an individual, but whole communities, laying the foundation to reach every person with the basic health services they need to thrive.
FROM April 20th, 2023
It was a pleasure to attend the Launch of the WHO-UNICEF-JICA guide on Strengthening implementation of home-based records for maternal, newborn and child health, this afternoon! The World Health Organization (WHO) recommends the use of home-based records as a complement to facility-based records, to improve care seeking behaviours, men’s involvement and support in the household, maternal and child home care practices, infant and child feeding, and communication between health workers and women, parents and caregivers, so I am delighted that my The Wellbeing Foundation Africa in-country policy team are collaborating with national policymakers and the NPHCDA, Unicef, JICA and partners to validate Nigeria's Maternal and Child Handbook this week. Having initiated the WBFA IMNCH Personal Health Records©️ in 2006, and the WBFA RMNCAH Universal Health Records©️ and Maternal Notes in 2014, I am delighted by the National Primary Health Care Development Agency (NPHCDA) leadership and multilateral organisational stakeholdership that has grown to embrace the concept of The Maternal and Child Health (MCH) Handbook in Nigeria. Published for the first time in Japan in 1948, the MCH handbook is being developed and adapted around the world. MCH handbook programs have been introduced in more than 50 countries and areas to increase knowledge and change MCH related behaviour through strengthening communication between health professionals and mothers with children. It is also utilised as a basic tool for ensuring the quality of lives of mothers, children and families. Interestingly, child health records and growth charts were introduced in Nigeria at the Wesley Guild Hospital (WGH), Ilesa, in the old Western Region back in the 1950s and early 60s by Professor David Morley, whose survey of the population of Imesi-Ile village revealed that 450 children out of every 1000 was dying before the age of five years. A full longitudinal study was initiated and over the next 18 months all children born into the community were registered, and then followed with monthly checks for a full five years. A special ‘Under Fives Clinic’ was initiated with high protein weaning food introduced. Mothers kept the children’s records with less loss than for hospital based records; Grade II midwives were taught to deal with 90% of clinical needs and to refer to the other 10%. By 1960 outpatient attendance had reached 200 000 at WGH, 80% of whom were under 18 year olds. The first measles vaccine was trialled at Ilesa and Imesi-Ile in 1960 - and thus, the pioneering work at the local Imesi-Ile community revolutionised global child health. I look forward, along with partners, to the greater strengthening and implementation of home-based records for maternal newborn and child health in Nigeria, through the adoption and domestication of the WHO, Unicef and JICA Guide For Country Programme Managers.
FROM April 18th, 2023
153 Midwives trained and counting… to save lives and improve a woman’s pregnancy experience! When I attended the Lagos State Health Services Commission Nursing Scientific Conference in July 2022, the desire for training opportunities was loud and clear, so I am delighted to witness The Wellbeing Foundation Africa Partnership with General Electric - GE Healthcare, continue our Sonology Training Program for Nigeria's Midwives on the Vscan handheld ultrasound machine at the Lagos Island Maternity Hospital today and tomorrow. Based on WHO Antenatal Care recommendations, which aim to empower all women to access the type of person-centred Antenatal Care that they require and to provide a sound foundation for such care in accordance with a respectful and human rights-based approach, the training is the first time midwives and nurses in Lagos will be educated on the US machinery, further upskilling and developing the evidence-based practices and guidance to improve the quality of care provided to all mothers and babies throughout The Wellbeing Foundation Africa continuum of care. It gives me great joy that The Wellbeing Foundation Africa is increasing access to training and medical equipment in Nigeria to empower safer births by engendering public sector midwives and nurses with the necessary knowledge and skills to utilise US machinery effectively. As national leaders in delivering a progressive antenatal intrapartum and postnatal care pathway, we are creating demand, as well as strengthening capacity, and providing a trusted community health centred approach daily to the early detection and subsequent diagnosis of women and neonates to minimise adverse complications throughout pregnancy. A well trained and equipped healthcare worker delivering quality care to an informed and empowered mother is the difference between life and death. I appreciate the excellent stakeholder engagement with the Lagos State Health Services Commission, congratulate all attendees, and reconfirm the The Wellbeing Foundation Africa commitment to champion training, and empowering healthcare workers across Nigeria, to improve health outcomes for all.
FROM April 14th, 2023
It's great news to know, as the United Nations and global development partners mark World Chagas Disease Day today, that according to the latest WHO data published in 2020, total deaths by Chagas disease in Nigeria were 0 or 0.00%. The age-adjusted death rate is 0.00 per 100,000 population, ranking Nigeria #183 globally. In 2000, there were over 1.7 billion people worldwide affected by Chagas Disease (CD), a Neglected Tropical Disease (NTD) that affects over a billion people worldwide; therefore, it is imperative that its Time to integrate Chagas Disease into primary health care. People with Chagas Disease can be found anywhere in the world. However, the transmission of the disease through the bite of "kissing bugs" (vector-borne transmission) occurs only in the Americas, typically in rural areas of Mexico, Central America and South America. The disease can also transmit from mother to child during pregnancy or through blood transfusions and organ transplants. Fatigue, fever, swollen glands, and digestive disturbances are some of the symptoms of the disease. Neglected Tropical Disease (NTA) is described as a group of infectious diseases that are common in tropical and subtropical regions. They are caused by pathogens, including viruses, bacteria, parasites, fungi and toxins. These diseases are largely overlooked and underfunded, yet they cause significant illness, disability, and death. Chagas Disease is a Neglected Tropical Disease that is not entirely dissimilar to African Sleeping Sickness, which is also an NTA. Both Sleeping Sickness and Chagas Disease are infectious diseases caused by the same parasite - Trypanosoma. The parasite Trypanosoma cruzi is the cause of Chagas Disease, while Trypanosoma brucei gambiense causes Sleeping Sickness. These parasites live in animals and can transmit from person to person threatening millions of people around the world, including 36 countries across Sub-Saharan Africa. Displacement of populations, war and poverty are also important factors that facilitate the transmission of the disease. As such, many people affected by the disease live in remote rural areas with limited access to adequate health services, complicating surveillance, diagnosis and treatment of cases. As I end this work week, I commend the dedication of every Wellbeing Foundation Africa State Project Team across Nigeria. The Wellbeing Foundation Africa programs are anchored through our flagship Mamacare360 Antenatal & Postnatal Program structure across Nigeria. Our Sokoto and Kano State Teams are making impactful progress in scaling up Zinc-LO-ORS treatments to reduce childhood diarrhoea in Northern Nigeria, supported by Nutritional International & the Government of Canada. The Lagos, Kwara, and Osun States Teams continue our WBFA Mamacare-Dettol Nigeria Hygiene Quest Programs in health care facilities, schools and communities across the FCT Abuja, Lagos and Kwara States, alongside our Osun and Cross River State Teams that continue Mamacare Maternity Programs.
FROM April 6th, 2023
According to the World Bank, despite Nigerian women making up 49.32% of Nigeria’s population, nearly half, their numerical strength fails to impact the nation’s political life with female representation in decision-making being abysmally low since Nigeria’s return to democracy in 1999. Therefore, it is with great pride that I congratulate the 7 women winners of Senatorial seats and the 11 women elected into the House of Representatives, and the 4 women elected as Deputy Governors, along with women that won House of Assembly seats in their respective states. In December 2022, I was honoured, as a Steering Council Member of the African Womens Leaders Network both in Nigeria and globally, to join the like-minded and spirited women of #AWLN, a ground-breaking movement implemented with the support of the Office of the African Union Special Envoy on Women, Peace, and Security, and of the United Nations Entity for Gender Equality and the Empowerment of Women UN Women, to promote the goals of increasing women's political participation and leadership aligned with the ElectHER movement of advancing the inclusion of women in politics, public life and ultimately achieving 51% women representation, at the ElectHer Celebrating the Nigerian Spirit Ahead of 2023, Green Wine Green Gala, funded by the European Union, in the electoral run-up of the 2023 Nigeria elections where women made up only 8.9% of the total candidates. Notwithstanding the increased advocacy in the last four years for gender balance and more active female participation in politics, female representation in the 2023 polls is believed to be the worst, compared to the 2011, 2015 and 2019 general election statistics. Closer to home in Kwara however, the 2011 elections returned 6 women in the state house of assembly, 4 women in the 2015 state assembly, no women in the 2019 state assembly, despite an encouraging history of woman's representation which included 10 female local government chairpersons, 2 female senators, 3 female federal representatives, 3 female federal ministers and an ambassador during 2003 to 2019. 5 women have been elected to the Kwara state assembly in the recently concluded 2023 election, including 26-year-old Rukayat Shittu, one of the youngest candidates in Nigeria to contest and win a political seat. It is a great pleasure to also congratulate Madame Beatrice Eyong, UN Women Country Representative to Nigeria, on receiving the International Gender Champion Special Recognition Award at the Women in Maritime and Energy Awards 2023. With over 35 years professional working experience in promoting gender equality and women's empowerment, and within her role as Country Representative of UN Women Nigeria, Ms. Eyong has led a strong multi-sectoral approach to equity across private and public industries, efforts which are essential as Nigerian women continue to be underrepresented in elective offices. Despite the challenges women face, we must continue the gust of positive energy for women’s activism and advocacy, education of women, positivity on the part of successive governments towards women empowerment, and interest of women to participate in politics.
FROM April 4th, 2023
Personal, social, health and economic education (PSHE) help children and young people stay healthy, safe and prepared for life and work. When taught well, it is a necessary part of all pupils' education to help them achieve their academic potential. As the Millennium Development Goals era concluded in 2015, my The Wellbeing Foundation Africa ushered in the bold and ambitious 2030 Agenda for Sustainable Development Goals. Adopting transformative and practical schools and visiting nursing delivery models in Nigeria to develop peer-education programming for primary and adolescents in personal, social and health education (PSHE), and water, sanitation and hygiene (WASH) knowledge and skills. Upscaled and boosted since 2022, through our impactful collaboration with, and support from, Reckitt, Dettol Nigeria and The Wellbeing Foundation Africa's (WBFA) Hygiene Quest curricula and programming, children at GJSS Gbagalape, GJSS Giri, GJSS Gwagwalada, Abuja, St Theresa Nursery and Primary School, Lagos, and Ita Aisha, Ilorin, amongst many other schools in the FCT Abuja, Lagos and Kwara states, receive weekly empowering, engaging and story-driven sessions. The Hygiene and Me module is split into two classroom topics, 'The Unseen World', which focuses on germs that cause illnesses and 'The Power of Clean Hands', which focuses on the best practices and importance of clean hands, impacting health, education, and development. By teaching our children and youth how to prevent the spread of germs through good personal hygiene habits and behaviours, we are building their understanding of hygiene, contributing towards our goal of reducing diarrhoea and keeping children and the environment in which they learn healthy and safe. The Wellbeing Foundation Africa's (WBFA) Primary & Adolescent School Nurses and Health Visitors are our Sanitation Angels. They include qualified nurses, midwives and coaches with specialist training in public health for children, young people and families. WBFA aims to reach 6 million children in Nigeria by 2025, contributing to the goal of reaching 100 million children globally by the end of 2026. They aim to achieve this through our grassroots work to deliver Clean Naija Commitments to improve water, sanitation and hygiene (WASH), reduce the burden of diarrhoeal disease and open defecation by 2030.
FROM March 31st, 2023
Never doubt that a small group of thoughtful, committed individuals can change the world. In fact, it's the only thing that ever has. - Margaret Mead As my Wellbeing Foundation Africa continues on its quest to globally contribute to achieving zero preventable maternal and neonatal deaths by 2030 through transformative approaches to health workforce education, training and skills, we gratefully and enthusiastically welcome the generous donation of eight Vscan portable handheld ultrasound machines from the Nigerian division of the global medical technology innovator, General Electric Healthcare, towards a mutual goal of increasing frontline midwives access to modern tools. I was proud to virtually join my Wellbeing Foundation Africa apex midwives and a cohort of Federal Capital Territory Abuja public health facility midwives and stakeholders today as we trained on the use of the Vscan wireless ultrasound systems at The Wellbeing Foundation Africa and UNFPA Gwagalada School of Nursing and Midwifery Skills Laboratory. This innovative technology is designed for primary health workers, including midwives, who work in remote rural settings to assess pregnancy risks early and help expand the reach of quality care to mothers who need it the most. Accessible and appropriate, the ultrasound machine is intuitive and reliable when on the ground, allowing our midwives to follow the WHO recommended one ultrasound scan before 24 weeks gestation to estimate gestational age, improve detection of foetal anomalies and multiple pregnancies, reduce the induction of labour for post-term pregnancy, and improve a woman’s pregnancy experience. Most women in developed countries receive at least two ultrasound scans during pregnancy; however, in much of Africa, this type of procedure isn't as common, drastically impacting maternal and foetal health. In Nigeria, the lifetime risk of dying during pregnancy, childbirth, postpartum, or after an abortion for a Nigerian woman is 1 in 22, compared to 1 in 4900 in developed countries, which have timely access to healthcare, including the preventative ultrasound system to detect any complications early on. Supporting the skilled deployment of these ultrasound machines will contribute to the Wellbeing Foundation Africa's progressive antenatal, intrapartum and postnatal care pathway by enabling our midwives to easily image patients at the point of care, further transforming our Mamacare 360 community health-centred programming, which commits daily to the early detection and subsequent diagnosis of women and neonates to minimise adverse antenatal intrapartum and postnatal complications. A well trained and supported midwife delivering quality and respectful antenatal and postnatal maternity care and counsel to an informed and empowered mother is the difference between life and death. We appreciate and thank the Nigeria division of GE Healthcare for donating these ultrasound machines. The accelerated and optimised care and treatment will further strengthen maternal care in the region and minimise postnatal complications, delivering better health outcomes across Nigeria and emboldening the frontline and the family!
FROM March 29th, 2023
We all agree; Water Is The Foundation of Health! Co-Creating future programmatic actions is both my purpose and my passion, so I was honoured to be invited by our trusted The Wellbeing Foundation Africa partners Reckitt to highlight and share my insights on our collaborative WBFA and Dettol Nigeria Hygiene Quest programme and curricula, which is accelerating the uptake of long-lasting WASH habits in schools, healthcare facilities and communities across Nigeria, on the sidelines of the UN-Water Conference 2023 at the UN HQ in NYC last week. Taking place at the WBFA partner McCann Worldgroup Black Box, I joined moderator David Shukman, Former BBC Correspondent and Science Editor, Fan Zhang, Lead Economist and Global Lead for Water Economics and Climate Change at the World Bank, Rajash Sarin, Regional Director, Water.org, Professor Daniele Lantagne, Tufts University, and Rodrigo Belli, CEO of Agua Camelo to discuss how water is the foundation of health, with continuum being the key to healthy communities, from access to water and sanitation to hygiene and hygienic behaviours, and finally to better health outcomes. Straight afterwards at the UNHQ, it was great to catch up with Dominic O’Neill, Executive Director and Sue Coates, Deputy Executive Director, of my long-standing advocacy partners, The Sanitation and Hygiene Fund who are a transformative UN fund that is catalysing national sanitation economies across the African Union region, including in Nigeria which is a high priority country, to pave the way for climate resilience, gender equity and water security through innovative financing in WASH. Reflecting on the Water Conference and the adoption of the Water Action Agenda, representing voluntary commitments of nations and stakeholders, including those of my ECOSOC and Global Compact accredited The Wellbeing Foundation Africa, to achieve SDG6, it is evident that without enough water at the right time in the right quality, there is no sustainable development in any sector, leaving billions behind.
FROM March 27th, 2023
A world where every child is wanted, every birth is safe, and every young person's potential is fulfilled! Last week at the United Nations, it was an honour to touchpoint with senior women leaders of the United Nations Population Fund, a multilateral development anchor partner of my The Wellbeing Foundation Africa. In my meetings with Dr. Natalia Kanem, Executive Director, on the sidelines of attending the UN Water Conference 2023 at the UN HQ in NYC with my WBFA Global Team, and with her colleagues Diene Keita, Deputy Executive Director for Programmes, and Mariarosa Cutillo, Chief of Strategic Partnerships, we reviewed the impact of our WBFA UNFPA facilitated environments where mothers and young people are empowered to achieve a high-quality of wellbeing, based on a holistic approach to progress for all. Through our WBFA UNFPA RMNCAH Nutrition International Leverage and Influence for Transformation NLIFT initiative, we pioneered integrative nutrition interventions into existing development platforms, becoming an Implementing Partner in 2018 with UNFPA to execute the MamaCare + Nutrition programme through our flagship MamaCare360. In 2019 WBFA joined Member States in making the historic commitment at the Nairobi Summit ICPD+25 convened by UNFPA, to accelerate the achievement of the three zeros by 2030: zero unmet need for contraception; zero preventable maternal deaths; and zero gender-based violence and harmful practices. Dr. Kanem, a champion for gender equality and for the health, rights, and wellbeing of women and girls presented me with the emblematic advocacy symbols of the Bodyright.me Campaign, and while together, we discussed the importance of imminently strengthening the connections between population, equity, comprehensive education and a prosperous world through investing in healthcare that prioritises women and girls, especially the most marginalised. Our work aspires to further the mission of a world where every pregnancy is wanted, every childbirth is safe and every young person's potential is fulfilled. I look forward to the continued WBFA UNFPA joint efforts, as we aim to achieve the SDGs by 2030.
FROM March 25th, 2023
Fighting Slavery’s Legacy of Racism Through Transformative Education, Partnerships For Recognition, Justice and Development. On International Day of Remembrance of the Victims of Slavery and the Transatlantic Slave Trade, I am remembering the millions of Africans who were torn away from their families, deprived of their human rights and left with trauma spanning generations. The racist legacy of the transatlantic slave trade continues to reverberate today in harmful prejudices and beliefs that impact people of African descent across the world. As proclaimed by the General Assembly, the theme for the 2015-2024 International Decade is “People of African descent: recognition, justice and development.” In proclaiming this Decade, the international community is recognising that people of African descent represent a distinct group whose human rights must be promoted and protected. Around 200 million people identifying themselves as being of African descent live in the Americas. Many millions more live in other parts of the world, outside of the continent. As I attended various work engagements at the United Nations HQ in NYC this week, with the UN Water Conference 2023 taking place, it was clear that inequities emerge from the shadows of complacency, and that discrimination and hate speech are a plague of their own. We must not let down our guard in dismantling racism and prejudice. My Wellbeing Foundation Africa’s trusted partnership and work with UN ECOSOC, UN Global Compact, UNFPA, Every Woman Every Child, and African Womens Leaders Network, harnesses years of thought leadership and experience in programming for the needs of the most marginalised and disadvantaged, as we advance equity and social justice for people of Africa and African descent, and toward the fulfilment of human rights and dignity for all. Through recognising this period of history, we can help people see the world through an ethical lens and change the status quo, with transformative education being essential to the learning of slavery in order to end racism and injustice, and to build inclusive societies based on dignity and human rights.
FROM March 24th, 2023
At the Yale Club yesterday, it was a pleasure to engage with our Wellbeing Foundation Africa commitment partners, The United Nations and UN Global Compact, to mobilise the movement of sustainable companies and stakeholders to create the healthy and thriving world we want, on the sidelines of the UN Water Conference 2023, in New York City, hosted by Reckitt, World Wildlife Fund, Water Resilience Coalition, and the Government of Mexico. The public roundtable moderated by David Shukman formerly of BBC, and featuring David Croft of Reckitt, Sarah Davidson of World Wildlife, and Jim Andrew of PepsiCo focused on achieving water positivity, which complemented the Ambition for 100 Basins, and launch of the Business Leaders Open Call for Accelerating Action on Water, creating the space for those interested groups from businesses, civil society, to governments, to chart out next steps for how to move from commitment to concrete action. We discussed the importance of water conservation for businesses operating in water stressed areas, as companies can often face unique challenges to operating responsibly when on the ground, and must harness the opportunities to make a positive impact through understanding and learning the local lens. My Wellbeing Foundation Africa supports the ten principles of the UN Global Compact with respect to human rights, labor, environment and anti-corruption. With this pledge and through this initiative, we express our intent to support stakeholders, including the private sector and governments in their implementation of sustainable improvements to water, health, wellbeing, socioeconomic development and monitoring and evaluation practices in Nigeria and globally. It was good to learn from the parliamentarians of the Government of Mexico, and their incredibly important work on water. Together, we can achieve the key dimensions of the Sustainable Development Goal 6 including water quantity, quality, and accessibility by aligning our strategies and operations innovatively.
FROM March 23rd, 2023
Turning the Tide: A Call to Collective Action I was encouraged to see the sea change in how we value, manage and use water with the Global Commission on the Economics of Water at the United Nations HQ, with the collective call for action being led by H.E. Dr. Ngozi Okonjo-Iweala, Director-General WTO, H.E. Tharman Shanmugaratnam, Senior Minister, Government of Singapore, Prof. Dr. Mariana Mazzucato, Professor in the Economics of Innovation and Public Value at University College London, and Prof. Dr. Johan Rockström, Professor in Earth System Science at University of Potsdam in the presence of H.M. King Willem-Alexander of the Netherlands and H.E. President Emomali Rahmon of Tajikistan. The seven-point Call to Collective Action provides a path that can be realised in the current decade; for how we govern, value and use water, from the local to the global, and open up major opportunities for innovation and investment, to enable more efficient, inclusive and sustainable use of water. It will enable the conversion of water to go from a growing global tragedy to immense global opportunity, to bring a new direction to policies and collaboration, ensuring that everyone has access to the water they need. Drawing on the wisdom, insights and diverse experience of the private and public sector, the Commission will continue to engage in societal dialogues worldwide over the next year and develop its ideas and proposals further with a final report, to be issued in 2024, aiming to complete the sustainability trilogy that began with the Stern Review on the Economics of Climate Change and the Dasgupta Review on the Economics of Biodiversity. A great appreciation to Henk Ovink, Special Envoy of the Kingdom of the Netherlands for Water, for his continued dedication in catalyzing this conference, as we discussed how a sustainable and just water future can be achieved, but we must treat water as what it is: our most precious global collective good, essential to protecting all ecosystems and all life, which rejuvenates our economies, benefits people everywhere, and unlocks progress in all our Sustainable Development Goals.
FROM March 22nd, 2023
Water Actions; the change we want to see in this world. Today on World Water Day 2023, I begin my engagements at the UN Water Conference at the United Nations HQ in New York City! This once-in-a-generation moment for the world to unite around water, with the last United Nations Water Conference being held 45 years ago in 1977, highlights the strong global commitment to the Sustainable Development Goals, and the continued promise that everyone will have safely managed access to water and sanitation by 2030. The latest data states that governments must work on average four times faster to meet SDG 6 on time, but water and WASH is not a situation that any single actor or group can solve. According to the WHO and UNICEF 1.4 million people die annually and 74 million will have their lives shortened by diseases related to poor water, sanitation and hygiene and today, and almost half of the global population, 3.6 billion people, lack safe sanitation. Water affects all of us, and therefore we must all take action now. Joining our trusted The Wellbeing Foundation Africa partner Reckitt, and Starbucks, Ecolab, Gap Inc., DuPont with the U.S. Government, I welcome the nearly $150 million that the Water Equity Global Access Fund IV will be investing by mid-2023 with the goal of reaching 5 million people with access to water, sanitation and hygiene. I am delighted to focus on accelerating change to solve the water and sanitation crisis, as dysfunction throughout the water cycle undermines progress on all major global issues, from health to hunger, gender equality to jobs, education to industry, and disasters to peace.
FROM March 21st, 2023
Accelerating change; Interdisciplinary expertise can tackle complex problems. As I head to global engagements on the 75th anniversary of the Universal Declaration of Human Rights, my The Wellbeing Foundation Africa Frontline Programmes continue to provide timely access and leading optimal services to health, wellbeing and social care in 230 hospitals, 92 schools, and 100 communities, across 7 states in Nigeria, for all. On International Day for the Elimination of Racial Discrimination, the urgency of combating racism and racial discrimination, based on a global set of common values and the acknowledgment that rights are inherent to every single human being, is core to the WBFA social work which aims to advance equality, combat racism, racial discrimination, and related intolerance through grassroots education and community behavioural change. As my Wellbeing Foundation Africa in Special Consultative Status to the United Nations ECOSOC advocates for the elimination of discrimination and embraces the need for equity, I am looking forward to attending this week’s United Nations Water Conference, and providing insight on advancing the Sustainable Development Goals, in particular #SDG6 - ensuring access to water and sanitation for all WASH. Water is critical for the health and prosperity of people and the planet, and frontline feedback is essential in guiding global thought leadership which leads to the necessary programmatic actions on the ground. Together, we must harness this once-in-a-generation opportunity to accelerate progress towards universal access to safe water and sanitation by 2030 to mainstream hygiene as central to community and maternal health, while eliminating conditions that perpetuate discrimination.
FROM March 2nd, 2023
Making history in Women's History Month, I was excited today, as we approach International Women's Day, to join my Wellbeing Foundation Africa anchor partners Reckitt Benckiser Group and Dettol Nigeria to celebrate the power of ‘women for health’ and launch the WiNFund. Health is something that connects us all but is tragically still not available to 50% of people across the world, yet daily I see the impact of our Wellbeing Foundation Africa's Hygiene Quest collaboration bring much needed health and hygiene practices to communities across 3 states of Nigeria, and hope to scale and spread this beneficial progress to more states. We know that women entrepreneurs create 35% better returns, yet less than 2% of VC investment goes to women. Old approaches have failed. Now is the time to disrupt this status quo. Improving access to healthcare will take new leaders, innovation and a virtuous community owned approach. I congratulate Reckitt and the Health Innovation Exchange - HIEx, along with Kofi Annan Foundation, Tokenproof and the Ecobank Foundation, who aim to impact availability of healthcare by championing the next generation of female health entrepreneurs in Africa by co-founding the Women in Innovation Fund (WiN FUND NFT) - a 100% non-profit that supports female-led health innovations with real-world impact, as 70% of the global healthcare workforce are women. The approach combines grassroots movements, tech innovation, and the expertise of frontline workers by using unique digital artwork NFTs (non-fungible tokens) to fund projects, build a community of mentors, health experts and innovators to help women-led social enterprises democratise access to health care, complimented by traditional funding routes. The first NFT collection, designed by Rwandan artist Christella Bijou, is now live, and we have received over 300 applications from women-led enterprises across seven nations in Africa, demonstrating the strong untapped potential of grassroots innovation! To learn more, you can join our community and show your support for women-led organisations through NFT HERE
FROM March 1st, 2023
Today, on Zero Discrimination Day, I am highlighting the need to ensure every human has the right to live a full and productive life, based in dignity, inclusion, compassion, and peace. Together with Africa REACH Leadership Council Members, as we took the bold step of launching our initiative to increase access to life-saving medication at the 36th AU Summit African Union in the margins of the 27th Ordinary General Assembly of the Organization of African First Ladies for Development, I conversed with UNAIDS Global Chief Winnie Byanyima, commending the focus of this year’s theme, Save lives: Decriminalise - emphasising the decriminalisation of key populations and people living with HIV, to save lives and help advance the end of the AIDS pandemic. As an Inaugural Africa REACH Board Member, and long-time advocate for the health and wellbeing of those living with HIV through The Wellbeing Foundation Africa Positive Lifeline and PMTCT programming, I continue to discourage criminal laws targeting those living with HIV as a violation of human rights, as it exacerbates the stigma and creates barriers in accessing the the support and services people need to protect their health. In 2021, United Nations member states including Nigeria made a commitment that by 2025 less than 10% of countries would have punitive legal and policy environments that affect the HIV response. Unfortunately, today, 134 countries still explicitly criminalise or prosecute HIV exposure, non-disclosure or transmission, furthering us from achieving this target and our Sustainable Development Goals. Unfairly, criminalisation of PLWHA increases vulnerability, driving discrimination and structural inequalities. Together, we must create a global movement of solidarity to end all forms of discrimination, and allow people the prospect of healthy and fulfilling lives, while working towards ending AIDS.
FROM February 17th, 2023
As women in global health from Nigeria, South Africa and Zambia, I joined Professor Flavia Senkubugeand and Dr. Choolwe Nkwemu Jacobs, to address the importance of gender-transformative leadership to bring much needed diversity in perspective and professional expertise as the African Centres for Disease Control and Prevention faces a crucial milestone in selecting its next director-general. Women have a critical role as experts in the health systems they largely deliver, and provide valuable insight to gender responsive policies which achieve better health outcomes and tackle gender inequality in the health care sector, which undermines global health efforts. Therefore, together, as supporters of the Women in Global Health movement with 46 chapters worldwide, and the largest presence in Africa, we are calling on the African Union, Africa CDC, and its member states to consider women equally in all senior decision-making levels, as the African region has no shortage of talented women capable of taking on these important roles, including that of director-general. Read our full thoughts here.
FROM February 10th, 2023
On World Pulses Day 2023, I am encouraged that the Food and Agriculture Organization (FAO) campaign highlights raising awareness of the importance of pulses in diets within Sub-Saharan Africa. Pulses such as dry peas, chickpeas, cow peas and lentils positively contribute to food security, nutrient dense diets, and have adapted to adverse climatic conditions, allowing them to grow resiliently and sustainably, providing healthier and productive lives. My Wellbeing Foundation Africa prioritises the nutritional status of children and women who are most vulnerable to malnutrition. Our WBFA frontline midwives encourage good nutrition every day, as the first defence against poor health outcomes, and aim to break the intergenerational cycle of malnutrition in communities, as the right to adequate food is universal for all. The production and consumption of pulses has transformed and diversified farming systems. Farmers can both sell and consume them, aiding in maintaining household food security and economic stability, while improving lives globally. It is rich in soluble fibre and high in protein, which can help control blood sugar, lower cholesterol, making it a recommended and accessible addition to diets by the WHO for the management of non-communicable diseases. Pulses can also thrive in water scarce environments, as they have a low water footprint and better tolerate drought and climate-related disasters, making them adaptable for agriculture livelihoods during shifts in weather patterns. The production of pulses of Africa increased from 5.11 million tonnes in 1972 to 22 million tonnes in 2021 growing at an average annual rate of 3.32%. We must prioritise advocating to, and collaborating with governments, and the private sector alongside the public and youth to support the education, production and consumption of pulses as part of sustainable food systems, healthy diets and to achieve the United Nations, The Global Goals, SDG 2.
FROM February 7th, 2023
As World Interfaith Harmony Week 2023 comes to a close, I am recognising the affirmative power of inter-religious dialogue based in mutual understanding and a culture of peace, to continue as a way to promote harmony, cooperation and goodwill between all, and at all times. Respect and dignity provide a platform which encourages the powerful movement of interfaith unity built on diversity, solidarity, tolerance and human dignity, World Interfaith Harmony Week 2023 exemplifies that our common values of, Love of God, Love of Good and Love of One’s Neighbour, far outweigh our differences. Governments, institutions and civil society such as my The Wellbeing Foundation must continue to prioritise various educational programmes and initiatives at the community level to build bridges across boundaries, and achieve the World Interfaith Harmony Week 2023 objectives of working together for gender equality, mental health, wellbeing, and environmental preservation.







FROM February 6th, 2023
My thoughts and prayers are with President Recep Tayyip Erdoğan and First Lady Emine Erdoğan, the Turkish Government and the people of Central and South-East Turkey, as well as the people and refugees of already vulnerable Northern Syria today, as they face the traumatic aftermath and damage of the devastating earthquakes this morning.
First responders have commenced rescue efforts and calls for international assistance are underway. In times such as these, collective efforts, support and global unity is required.
The WHO Director-General, Dr Tedros Adhanom Ghebreyesushas has immediately assured that the WHO network of emergency medical assistance has been promptly activated to provide essential care for the injured and most vulnerable. This response alongside those of national and international humanitarian agencies and organisations will be vital to provide sustained support at such a trying time.
My condolences to the families who have lost loved ones, as I hope and pray that rescue efforts brace up with coordinated strength and fortitude for the difficult hours and days that lie ahead.






FROM February 6th, 2023
International Day of Zero Tolerance for Female Genital Mutilation reminds us of the continued prevalence of this international violation of the human rights of girls and women, deep-rooted in inequality and discrimination, breaching their rights to health, security and integrity. According to UNICEF female genital mutilation continues to be on the rise among Nigerian girls aged 0-14, while accounting for the third highest number of women and girls who have been subjected to FGM globally. Over 68 million girls worldwide are estimated to be at risk of female genital mutilation during the 15-year plan to achieve the United Nations Global Goals SDGs, with 4.32 million in 2023 alone. As a UNFPA community stakeholder committed to the Nairobi Summit ICPD+25, WBFA aims to achieve; zero unmet needs for family planning and services, zero preventable maternal and infant deaths, zero sexual and gender-based violence including early and forced marriage, as well as female genital mutilation by advancing universal access to sexual and reproductive health, reinforcing the goal to end preventable maternal deaths. Our Wellbeing Foundation Africa's Mamacare360 Midwives work daily to protect the health, wellbeing, childhoods, education and ambitions of our girls and women, within the primary healthcare centres, households, schools and communities to engage families and focus on gender equality. Through safe space counselling during our Mamacare 360 programme, we are able to detect and support FGM survivors, and provide the opportunity to break the cycle by using education and awareness to urge mothers not to subject their daughters to this harmful practice. We must all continue to come together to accelerate our efforts to achieve a safe Nigeria for all, and eliminate this harmful practice completely. #EndFGM #MenEndFGM
FROM February 6th, 2023
A thankful Maternal Monday today, with the gladdening news of the safe delivery of triplets to a Wellbeing Foundation Africa’s Mamacare 360 Antenatal Classes family in Ilorin, Kwara State! When I founded the WBFA in 2004, it was to improve maternal, newborn and child survival outcomes in Kwara and Nigeria, and now in 2023 this delivery is a testimony to the carefully intersected and integrated program offerings we provide. From home-based health records empowering information and data, to every child-bearing woman receiving free and monthly educational midwifery maternity ANC care, to delivery by highly skilled health professionals trained in emergency obstetric care, to early and exclusive induction of lactation in the Neonatal Intensive Care Unit with the expression and administration of buccal colostrum and opportunities for kangaroo care bonding, I am immensely appreciative for our decades long productive partnership with the General Hospital Ilorin, and the tertiary University of Ilorin Teaching Hospital, and for the dedicated and diligent duties of our Wellbeing Foundation Africa Midwives and State Project Team. I hope and pray that father, mother and the babies continue to thrive, Amen. #Alaafia #AlaafiaKwara #KwaraWellbeing #CommittedToCaring
FROM February 4th, 2023
On World Cancer Day, I am joining my Wellbeing Foundation Africa in advocating for comprehensive healthcare which prioritises cancer innovation, early detection, prevention, treatment and support to make the world a healthier place. According to the WHO, globally, nearly 1 in 6 deaths are due to cancer, with an estimated 70% of all cancer deaths occurring in the Global South, making it the leading cause of death worldwide. Though over 40% of all cancers are preventable, a lack of access to essential health services, healthier behaviours, regular screening, and cancer education and care means that many are denied a timely diagnosis and treatment - furthering the equity gap as most disadvantaged groups are also more likely to have increased exposures to a host of risk factors, like tobacco, an unhealthy diet or environmental hazards. According to my Wellbeing Foundation Africa and Amref Health Africa’s landmark 2018 Rapid Assessment of Cancer Care in Nigeria - which guided Nigeria’s policymakers in formulating National Cancer Strategy and Registries - the burden and trend of non-communicable diseases - including cancer - is on the increase in Nigeria. That is why myself and WBFA continue to bridge the gap, empower and support organisations and activations such as the LSTM News Co-Creation Workshop to identity the gaps, the needs, and barriers in Midwifery, Oncology and Mental Health nursing in Nigeria, the Marcelle Ruth Cancer Centre and Specialist Hospital, The Bricon Foundation, Medicaid Cancer Foundation and the Cancer Walk with WHO Nigeria, as we continue to work toward and emphasise the importance of achieving the UN, The Global Goals for Sustainable Development by 2030. With 19.3 million new cases of cancer this past year, each and every one of us can contribute to creating a health community that will make real progress in reducing the global impact of cancer; because change begins with a ripple and ends with a wave. #CloseTheCareGap #GlobalGoals
FROM January 30th, 2023
Act now. Act together. Invest in Neglected Tropical Diseases. World Neglected Tropical Disease Day brings heightened awareness to the need for immediate sustainable financing, and country accountability of #NTDs which are widespread in the developing world affecting the most vulnerable populations and regions, but are since controlled or eradicated in the developed world, to accelerate progress towards the World Health Organization NTD road map targets by 2030. Though NTDs affect 1.7 billion people worldwide, and account for 57 million disability-adjusted life-years lost, the lack of awareness and concerted global action to tackle this diverse group of 20 conditions prevalent in tropical areas, disproportionately affecting women and children in impoverished communities have led to very little funding and international attention. These diseases, many of which are vector-borne, have animal reservoirs and complex life-cycles, making their public health control challenging, are “neglected” as they are almost always absent from the global health agenda and are associated with stigma and social exclusion. Prevalent in areas where the understanding of #WASH, #nutrition and #onehealth are inadequate, these diseases of neglected populations perpetuate a cycle of poverty, poor health outcomes and limited economic opportunity. Nigeria is one of the most endemic countries in the world for NTDs, with an estimated 100 million people in the country at-risk for at least one NTD, and accounting for about 25% of the burden of NTDs in Africa. Through my Wellbeing Foundation Africa programmes, we are #100PercentCommitted to beating NTDs; and in my advocacy withThe END Fund, I have witnessed firsthand how grassroots collective action and programming strengthen public health measures and disease surveillance, allowing for the upskilling of local health workers, accessible treatment, and community behavioural change to effectively control, eliminate and eradicate #NTDs. The new World Health Organization progress report released, entitled “Global report on neglected tropical diseases 2023” highlights that we have the tools to save lives, prevent suffering and make 2023 the year to shine a spotlight on investing in universal care to end these diseases that are entirely preventable. Equity in access, equity in care and equity in recognition are needed to #BeatNTDs.
FROM January 26th, 2023
It was a great privilege to host and introduce the WHO Foundation Health Emergencies: Stories from the Frontline of a Climate Crisis Reception with Anil Soni, Chief Executive Officer at WHO Foundation, joined by Ndidi Okonkwo Nwuneli, Executive Chair, Sahel Consulting Agriculture & Nutrition, Emi Mahmoud, UNHCR Goodwill Ambassador, Kamal Ahmed, Editor-in-Chief and Co-founder The News Movement, and Vanina Laurent-Ledu, President of the Foundation S - The Sanofi Collective, at the World Economic Forum in Davos last week. Using the power of storytelling, and showcasing the talent, creativity, and innovation from two regions at the frontline of a health and climate crisis in the greater Horn of Africa and the Sahel, we explored the impact climate change has on global health, from starvation to disease. As the WHO Foundation’s Inaugural Ambassador for Global Health, and Special Advisor, Independent Advisory Group, WHO Africa Regional Office, I aim to raise awareness and tackle the particular challenges Africa and Nigeria face in global health situations by using my experience and network to mobilise a key opportunity for private sector leadership and resource procurement. I am supporting the WHO and its work on the ground as they increase the capacity of health workers, prevent the spread of disease, provide essential medicines and emergency nutrition, vaccinations, and set up mobile health centres for people forced to leave their homes. Currently more than 60 million people across 13 countries in the greater Horn of Africa and the Sahel face extreme hunger or are in need of life-saving assistance - some countries are facing the worst drought in a generation, while others are coping with dramatic flooding. The emergency is heightened across both regions by conflict and a sharp rise in global food and fuel prices, linked to the war in Ukraine. The situation is already dire and fast deteriorating. In my own country of Nigeria, many were displaced by devastating floods, and during that time Nigerians had no choice but to use floodwaters as drinking water, despite the risk of contracting diarrheal diseases, including cholera from contaminated water. At this moment nearly 1.5 million infants and children alone are in need of urgent humanitarian assistance and with 1.3 million people displaced - there is a growing and heightened risk of waterborne diseases, drowning and malnutrition. WHO has responded by rapidly providing emergency health kits for 900,000 people, deploying mobile health teams that are delivering emergency nutrition, medicines, vaccines, and health care in many displacement camps with particular support for children, pregnant and lactating women. Through supporting and advocating for the WHO Foundation’s Emergency Appeal for the greater Horn of Africa and the Sahel Regions, we can tackle this escalating crisis through collective and agile action, as WHO and its partners in the region must be empowered to respond immediately and comprehensively through various resources for the utmost impact. My Wellbeing Foundation Africa shares the WHO Foundation and WHO mission to ensure that health is for all, and that where you are born should not determine how you live. They exist to ensure that the resources and partners needed to achieve this mission are mobilised, assisting WHO to carry out life-saving work and supporting countries and communities around the world with climate-resilient healthcare. It is crucial we continue to amplify the inspiring voices of the people addressing injustice and affecting change in their communities, to improve the health and wellbeing of the people and places they love. Global health needs us all, from every country, to work as one. We must all dedicate ourselves to keeping the world safe, and advocate for the protection of the most vulnerable. By working together, we can change the lives of future generations.
FROM January 10th, 2023
FROM December 8th, 2022
Someone is sitting in the shade today because someone else planted a tree long ago. - Warren Buffett This #ThrowbackThursday I am reflecting on the Forbes 400 Summit on Philanthropy in 2013, where I discussed the importance of purposeful giving, and how the actions of one person can make a difference in the outcome of many lives alongside Warren Buffet and Bill Gates. Reproductive health care, more than most issues, has been enormously shaped by individual billionaire philanthropists. Many of the critical breakthroughs in the field were philanthropy-funded, as are many basic services today around the world. Bill Gates, through the Bill & Melinda Gates Foundation, and Warren Buffett, through the Susan Thompson Buffett Foundation are two of the biggest philanthropists, and leading providers of access to contraception worldwide. The Gates Foundation empowers women and girls to take charge of their own health, enabling them to make informed decisions about family planning and have access to contraceptive options that meet their needs, to reach the longer-term goal of universal access to voluntary family planning. The Buffett Foundation is the leading provider of family planning access for poor women in the U.S, and the the most influential supporter of expanding access to and conducting research on the contraceptive. Philanthropy is essential for reproductive health care, as foundations, including my Wellbeing Foundation Africa can decentralise the definition and distribution of public health goods from the government, operate on a longer time scale than many businesses in the marketplace and elected officials in public institutions, and create frontline trusted programming which educate and influence community behavioural change to meet better health outcomes and achieve the United Nations Sustainable Development Goals. If you're in the luckiest one per cent of humanity, you owe it to the rest of humanity to think about the other 99 per cent. - Warren Buffett 📸📹: Forbes 400 Summit on Philanthropy, 2013
FROM December 5th, 2022
Healthy soils are the basis for healthy and nutritious food: it all starts in soils, where food begins! While at the recent #COP27 in Sharm el-Sheikh, Egypt, I took the opportunity to update my knowledge of agriculture and food security at the first-ever food systems pavilion, and with the Islamic Development Bank, both who shined a spotlight on the foundation of life on land. The pavilion, and Adaptation and Agriculture Day at #AfricaCOP represented an extensive and important opportunity to ensure that the health of the planet’s soil, and with it, all the nutritional, ecosystem, and climate benefits soil provides is considered by policymakers in discussions, and led to a new United Nations agreement on a four-year plan and initiative aimed at scaling up finance to transform agriculture by 2030. Alongside this, in my discussions with Eng. Hani Salem Sonbol, CEO of the Islamic Development Bank Group’s international trade financing arm, the International Islamic Trade Finance Corporation (ITFC), and Acting CEO of the Islamic Corporation for the Development of the Private Sector (ICD), I was pleased to learn that since its inception, the Bank has approved a total of US$12.3 billion for investment projects in agriculture and rural development across its 57 member countries, including the Nigerian states of Kaduna, Kano, Kwara, Imo, Cross River, Ogun, and Oyo, and the Federal Capital Territory, Abuja, with the ISDB and the Government of Nigeria recently signing a US$150 million financing agreement for a flagship project that provides extensive support to the country’s food security. As part of a mega co-financing effort for the launching of the Special Agro-Industrial Processing Zone (SAPZ) Project in the Federal Republic of Nigeria, the project aims to support poverty alleviation, stimulate sustainable activities for low-income households, and enhance the competitiveness of the agriculture sector through the promotion of select value chains in the country. In addition to the Federal Capital Territory (FCT), SAPZ Program will cover seven other states namely Kaduna, Kano, Kwara, Imo, Cross River, Ogun, and Oyo, while the ISDB Project will cover FCT, Kano, and Kwara States, towards (i) development of infrastructure for 3 Agro-Industrial Processing Hubs (AIHs); (ii) 10 Agricultural Transformation Centers (ATCs); (iii) improvement of irrigated land & farm to market access roads; (iv) supply of certified agricultural inputs and extension services; (v) skills development for 10,000 farmers and MSMEs; and (vi) updating agro-industrial zone policy and establishment of a regulatory institution/special regulatory regime. Expected outcomes are: (i) increasing investments by private sector companies within the AIHs by US$375 million; (ii) creating 185,000 new jobs, including 50% for women and 50% for youth; (iii) increasing the yields of key crops by at least 50%; (iv) reducing post-harvest losses within the catchment area by at least 10-20%; and (v) increasing in the income of small producers/farmers by 25%. Once operational, the project will support inclusive and sustainable agro-industrial development and enhance the competitiveness of the agriculture sector through the promotion of select value chains. The Agriculture and Rural Development department develops and implements the Bank’s strategy, assistance framework, plan of action and work program in the agriculture and rural development sector. Its mission is to promote sustainable, inclusive, integrated and equitable agriculture and rural development that supports the modernization of food systems, enhances food security and increases the resilience of populations through efficient natural resources management, and increased productivity and connectivity. The Project will contribute to Nigeria's effort in achieving its SDG targets, specifically on the following: SDG1, SDG2, SDG5, SDG9, SDG12, SDG13 & SDG17. Nigeria became a member of the IsDB Group in 2005. The country is a key beneficiary of the IsDB financing in Africa with a total portfolio of approved operations amounting to US$ 1.8 billion. IsDB Group's financial support for Nigeria is diverse, covering broad sectors of the economy. Agriculture infrastructure projects account for 29 % of IsDB's financing for Nigeria, followed by health (18%), transportation (17%), and water (15%), among others. The Bank also has a solid pipeline of projects to be processed between 2022 and 2023. Over the last 70 years, the level of vitamins and nutrients in food has drastically decreased, and it is estimated that 2 billion people worldwide suffer from lack of micronutrients, known as #hiddenhunger, with about two-thirds of the world's population at risk of deficiency in one or more essential mineral elements. My Wellbeing Foundation Africa has long worked to combat nutrition deficiencies and educate families and communities through our historical Alive and Thrive and Mamacare+NLift iterations,, as well as current LOORS-Zinc programming because we know that impact in health and social development is most keenly felt and measured at the household level in improving daily nutrition and food security. This #WorldSoilDay2022, we must immediately take action to prevent and reverse nutrient imbalances in agri-food systems, as soil plays a key role in all four dimensions of food security: availability, access, utilisation and stability. #WorldSoilDay #Soils4Nutrition #MaternalMonday
FROM November 30th, 2022
Yesterday, I marked the 3rd Anniversary of the Nairobi Summit on the International Conference on Population and Development #ICPD25 with the National Population Commission and United Nations Population Fund (UNFPA) under the theme “Sexual and Reproductive Justice as the Vehicle to Deliver the Nairobi Summit Commitments.”
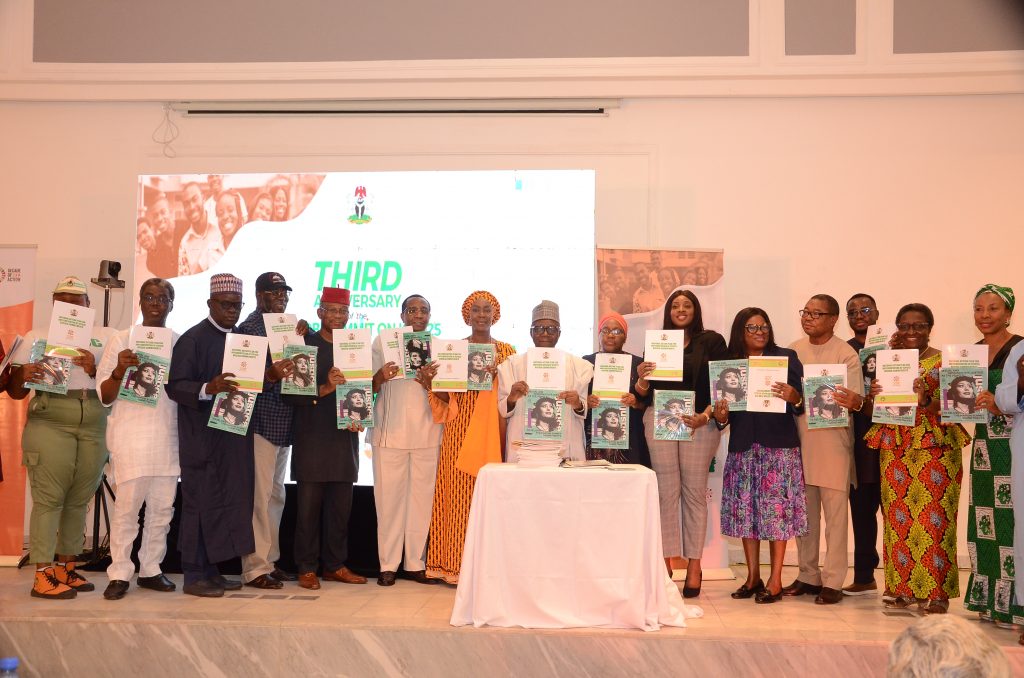 As the Nigeria Representative Member of the ICPD25 High Level Commission International Steering Committee and as UNFPA Nigeria Family Planning Champion, I was delighted to deliver a goodwill message and keynote presentation on the Wellbeing Foundation Africa 2019-2022 Progress Impact Report towards the 3 zeros of: zero unmet needs for family planning and services, zero preventable maternal and infant deaths, zero sexual and gender-based violence.
I was pleased to join Mallam Isa Kwarra, Chairman National Population Commission, Ms Ulla Mueller, UNFPA Resident Representative, H.E. Sune Krogstrup, Denmark Ambassador, H.E. Samuel Mogere, Charges D'Affaires, Kenya High Commission, Ambassadors of Namibia and Madagascar, Mr Mathias Schmale, United Nations Resident Coordinator, Dr Ejike Orji, Chair, Association of Advancement For Family Planning, the National Youth Service Corps Representatives, and Representatives of the Honorable Ministers of Women Affairs, Health, and Sports and Youth Development respectively - in launching the National Action Plan for Nairobi Commitment, and the Launch of The High Level Commission 2022 Report on the Nairobi Summit on ICPD25 Follow-Up.
Alongside WBFA Programs Director Dr Franco Apiyanteide, I affirmed that the Wellbeing Foundation continues to prioritise the most amplified issues from the summit; having a global impact that advocates for women, children and families, through empowering and educating #frontline health workers while increasing accessibility to #healthcare, #SHRH and #WASH.
As the Nigeria Representative Member of the ICPD25 High Level Commission International Steering Committee and as UNFPA Nigeria Family Planning Champion, I was delighted to deliver a goodwill message and keynote presentation on the Wellbeing Foundation Africa 2019-2022 Progress Impact Report towards the 3 zeros of: zero unmet needs for family planning and services, zero preventable maternal and infant deaths, zero sexual and gender-based violence.
I was pleased to join Mallam Isa Kwarra, Chairman National Population Commission, Ms Ulla Mueller, UNFPA Resident Representative, H.E. Sune Krogstrup, Denmark Ambassador, H.E. Samuel Mogere, Charges D'Affaires, Kenya High Commission, Ambassadors of Namibia and Madagascar, Mr Mathias Schmale, United Nations Resident Coordinator, Dr Ejike Orji, Chair, Association of Advancement For Family Planning, the National Youth Service Corps Representatives, and Representatives of the Honorable Ministers of Women Affairs, Health, and Sports and Youth Development respectively - in launching the National Action Plan for Nairobi Commitment, and the Launch of The High Level Commission 2022 Report on the Nairobi Summit on ICPD25 Follow-Up.
Alongside WBFA Programs Director Dr Franco Apiyanteide, I affirmed that the Wellbeing Foundation continues to prioritise the most amplified issues from the summit; having a global impact that advocates for women, children and families, through empowering and educating #frontline health workers while increasing accessibility to #healthcare, #SHRH and #WASH.


FROM November 28th, 2022
As International Day for the Elimination of Violence Against Women last Friday marked the launch of the United Nations UNiTE campaign led by UN Secretary-General Antonio Guterres and UNWomen, I commit to standing in solidarity and taking action this 16 days of activism in hopes to further prevent and eliminate violence against women and girls, call for global action to increase awareness, and create opportunities for discussion on solutions to achieve Sustainable Development Goal 5: gender equality and empower all women and girls. Violence against women and girls is one of the most widespread, persistent and devastating human rights violations today. For many women and girls in Nigeria, home, school and communities remain unsafe, despite violence in all forms being preventable. Almost one in three women aged 15-49 have experienced physical violence, with one in four girls, including very young ones, experiencing sexual violence, in Nigeria. The Wellbeing Africa Foundation is targeting this worrying data and trend through our various programming, by raising awareness, educating families and influencing positive community behavioural change. Our midwives and nurses promote a culture that does not tolerate any form of violence and break down the stigma attached to the social norms which allow this behaviour to go unspoken and unpunished. Through the safe, brave and supportive spaces WBFA creates, we are contributing to the fulfilment of women’s and girls’ human rights and to the achievement of the 2030 Agenda for Sustainable Development. Violence cuts across all generations, cultures, levels of education, income, religion and backgrounds. We must all join to act and ensure we leave no woman or girl behind by adopting adequate laws and legislation, addressing harmful gender norms, and providing comprehensive access to health resources and services for justice. Let us unite, take a stand, and raise our voices in support of women and girls’ rights. #16Days #OrangeTheWorld
FROM November 3rd, 2022
Each of us has a choice about how we respond to the extraordinary times in which we find ourselves. Each of us can see differently, act differently, and change things for the better.
Saying nothing and doing nothing is unacceptable as the courageous women and girls of Iran, their families and their allies are rightfully demanding their basic fundamental human rights.
We can all stand in solidarity at this critical moment, joining leaders in the international community to vocally and unequivocally demonstrate support for women’s rights in the demand that the Islamic Republic of Iran is suspended from the @UnitedNations #CSW Commission on the Status for Women, a governing body that needs to maintain credibility for it to serve women and girls worldwide, until and when the rights of women and girls are restored, respected and upheld.
The arc of the social justice universe is long, but can be extended to reach the guarantee for rights for women and girls everywhere. Be part of the unity of change; join me in signing this declaration. Woman. Life. Freedom. In solidarity with Iranian women and girls, today. bit.ly/IRIoffCSW
#Zan #Zendegi #Azadi
#WomenLifeFreedom #IRIoffCSW
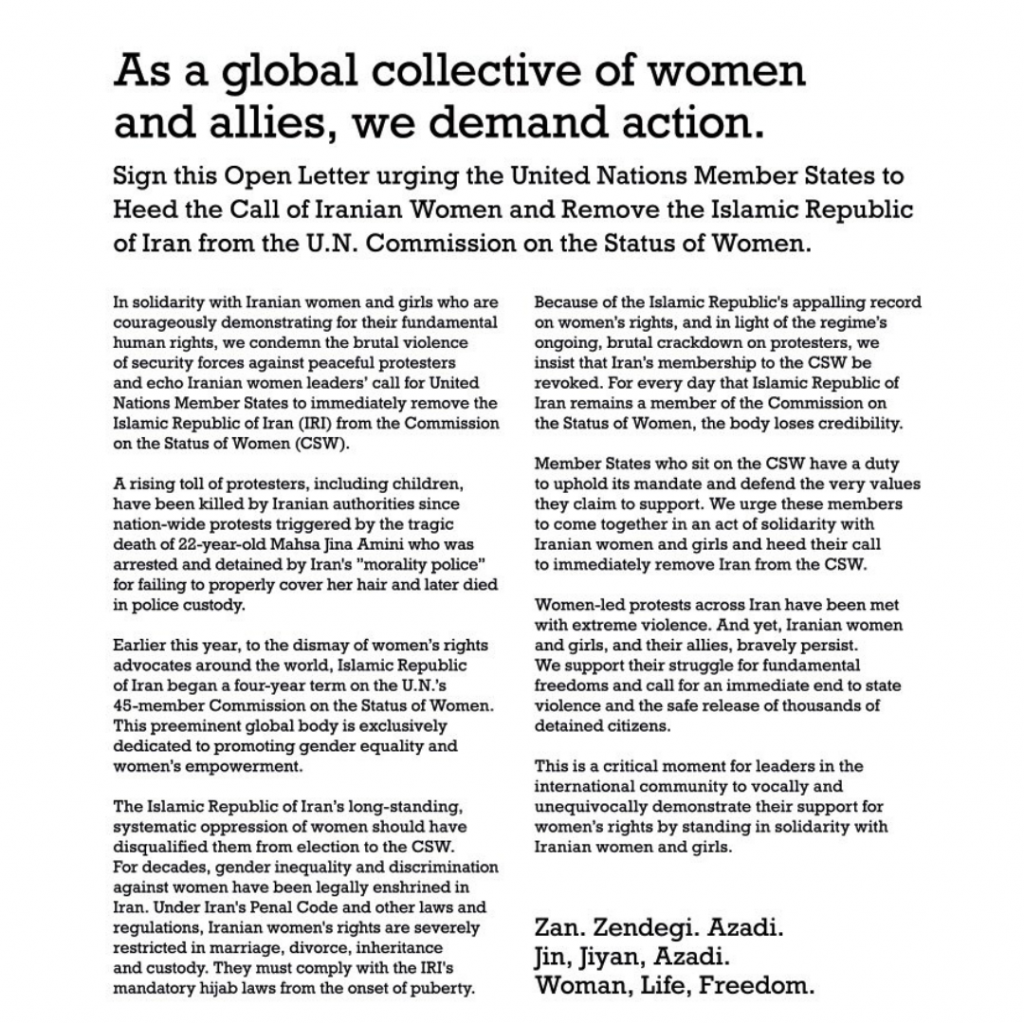
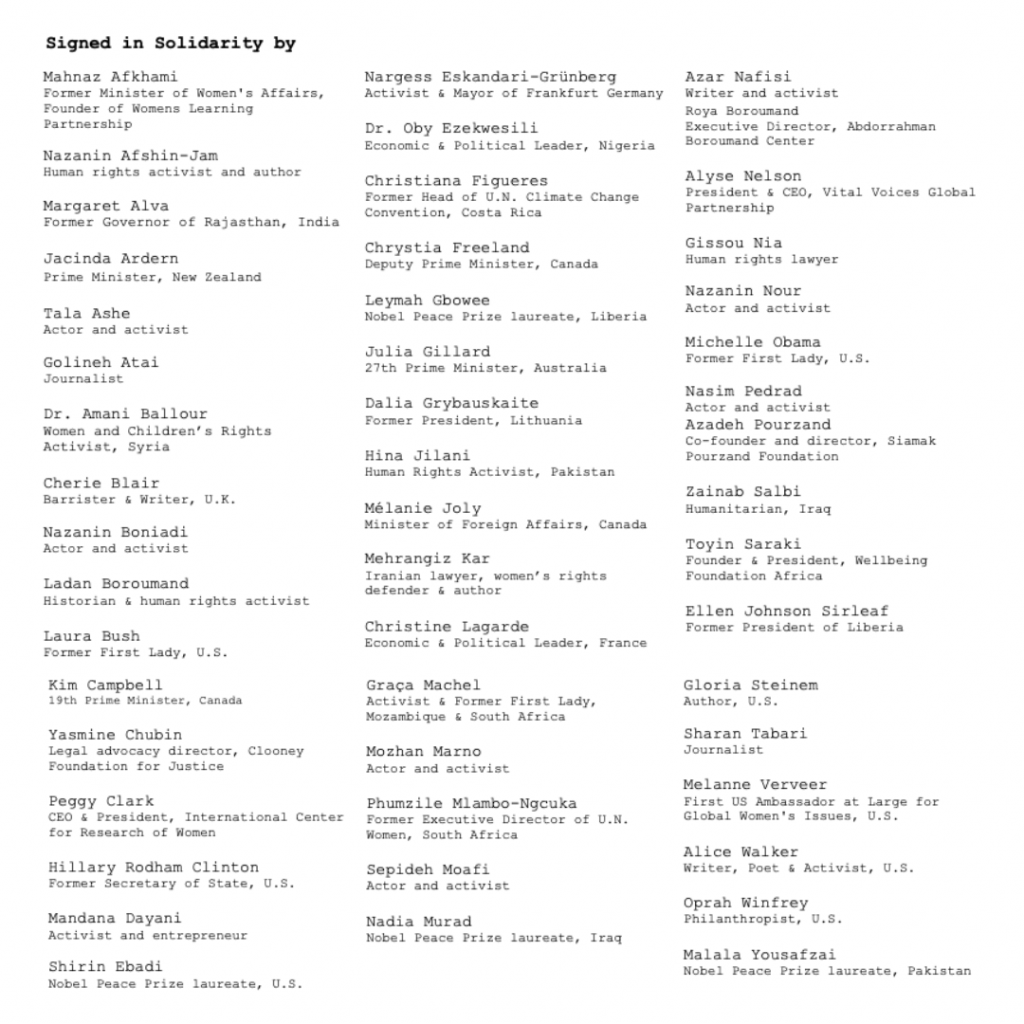
FROM October 31st, 2022
In my Goodwill Statement to Africa Reach, on whose Leadership Council I am honoured to serve, I stated that "the milestone of Zimbabwe becoming the first African nation to approve injectable PrEP prophylaxis for HIV post-exposure infection prevention is a highly welcomed breakthrough moment. A truly significant step in the right direction in delivering accessible and equitable treatment and prevention, breaking down systemic barriers, and addressing the unmet needs of the HIV burden."
"Currently 90% of all children living with HIV globally are located in Africa, and nearly two thirds of all new cases of HIV occur in Sub-Saharan Africa, with women and the girl child in this region bearing the disproportionate load of the HIV epidemic. Each and every person deserves optimal treatment and the opportunity to live a healthy life to its full potential. I look forward to the positive impact of injectable PrEP for Africa and in achieving the United Nations Sustainable Development Goals.”Prevention remains one of the most important interventions in the HIV response, and I am grateful to join the Chair of Africa REACH, First Lady of Namibia Her Excellency Monica Geingos to expand and strengthen HIV programming across Africa as we advocate and work towards bringing the #PediatricAIDS conversation to the fore. The Africa REACH initiative brings together the most powerful elements of African political structures, cultural influence and generational leadership to create a new action agenda around ending AIDS in children and youth in Africa. As we fight to end the AIDS pandemic, I look forward to welcoming the long awaited advancement of injectable PrEP to Nigeria, where we have over an estimated 1.9 million people living with HIV and AIDs to ensure health and wellbeing for all.
FROM October 30th, 2022
I have noticed over the years that the spread of fake news tends to rise in Nigeria ahead of general election cycles, of which the next is expected to take place in 2023. While many journalists report that it can be difficult to verify information from prominent figures, that is no excuse for malicious fiction to be presented as fact. I was disappointed and perturbed this week, to learn that some unscrupulous politically motivated individuals and digitally networked elements were deliberately and maliciously circulating a sensationally lurid video virally across Nigerian messaging and multimedia platforms - defamatorily alleging that it depicted a member of my family - in a coordinated and totally false negative disinformation and misinformation publication campaign of particularly vicious virulence. Knowing without any shadow of a doubt, that no member of my family could ever engage in such unsavoury conduct, I must appreciate the calls, goodwill messages, prayers from sensible, reasonable and intelligent Nigerians, who have assured that they condemn and firmly discountenance this latest episode of a perplexingly obsessive negative campaign of lies and calumny. While the apparent subject of the video has been identified and confirmed as not being a member of my immediate family, I do still enjoin the appropriate agencies to vigorously investigate the provenance and defamatorily circulatory sources of the video, in order to signal a firm cease and desist caution to the agents of calumny, and their directors, who truly should be impelled to recognise the appalling dangers that false news, misinformation and disinformation pose to statecraft, human decency and the collective wellbeing of society and the nation. Many people have had incredibly dangerous lies published about them, and the best they could do was phone around to all their friends and well-wishers and assure them that the stories were completely false. As cybercriminals evolve, through the dishonourable nature of those who, in exchange for lucre, propagate false and unsavoury fiction, I do believe that it's critical to counter their past, present and probable future cyberthreat tactics.
FROM October 28th, 2022
Displaced by devastating floods, Nigerians are forced to use floodwater despite cholera risk - Climate emergencies are a humanitarian and health crisis which affect us all. As Nigeria experiences complex and unpredictable climate risks which have led to extreme weather events such as the flooding in 34 out of the 36 states in the country, the compounding of existing vulnerabilities and inequities is putting millions of our people at immediate risk for disease, famine and death. More than 2.5 million people in Nigeria are in urgent need of structured humanitarian assistance, 60% of which are children, and with 1.3 million people displaced, there is a growing and heightened risk of waterborne diseases, drowning and malnutrition. The rise in cases of cholera is particularly worrisome as the WHO recently warned of the shortage of cholera vaccines, due to a strained global supply during a time of unprecedented rise in outbreaks worldwide, leading to the temporary suspension of the two-dose strategy. According to UNICEF’s Children's Climate Risk Index CCRI, Nigeria is now considered at 'extremely high risk' of the impacts of climate change, ranking second out of 163 countries. Children of 'extremely high risk' countries often face exposure to multiple climate and environmental shocks, paired with underlying child vulnerability, which my Wellbeing Foundation Africa midwives, nurses and healthcare teams are working daily on the frontline to mitigate by providing essential grassroots community-based Mamacare360 Maternity programming and intensified WASH services through our Reckitt, Dettol Nigeria, WBFA Hygiene Quest Curricula. The burden of climate-related health risks is inequitably and unequally distributed, and its worsening impacts are increasingly affecting the foundations and pillars of human health and wellbeing. Looking ahead, I welcome the African Summit which will be held alongside COP27 at Sharm El Sheikh, Egypt, in November, to dedicate financing sustainable development projects from the three climate commissions of the African Union (Congo Basin, Sahel Region and Island States). Climate change is the biggest health threat facing humanity, and if we do not address it immediately and scale-up response and recovery, it will potentially undo the last fifty years of progress in development, global health, and poverty reduction, while severely jeopardising the realisation of Universal Health Coverage.
FROM October 27th, 2022
As the 2022 Progress Report on the Every Woman Every Child Global Strategy for Women’s, Children’s and Adolescent’s Health (2016-2030) is released, I am reminded of my personal efforts, and my Wellbeing Foundation Africa’s commitment and support for the initiative since 2011, that has guided, conceived, birthed and delivered so many impactful frontline programs, to protect the promise and protect the progress of the United Nations Global Strategy #EWEC.
At this mid-point of actions towards achieving the 2030 Agenda for Sustainable Development #SDGs, we face growing barriers and challenges due to the COVID-19 pandemic destabilising access and availability of health services for nearly three years, a global climate emergency and various conflict zones - suddenly widening the gap of inequities that primarily impact the most vulnerable: women, children and adolescents, from maternal mortality to malnutrition.
My Wellbeing Foundation Africa will continue to prioritise, sustaining health investments and programming, particularly primary healthcare systems, improving food supply, collaborating across sectors including partnerships with the private sector, and advocating for the protection and promotion of gender equality - to reach and safeguard the rights and wellbeing of every woman, child and young person while addressing losses and building concrete progress to ensure we create a world where all have the opportunity to reach their full potential.

FROM October 25th, 2022
As World Polio Day passed yesterday, I reflected on how through global unity and commitment we have achieved a 99.9% decrease in polio cases since the 1988 World Health Organisation landmark resolution for the worldwide eradication of polio that was adopted at the 41st World Health Assembly.
In 2020 Africa was certified as free of indigenous wild polio, and while our progress is commendable, new outbreaks do continue to occur, reminding us that our efforts to deliver on the eradication of all forms of polio everywhere, is necessary, as until then no child is safe anywhere.
The Wellbeing Foundation Africa is committed to the international cooperation needed to protect innocent children from diseases, particularly polio, and empowers our on the field health care workers, including WBFA midwives and nurses to administer and achieve this humanitarian goal. Trusted frontline advocacy and education is necessary to overcome vaccine hesitancy, lack of access and misinformation.
I was encouraged to see the Global Polio Eradication Initiative’s GPEI 2022-2026 Strategy highlighted at the 2022 World Health Summit earlier this month, and that the polio pledging event will fund the roadmap and strategy to a healthier world for all children and mothers. Going ‘beyond’ while we build on our current investments will ensure no other life is lost to a preventable disease, and that life-saving services will enable mothers to have a positive experience of their pregnancy and young children to achieve their full developmental potential.
A big thank you to all the dedicated health care staff who safeguard every eligible child from polio, and continue to vaccinate despite significant challenges.
 📸 At Lugbe PHC, Abuja, 2018 - I like to personally attend African Vaccination Week which takes place every year in April, at any of our Mamacare HCF locations when I can, to build confidence and trust for the oral polio vaccine.
📸 At Lugbe PHC, Abuja, 2018 - I like to personally attend African Vaccination Week which takes place every year in April, at any of our Mamacare HCF locations when I can, to build confidence and trust for the oral polio vaccine.
FROM October 21st, 2022
During Breast Cancer Awareness month I am highlighting the importance of #frontline community midwifery to improve early detection and proactive behaviour against breast cancer. Breast cancer is the most common malignancy in women worldwide, and in Nigeria, it accounts for 22.7% of all new cancer cases among women.
In 2018, the Wellbeing Foundation Africa undertook a whole-country Rapid Cancer Assessment Research and Report in collaboration with partners Amref Health Africa, supported by Takeda International of Japan, the findings of which were presented to the Federal Ministry of Health. As the statistics prove, cancer is a personal story for everyone.
The Wellbeing Foundation Africa #midwives play a vital role through the trusting relationships they build with women and their superior knowledge and skills for recognising early signs. Through our midwifery-led MamaCare 360 Frontline Antenatal and Postnatal Education we reach women with the evidence-based self-care tools and practice to improve individual and family health outcomes.
Earlier this year myself and the WBFA team welcomed Laura Nels, Director JNJ Community Health Africa, and LSTM Global Programs Director, Dr. Charles Ameh to Abuja and Lagos - engaging with the Federal Ministry of Health, LSTM, Medicaid Foundation, The Real Visionaries and Johnson & Johnson Global Health and nationwide RMNCAH, Midwifery and Nursing Stakeholders at The Co-Creation Workshop: Understanding The Challenges and Gaps in Oncology Nursing, Mental Health Nursing and Midwifery Education In Nigeria. Together, we focused on building health workers’ capacity to provide specialised oncology services, midwifery, and mental health care, as it is essential to providing life-saving care to patients in healthcare facilities across Nigeria and to achieving SDG3.


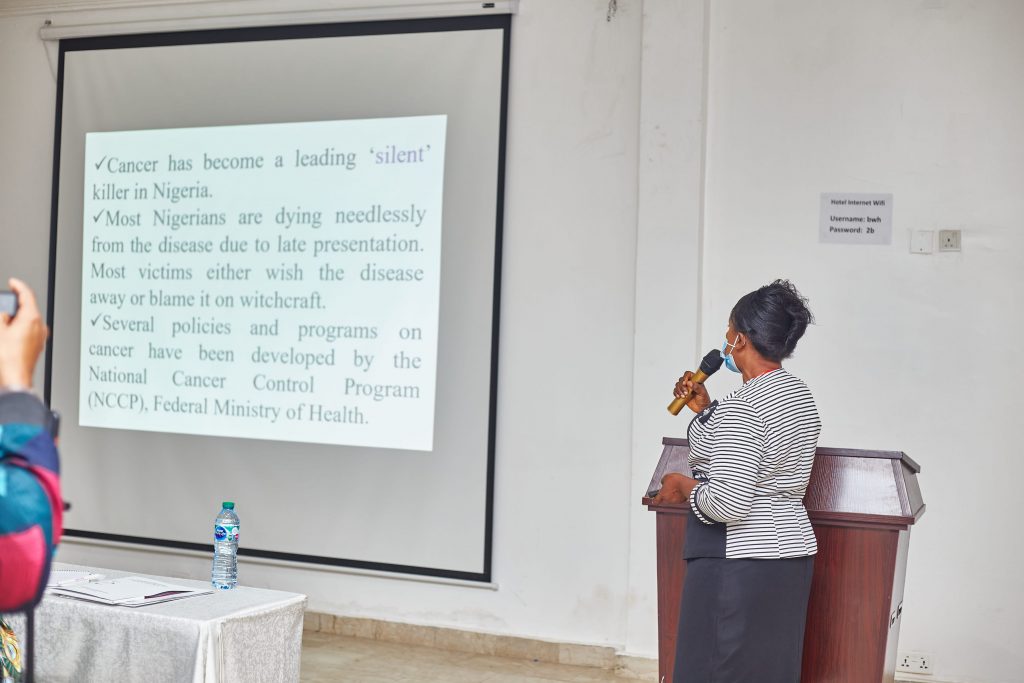 WBFA endorses the holistic recommendations of the WHO Cancer Report calling upon governments to strengthen and invest in cancer services, including prevention, screening, building capacities in health systems, training and retraining of relevant health workers such as midwives and ensuring palliative care for all by further connecting Primary Health Care facilities and cancer centres.
We may not cure breast cancer today, but we can contribute to the battle against it by bringing awareness and getting checked!
#FrontlineFriday #BreastCancerAwarenessMonth
WBFA endorses the holistic recommendations of the WHO Cancer Report calling upon governments to strengthen and invest in cancer services, including prevention, screening, building capacities in health systems, training and retraining of relevant health workers such as midwives and ensuring palliative care for all by further connecting Primary Health Care facilities and cancer centres.
We may not cure breast cancer today, but we can contribute to the battle against it by bringing awareness and getting checked!
#FrontlineFriday #BreastCancerAwarenessMonth
FROM October 17th, 2022
As I mark the International Day for the Eradication of Poverty today and reflect on World Food Day which took place yesterday, the message has never been clearer: no one should be left behind, and dignity for all must be achieved. The increase of interconnectedness through our globalised world represents a chain of attachment and impact which require the implementation of holistic solutions to develop long term inclusive resilience for food security, health systems and climate adaptation to ensure multidimensional poverty is addressed, and peace, protection of the planet and prosperity are sustainably established #SDGs. Since founding the Wellbeing Foundation Africa in 2004, we have worked to improve health and wellbeing outcomes through dedicated frontline health, nutrition and education programming and agrifood advocacy to combat malnutrition and tackle inequities, believing that to #feedthefuture and #GrowNigeria, every person deserves the opportunity to #thrive. Around the world, families are suffering the domino effects of challenges that know no borders, with the consequences of COVID-19, inequality, conflict, and the climate crisis, such as the current Nigeria floods - an overwhelming disaster that is ruining the agriculture and natural resources needed for the survival of many. With the extreme rains in Nigeria leaving 600 killed and 1 million more displaced, global solidarity is immediately needed to build a sustainable world where everyone, everywhere has regular access to enough nutritious food, and that we deliver on our commitments to social justice, ending poverty, healing our planet and the empowerment of the marginalised. It is our shared responsibility to eradicate poverty, combat all forms of discrimination and prioritise the right of all people to food, nutrition and equality with dignity for all in practice. #EndPoverty #IDEP2022 #GlobalGoals
View this post on Instagram
FROM October 14th, 2022
I am delighted today to welcome our health, education, water, climate and environment partners and national stakeholders at the commencement of our new community of healthy hygiene practice at national scale. The Wellbeing Foundation Africa partnership with Reckitt and Dettol Nigeria, in progression of our Clean Nigeria Initiative Commitments endorsed by the Ministry of Water Resources, is pleased to announce the launch of our Hygiene Quest Project, a comprehensive hygiene curriculum and strategic programme designed to promote and implement proper handwashing and water sanitation and hygiene techniques, including reducing open defecation in schools, healthcare facilities across our #Mamacare360 Antenatal and Postnatal Maternity Centres, and corresponding Cluster Communities through Abuja, Lagos and Kwara States. As we commence this important project, currently 23% of the Nigerian population still practices open defecation, with less than 8% of the population in Nigeria being able to access and practice safe handwashing. Therefore our interactive and engaging approach aims to tackle these challenges sustainably through grassroots core education, access and training. Escalating and cascading our shared efforts ahead of Global Handwashing Day this week, our union for universal hand hygiene is accelerating the Hygiene Quest outcome and the United Nations Sustainable Development Goals, while journeying to reach 6 million children in Nigeria by 2025. Handwashing is an effective and affordable way to prevent diseases and save lives. The Wellbeing Foundation Africa looks forward to scaling access to quality personal social health and hygiene education and information in schools, communities and within healthcare facilities, with Reckitt and Dettol Nigeria through Hygiene Quest, to drive lasting community behavioral change, and create a healthier and more equitable society for all. Data: UNICEF Water, Sanitation and Hygiene National Outcome Routine Mapping Report, WASH Norm 2021 #WashforWellbeing💦 #SDG2030#UniteforUniversalHandHygiene #WashYourHands#HandHygieneForAll
FROM October 11th, 2022
At #WISH2022 I had the privilege to participate in timely discussions regarding mental health and wellbeing, while assessing the implications of the pandemic. Today on #WorldMentalHealthDay, and with the evidence-based research from WISH Qatar and the Qatar Foundation, we have a powerful opportunity to revitalize our efforts to protect and improve mental health for all. #Mentalhealth does not discriminate and requires investment in financing, training, policy and legislation, research and advocacy. Speaking to H.H. Sayyida Basma Al Said, Founder Serenity Muscat, we must raise awareness and take action to build the capacity for health, education and social protection, particularly in early childhood development, and ensure the resources not only exist but are accessible. My Wellbeing Foundation Africa targets public standards for promotion, prevention, treatment and wellbeing policies for childbearing women and their families through our HCF, schools and communities based Mamacare360 Maternity and Primary & Adolescent #PSHE #WASH programming which provide opportunities for safe space conversations, and referrals, with our professional midwives, nurses and coaches. As I continue to advocate for rights-based, multisectoral legislation, plans and policies, I dearly wish that Presidential Assent for the Nigeria #MentalHealthBill will soon be forthcoming, especially as it is believed over 40% of Nigerians are suffering in silence. As this barrier to accessing mental health services remains a challenge compounded by cases of post traumatic stress compounded by the ongoing instability and insecurity in regions due to insurgency, kidnapping and attacks; now is the time to strengthen mental health care provisions and protections, through a community-based network of accessible, affordable and quality services and supports. We must deepen the value and commitment we give to mental health as individuals, communities and governments, and work with stakeholders to create a world in which everyone has an equal opportunity to enjoy mental health.
FROM October 6th, 2022
This week I have been delighted to join the World Innovation Summit for Health 2022, an initiative of the Qatar Foundation, held in Doha this year, as a speaker, moderator and participant. Born through the need to convene global experts to look for collaborative and innovative solutions to tackle global health challenges – WISH Qatar and the Qatar Foundation are inspiring drivers of change, dedicated to uplifting community development for all, established and invested in evidence-based ideas and practice. As a moderator, I had the pleasure of joining H.E. Jeannette Kagame – First Lady, Rwanda, H.E. Fatima Maada Bio – First Lady, Sierra Leone, and H.E. Vivian Torrij – Former First Lady, Panama, for an invigorating conversation on Child and Maternal Health which assessed the global efforts on reducing maternal mortality and newborn deaths, to achieve the United Nations Sustainable Development Goals, through collaborative scientific research, trusted frontline work, and policy reform. As a panellist, I had the great opportunity of Promoting Child Wellbeing: Lessons from COVID-19 alongside H.H. Sayyida Basma Al Said, Founder, Whispers of Serenity Clinic, Oman Professor Muhammad Waqar Azeem, Inaugural Chair of Psychiatry/Child Psychiatry Sidra Medicine, Victoria Hornby, CEO, Mental Health Innovations, UK and Moderated by Luisa Baldini of BBC. We discussed in-depth the long-term psychosocial and mental health implications for our children and adolescents due to the disruption of the pandemic, and how we can mitigate and address the adverse effects of the pandemic and draw out lessons for policymakers across the globe. We must embolden our children, while we catalyse investment, from health literacy, programming and policy to begin and protect from birth to age, addressing their unique needs and resources at every phase in life.
FROM October 1st, 2022
Happy #IndependenceDay! 🇳🇬 Today marks the 62nd anniversary of Nigeria's proclamation of independence from British rule on 1 October 1960. In 1914, the Southern Nigeria Protectorate was combined with the Northern Nigeria Protectorate to create the Colony and Protectorate of Nigeria, which has the borders of modern-day Nigeria. By the late 1950s, the call for independence of territories in Africa, and the affirmation of the Nigeria Independence Bill at the House of Commons on 15 July 1960 led to Nigeria being granted independence on 1 October 1960 as the Federation of Nigeria. Three years later, the constitution was amended and the country was declared the Federal Republic of Nigeria with Nnamdi Azikiwe, previously Governor-General, as the first President. On this historic day in 1960, Lieutenant David Ejoor, who later became the Chief of Army Staff, had the honor of commanding the guard at the midnight flag raising ceremony. On 1st October 1960 #Nigeria entered its new status of independence, not after commotion and strife as some other colonial territories had done, but rather after practical experience of the federal system which we decided to adopt, and with general agreement, to maintain, wishing to be independent and to be democratic and also incorporated into our Constitution a carefully drawn up Bill of Rights. Nigeria willingly accepted a Parliamentary system with reasonable and natural adaptations to our own traditions, including, as an essential part of parliamentary democracy, that there should always be a respected and vigorous opposition, freely and fully entitled to express their point of view. Let's renew our vision with replenished hopes and prayers for Nigeria, the most populous nation in the continent of Africa's extraordinary diversity and unity in race, in religion and in social and economic development.
FROM September 29th, 2022
Transformative solutions to achieve gender equality and empower all women and girls. #UNGA has consistently been the principal multilateral diplomatic setting for global cooperation from climate goals, to health equity, but as inequality worsens, exemplified by the repression of women from Ukraine to Iran; it is clear that the impacts of crises are never gender-neutral, and that there is still much to be achieved regarding women and girls recovery, resilience and representation. Preventing and ending violence against women and girls while improving equity require women’s leadership, prompt pledges and direct resources devoted to achieving a sustainable future where all women and girls are safe with opportunity. Therefore I am grateful that the newly created United Nations General Assembly Platform of Women Leaders is now established to place gender equality at the forefront of this multilateral arena. As the 77th United Nations General Assembly comes to a close, I appreciate my Global Office’s attendance, as my full executive and representative emissaries, a delegation that is strengthening collaborations and work with longstanding allies and taking part in complex and timely deliberations, which inform our humanitarian agenda for the coming year. As we face interlocking challenges, it is crucial for the woman and girl child perspective to be prioritised effectively, decisively and inclusively, and in the Decade of Action, the Wellbeing Foundation Africa is committed to achieving #SDG4 and advocating for the human rights of women and girls around the world, as we embolden them, improve access to services, strengthen laws and policies, to ensure accountability and transparency.
FROM September 24th, 2022
September 2022: Youth-driven design and research nonprofit YLabs and the London School of Hygiene and Tropical Medicine in partnership with the Wellbeing Foundation Africa announced the Children, Cities, and Climate Action Lab (CCC Action Lab) commitment at the Clinton Global Initiative’s September 2022 meeting in New York City. In further collaboration with, C40, and Urban Better, the CCC Action Lab is an initiative to accelerate healthy decarbonization in cities through youth leadership and action. The world is currently on track for catastrophic levels of warming that threaten to undermine the health of people everywhere, especially amongst the most vulnerable.
FROM September 23rd, 2022
100 years of working towards a world where every childbearing woman has access to a midwife's care for herself and her newborn! As the Inaugural Global Goodwill Ambassador of the International Confederation of Midwives for two terms (2014-2020) I am thrilled to celebrate with #ICM as they mark their 100-year anniversary alongside the 77th United Nations General Assembly in New York City. My Global Office Delegation attended the Centennial Commemoration and were elated to discuss and highlight the key achievements of #midwifery this past century, connect with incredible health partners and aid in developing the vision for the next 100 years. Addressing the unmet needs of women and their families must remain a constant priority, and my Wellbeing Foundation Africa Foundation will continue to empower our #frontline #midwives so they may efficiently #access, #educate, #counsel and #care for #mothers as trusted community health workers. #ThriveThursday #UNGA77
View this post on Instagram
FROM September 21st, 2022
End racism. Build peace. As I mark #PeaceDay, I commend the UN Peacekeeping call to strengthen the ideals of peace to build communities where all are afforded equity and the opportunity to thrive. Persistent injustice due to bias, discrimination and racism hinders fundamental human rights, perpetuates unrest, undermining democracy. My Global Office is addressing this escalating crisis and pursuing peace at the 77th United Nations General Assembly this week, as they attend the Concordia Annual Summit and Devex #UNGA77 Halfway to 2030 today, advocating for the rights and dignity of people while building a practical pathway to a fairer world #SDGs. Inspired by the words of #flotus, the First Lady of the United States, Dr Jill Biden at the #ConcordiaSummit, and as direct conflict and animosity destabilize societies across the globe, with health and economic challenges surging, we must convene to dismantle the systemic barriers which hinder our progress towards equality, empathy and a peaceful planet as we are all connected.
FROM September 19th, 2022
The Power of Collective Collaboration: Transformative Solutions and Education for Change From the #frontlines to global impact, my teams are building solutions and transforming education. Yesterday, my Global Office continued my commitments at the 77th United Nations General Assembly, engaging with MIT Solve as social impact leaders, while my Kwara Office is advocating with Chevening FCDO to create an educated future; a Wellbeing Foundation Africa commitment to achieving the Sustainable Development Goals progress. With a mission to drive innovation to solve pressing world challenges, I am honoured to be an MIT Solve judge for Equitable Health Systems. Positively affecting over 150 million lives to date, affordable, accessible, and high-quality health systems must serve all equitably. My Global Office shared their expertise on people-centred health infrastructure, from the ground up, mentoring Solvers and supporting innovative partnerships to improve health outcomes. This continued empowerment of transformation for the better took place on the ground today as well, as the Wellbeing Foundation Africa, Kwara Office & British Deputy High Commission Courtesy Call to discuss the Chevening Scholarships Programme with Mr. Wale Adebajo, Political Advisor British High Commission in Nigeria, and the Chevening team as they introduce the program to Kwara State. Through our programmatic community work which has been supported by the High Commission and British Development Agencies over decades, we have expanded the opportunity to access learning skills, mobilising and elevating emerging Nigerian leaders. By solving together, we can tackle the issues of our rapidly changing world, promote education, and learn to live together sustainably.
FROM September 16th, 2022
As the 77th Session of the United Nations General Assembly opened on Tuesday, I welcomed the words and targets of UN Secretary-General Antonio Guterres opening remarks at the first full offline meeting since the pandemic's onset, calling for solidarity among member states to address common challenges, such as ensuring equity in healthcare. Global health and emergency response are a priority, as all Member States accelerate equitable progress toward implementing Universal Health Coverage by 2030 #UHC2030, to create a safer, fairer and healthier world. By demonstrating unity and solidarity, we can build new partnerships, share best practices and save lives. With frontline-focused dedication, integrity and authentic purpose, my global team will continue the multilateral discussions at #UNGA across the full spectrum of international issues covered by the Charter of the United Nations. I look forward to the key decisions which will advance peace, human rights and sustainable development for all. #FrontlineFriday #ConcordiaSummit #WHOFoundation #PMNCH #ClintonFoundation #BusinessFightsPoverty #SDGAction #unitednations
View this post on Instagram
FROM September 10th, 2022
Today on World Suicide Prevention Day #WSPD, I commend the efforts of the International Association for Suicide Prevention and WHO in focusing attention on reducing stigma, raising awareness, and implementing support to prevent the rise of this serious global health concern. The profound grief and impact of this crisis affects the wellbeing of humanity, with an estimated 703,000 people a year taking their own lives around the world, and for every suicide, a likely 20 other people making an attempt, with many more having serious and dangerous thoughts. Through well-informed action, we can create supportive safe spaces which aim to inspire confidence and the light of hope in all ages. Suicide prevention is a priority public health agenda, especially as we aim to expand evidence-based programming and advocate for the accessibility of mental health services. I hope this is a reminder that there is always an alternative, and that together we can all create hope through action and #bethelight. #WorldSuicidePreventionDay
FROM September 9th, 2022
Inclusive, equitable and quality education is a human right which must be protected. On this International Day to Protect Education from Attack, and as International #LiteracyDay took place yesterday, I am highlighting the importance of literacy as a matter of dignity, and education to be safeguarded particularly for children and youth in conflict zones who remain among the most vulnerable. The Wellbeing Foundation Africa aims to advance the United Nations Sustainable Development Goal #SDG 4, and Safe School Declaration to secure a sustainable future and create a healthy society by implementing #frontline intervention through our Adolescent #PSHE #WASH programming which emphasises the role schools play in providing a safe space for children, where they can be protected from threats and crises, from conflict to health. Education and literacy are essential skills that save lives. Governments, private sector agencies, and humanitarian organisations must partner to provide secure and feasible measures to ensure access to safe education is rarely impeded. Only then can these transformed literacy learning spaces begin to break the cycle of inequality, hostility and poverty. #FrontlineFriday 📸 #FlashbackFriday Wellbeing Africa Schools Furniture, Textbooks and Learning Materials Empowerment Program Donations To 32 Primary and Secondary Schools in Kwara State, 2007.
FROM August 27th, 2022
It is with the greatest sadness that I learn of the passing of Her Majesty Queen Elizabeth II.
The Queen was a true and sovereign inspiration, the embodiment of unwavering duty, who truly exemplified the highest form of courage. Her powerful influence, ruling for longer than any other Monarch in British history has created an immeasurable impact which continuously rings true to the noble motto “I Serve”.
As a young woman, I recall meeting Her Majesty and being enchanted by her devotion, passion and care for all. The example and continuity she set as a profoundly respected leader will be deeply missed, but I know her legacy will set a high benchmark for monarchic service and continue to embolden future generations.
My thoughts and prayers are with people across the United Kingdom and Commonwealth, and may Almighty God strengthen and comfort the Royal Family during this solemn and distinguished hour.
“I declare before you all that my whole life whether it be long or short shall be devoted to your service and the service of our great imperial family to which we all belong.” Her Majesty The Queen, on her 21st Birthday, 1947
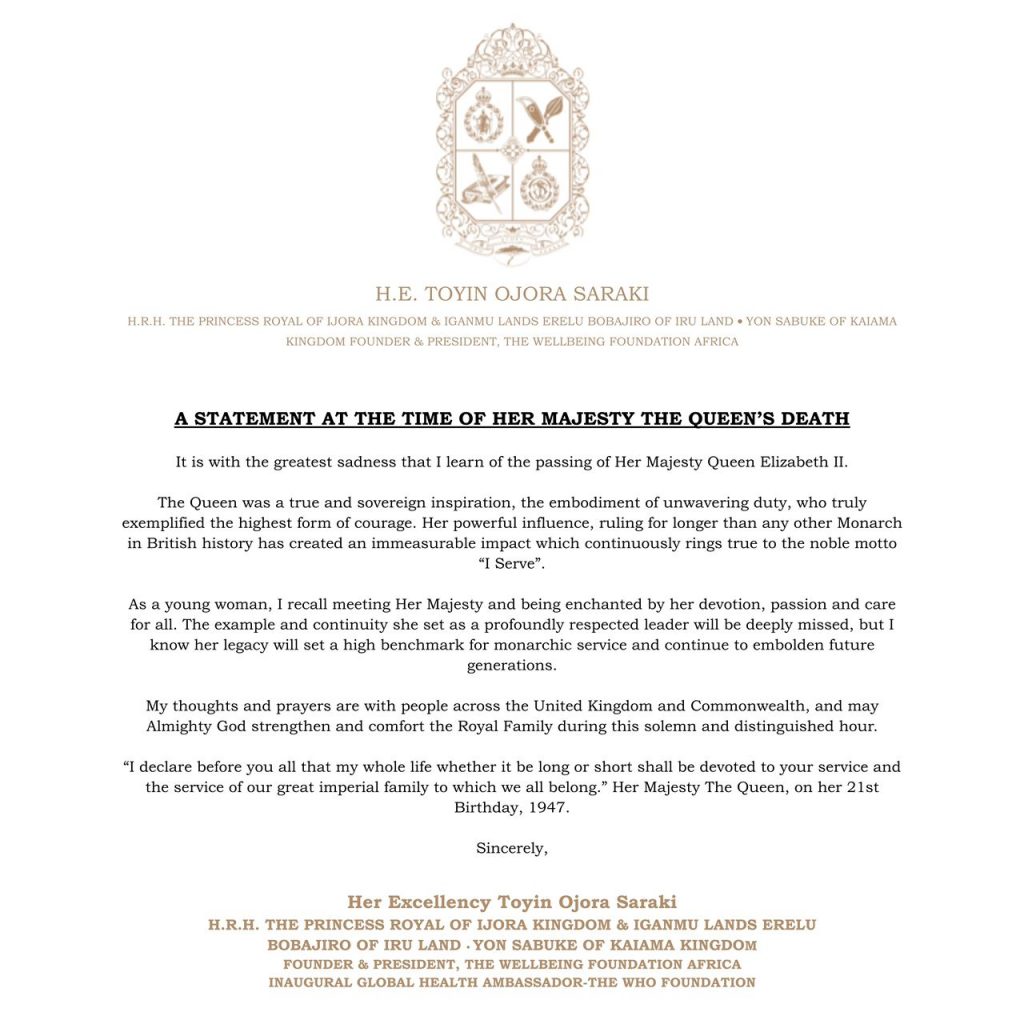
FROM August 25th, 2022
Today I had the pleasure of joining the 13th International Conference on the Maternal Child Health Handbook, alongside Her Imperial Highness Crown Princess Akishino, WHO Special Advisor to the Director General, Prof. Peter Singer, Prof. Miriam Khamadi Were, UNICEF, UNFPA, healthcare, policymakers and research representatives from Nigeria, the Netherlands, Pakistan, Bangladesh, and Ghana, to mention a few, with a focus on promoting health equity and making mothers feel like visible primary partners in their and their child's health journey. Since 2006, when the WBFA committed its efforts to the development and deployment of home-based health records and handbooks in Nigeria and Africa, we have tenaciously held to the mission that accurate and accessible health information both educates, guides and delivers measurable benefits for every woman, child and family. The #MCH Handbook is a home-based health record and information tool which supports women throughout their pregnancy, delivery, and postnatal period, extending to the first few years of the child's life. Introduced in more than 30 countries already, by empowering parents through being an accessible source of information, the handbook bridges communications gaps between them and health professionals, emboldening them to be actively involved in the decision-making and management of their family’s health. A very intense sharing and learning experience, the conference is a powerful affirmation of the core vision of my Wellbeing Foundation Africa mission from inception. Ensuring the continuity of care and providing health education to families leads to social cohesion and holistic maternal and child care which is highly effective as prevention and protection. I look forward to continuing to discuss, strategise and champion the immediate prioritisation of attainable and equitable maternal care as the conference continues tomorrow, and I thank today’s moderator Dr. Shafi Bhuiyan MBBS, MPH, MBA, PhD and Prof. Yasuhide Nakamura for their organisation and guidance throughout the day! #MakingMeVisible #DallaLanaSchoolofPublicHealth #UofT
FROM August 24th, 2022
Yesterday on International Day for the Remembrance of the Slave Trade and its Abolition, as the world reflected on the tragedy of the slave trade, I am remembering and honoring those who campaigned for freedom and defied the cruelty of oppression. Sadly, modern slavery still persists, with transatlantic trafficking continuing to have a profound impact on the lived experiences of vulnerable communities across the globe. Slavery was and still is a violation of #HumanRights, resulting in brutal labour, sexual and inhumane exploitation, and an enduring pernicious legacy of racism. The concept of equal and unconditional dignity can only be achieved universally once the deconstruction of racism takes place, particularly with the younger generation, liberating themselves and future generations from the prejudicial ignorance and constructions of the past. The Wellbeing Foundation Africa advocates and teaches through our Adolescent and #PSHE #WASH programming the importance of developing a social and emotional sense of values, respectful dialogue, peaceful tolerance, and mutual understanding which combats all forms of discrimination, including those based on gender. We take every opportunity to help our youth to understand Africa’s history, learn about the destructive effects of colonisation, and make the connection between the slave trade and the widespread discrimination and racism that characterises today’s society. Collective intergenerational efforts to fight injustice is essential to dismantle political, economic and structural power imbalances rooted in enslavement which still deny equality of opportunity. Let us work together to inspire every generation to build societies based on integrity and solidarity, so that we can bring an end to modern slavery. #TeenageTuesday #WASHWednesday
FROM August 22nd, 2022
“No violence can be justified in the name of religion.” - Pope Francis As this new week begins with the International Day Commemorating the Victims of Acts of Violence Based on Religion or Belief, I totally agree that upholding peaceful assembly and the right to freedom of association, especially to strengthen democracy and combat intolerance is an important mission for us all. Interdependent, interrelated and mutually reinforcing, the open, constructive and respectful discussion of interfaith and intercultural expression and dialogue is a human right. As acts of violence increase towards religious communities and minorities globally, we must immediately condemn, provide victims with the appropriate support and assistance, work together to enhance the implementation of existing legal regimes to protect individuals and increase efforts to expand human rights education. My Wellbeing Foundation Africa, through our grassroots advocacy and frontline programming, is an intentional and strategic #ForceForGood and is #CommittedToCaring, by promoting #FreedomOfReligionOrBelief, as enshrined in article 18 of the Universal Declaration of #HumanRights @UN, and facilitating empowering and considerate dialogue between various groups. Today serves as a reminder of the need to protect the infrangible right of religious freedom and the consequences when a country fails to do so. Let us vow to do better and create societies that are free from violence. #ToyinSaraki #Alaafia #Wellbeing #MaternalMonday
FROM August 19th, 2022
Just as it takes a village to raise a child, we must collectively come together to support those facing humanitarian crises. As we face record-high humanitarian needs around the world this World Humanitarian Day #WHD2022, it is with deep gratitude that I recognize and praise the dedication of essential frontline staff, who deliver lifesaving assistance without hesitation each day. I am honoured to thank our various Wellbeing Foundation Africa partner stakeholders and governmental organizations such as UNHCR, UNFPA, UNDP, UNEP and stand for the safety and security of humanitarian workers and for principled humanitarian action. As Inaugural Global Health Ambassador of WHO Foundation, I echo the need for our global health community and private sector partners to power health emergency preparedness to reach true health equity. #Ittakesavillage to support people in need, and health-care workers, including the WBFA #midwives #nurses #doctors and #staff are central to humanitarian action. They go wherever vulnerable people are. 📸 Adagom Refugee Resettlement Community, Cross River State, Nigeria 2021 #FrontlineFriday #WorldHumanitarianDay
FROM August 17th, 2022
I started the working week with a timely meeting of essentially glad tidings in conversation with UN Women Nigeria Representative, Madame Beatrice Ekong, convened by AWLN Chair, Professor Funmi J. Para-Mallam mni, focusing clearly on the continued and future impact of inclusivity, empowerment, local ownership and integrity for women and girls across the continent. It was a pleasure to join the like-minded and spirited women of the African Women Leaders Network Nigeria Steering Council, a ground-breaking movement implemented with the support of the Office of the African Union Special Envoy on Women, Peace, and Security, and of the United Nations Entity for Gender Equality and the Empowerment of Women UN Women. In line with the Africa Agenda 2063 and the 2030 Sustainable Development Goals, the AWLN Nigeria Chapter discussed the vision of the “Africa We Want”, one where women and girls are supported to reach their rightful roles in all spheres of life. Working together through our network of over 200 diverse women leaders in media, politics, diplomatic corps, academics, research, civil society, private sector, young women, rural women and women in the diaspora, our targeted aim toward development, governance, peace and stability, economic empowerment and women's access to finance directly aid in achieving #SDG Goal 5. Empowering women and girls and achieving gender equality are crucial to my Wellbeing Foundation Africa's safe childbirth and safer childhood targets as we work towards improving social determinants, creating inclusive, open, prosperous and healthy societies. Together, with the AWLN, and in support of the delivering as One UN approach, our active engagement and advocacy aspire to share resources, opportunities, solidarity, and partnership for mobilisation of an equitable future. #GenerationEquality
FROM August 12th, 2022
Today on International Youth Day 2022, myself and the Wellbeing Foundation Africa are reiterating and amplifying our commitment to taking action and achieving the Sustainable Development Goals across all generations to ensure no one is left behind. Intergenerational solidarity is essential for the positive and progressive development of society, especially as the bias of ageism continues to go unaddressed in health and human rights, leading to a lack of fulfilled potential. Reflecting on the Global Report on Ageism launched by the United Nations in March 2021, our youth continue to face adversity and barriers across employment, political participation, health and justice. The key to shaping these spheres to be accessible and brave spaces will manifest from an engaged and productive intergenerational intervention strategy, increasing the strength and unity to achieve #SDGs for all. With a sustained focus and mission anchored primarily on the successful delivery of goals 3, 5 and 6, good health and wellbeing, gender equality and #WASH, WBFA frontline programming educates, empowers, and advocates for open communication and community and social connectedness across all ages, young and old alike. We encourage the joining of forces, collaboration and fight against discrimination in hopes of an equitable and inclusive future that listens to elders while including youth at the table. Let’s aim to build back better by leveraging all generations’ wisdom, knowledge and lived experiences.
View this post on Instagram
FROM August 10th, 2022
I am honoured to be invited by UNDP to lend my voice to, advocate for, and champion #ImagineNigeria. As the Imagine Nigeria Report, which presents the findings of a multi-stakeholder foresight exercise led by the UNDP, launches today at the State House, Abuja, I am envisioning a Nigeria where we collectively work together to create a progressive, prosperous and peaceful nation. Imagine Nigeria considers the multiple pathways in which Nigeria can further develop in the promise of a flourishing and bright future. With over 300 participants from all regions of Nigeria and the diaspora, who put in over 6,000 hours of consultation, research, analysis and scenario-building processes, the report aims to now mobilise various stakeholders globally for action. As our world rapidly changes from technology to urbanisation, and faces challenges such as the pandemic, it is time to act quickly and act together. Through assessing trends, Imagine Nigeria shares four potential scenarios to shine a critical light on future uncertainties, and then recommends five pillars for advocacy and action, from now until 2050, to witness transformation and engender a new level of commitment and cooperation within Africa. Building trust is the key to a thriving Nigeria and must be the basis of all engagement, policy and operation. Through shared hope, values and commitments, we can create a new national narrative that builds a culture of innovation, catalyses the green economy, and leads Africa. The Wellbeing Foundation Africa and I look forward to continuing to facilitate this change, through empowering communities with the power to act, by sharing knowledge and resources to uplift Nigeria. #ImagineNigeriaChallenge
View this post on Instagram
FROM August 9th, 2022
As I mark International Day of the World's Indigenous Peoples, I am reminded of a young group I met in September 2019 when I honoured the invitation of the Independent Midwives Association of Namibia, and also of the efforts and aspirations of a young traditional cultural dance group I met at the United Nations headquarters in New York that same year. These encounters exemplified the role of indigenous women and girls in the preservation and transmission of traditional knowledge, particularly when it comes to health and societal wellbeing. Indigenous knowledge in the sphere of health, often first present as traditional birth attendants, who aim to fill the gap of inadequate or completely absent public services. From providing their communities with essential information on sexual and reproductive rights to #GBV, generations of indigenous women have passed down critical skills and practices to help mitigate the effects of inaccessible healthcare. The Wellbeing Foundation Africa and I aim to empower indigenous women and girls with training and modern practices to shape the evolution of trusted traditional wisdom with modern techniques being applied for good. The transmission of ancestral knowledge and advocacy which takes place as the carers of society are crucial, but we must also equip these knowledge keepers, leaders and human rights defenders with contemporary education, #WASH, and autonomy to combat harmful traditional practices, and tackle the rise of intersecting levels of discrimination based on gender, ethnicity and socioeconomic status. At home in Nigeria, our WBFA community midwives continue to work towards achieving the #SDG2030 Goals and WHO Global Targets 2025, to improve maternal, infant and young child health outcomes, while viewing wellbeing as both an individual and a collective right, strongly determined by community, land and the natural environment, as conceptualised by indigenous peoples. We must acknowledge, strengthen and support indigenous midwifery through healthy policy and integration while creating opportunities for upskilling and reskilling. Let’s reclaim the role of these heroines! #IndigenousPeoplesDay #TeenageTuesday
FROM August 6th, 2022
In a first-ever-in-Nigeria pioneer partnership project, and aligned with the society pillar of Medela Cares, the Wellbeing Foundation Africa #frontline heroes, midwives and doctors are improving the #breastfeeding support offered to new mothers in Nigeria, by delivering NICU-specific education and training on the value of human milk and how to build sufficient milk supply for long-term lactation and breastfeeding. As committed members of the United Nations Every Woman Every Child Initiative, together we aim to drive change and improve health outcomes for generations to come. Research has shown that 47% of the deaths of children under 5 years occur in the first 28 days of life, and these deaths are a result of preventable diseases that can be avoided through improved nutrition with the mother's milk. Collaboratively, my Wellbeing Foundation Africa through our #midwives have introduced, and continue to deploy, educate and facilitate the use of Medela Cares lactation strategy and tools by leading training sessions for healthcare workers and mothers, in the 3 focal project states of Lagos, Kwara and Abuja; supporting the timely initiation of breastmilk expression, improved the capacity of use of breast pumps within facilities, promoted exclusive breastfeeding and maintenance to empower mothers to nurture their babies through optimal nutrition. Mother’s Own Milk is essential, and the lactation care provided to mothers must acknowledge its importance of it to ultimately improve infant feeding and health outcomes in Nigeria. #WBW2022 #WorldBreastfeedingWeek
FROM August 4th, 2022
#Breastfeeding provides food security to infants from the very beginning of life, promoting overall family health and wellbeing. #Nutrition is essential to #nurturing, and is linked to achieving the United Nations Sustainable Development Goals, contributing to global maternal and infant survival. Breastfeeding is an essential part of good nutrition, food security and reduction of inequalities, and through engaging with valued partners along the #warmchain, my Wellbeing Foundation Africa is strengthening the capacity for transformative change and equality. Placing the mother-baby dyad at the core of our programming and development ensures an optimal level of continuum of care, and that mothers are empowered with a more fulfilling and effective breastfeeding experience. WBFA’s Mamacare+N, is a maternal, newborn and child health service, with a focus on women and girls, supported by our forward thinking partners UNFPA, UNFPA Nigeria and Nutrition International, encompassed key interventions and access in family planning, iron and folic acid supplementation, and nutritional advice, as they mutually reinforce each and contribute to ending intergenerational cycles of poor health and poverty. From drawing up strategies for the protection, promotion and support of nutrition from and during breastfeeding, including monitoring and evaluation to inform national analysis, targets and policy, we must acknowledge that #breastisbest!
FROM August 2nd, 2022
It is well proven that breast milk is the optimal source of nutrition for babies, yet the long-term benefits are lesser known. Associated with healthier adolescents, #breastfeeding for 6 months or longer, compared to less than 6 months or not at all, has shown improved cognitive performance, socio-affective responding and physical wellbeing from childhood into adolescence. In other words, healthy, happy, breastfed babies create healthier and more productive teenagers. To empower early childhood development through improved nutrition starting with early and exclusive breastfeeding, my Wellbeing Foundation Africa has executed strategic public-private and philanthropic investments to improve breastfeeding across Nigeria. Between 2017 and 2020, the WBFA Alive and Thrive, McCann Health, FHI360 and Gates Foundation consortium promoted appropriate Infant and Young Child Feeding #IYCF, and encouraged optimal breastfeeding practices at over 370 private medical facilities in Lagos and Kaduna States. Our #Mamacare360 Midwifery-led #ANC #PNC programme continues to promote early initiation and exclusive breastfeeding, providing the lactation support required for mothers and healthcare facilities across Nigeria, activating and actualising the WHO and UNICEF’s Baby-friendly Hospital Initiative's "Ten Steps For Successful Breastfeeding" in order to support mothers and newborns. These steps highlights the support which the mother needs while the support healthcare and hospitals should provide to all mothers and their newborns after birth. As we work to achieve a world where breastfeeding is the cultural norm and where mothers and families are enabled to feed and care optimally for their infants and children, let us continue to amplify and reflect on how breastfeeding contributes to a brighter and better healthy society for years to come. #WBW2022 #TeenageTuesday #WorldBreastFeedingWeek2022
FROM August 1st, 2022
As we celebrate a new month, with the beginning of #WorldBreastfeedingWeek2022 this #MaternalMonday, commemorating the Innocenti Declaration signing on the 1st of August 1990, we focus on protection, promotion and support of Breastfeeding. Since then and continuously progressing: WBFA and I prioritise the advancement, strengthening and maintenance of breastfeeding, by providing the universal right of Respectful Maternity Care #RMC, aligned with #SDG 3, ensuring healthy lives and promoting wellbeing for all, through our Mamacare360 programme which improves maternal and infant survival, health and wellbeing throughout the antenatal, birth and postnatal periods. Our Wellbeing Foundation Africa Mamacare Baby Friendly Antenatal and Postnatal, which began in 2015, continues to reach mums daily in 8 states, while our Mamacare Digital Whatsapp keeps mums in contact with midwives as lactation counsellors across Nigeria. Each day we do more than advocate to step up education and support for breastfeeding by understanding, implementing and adhering to the World Health Organisation and UNICEF Global Strategy for Infant and Young Child Feeding, the WABA Global Warm Chain of Support for Breastfeeding and quality WBFA Mamacare360 #midwifery which was launched on World Breastfeeding Day 2011. Breast is always best. Let’s foster a cohesive breastfeeding movement and enable equitable environments for mothers and families to be empowered, to optimally, safely and actively breastfeed their baby. #WBW2022 #WarmChain #HappyNewMonth
FROM July 30th, 2022
As our world becomes more globalised and connected through the expansion and use of technology, the atrocity of human trafficking has morphed and consumed our online platforms and cyberspace. On World Day Against Human Trafficking, I am highlighting how this horrific crime, which attacks the rights and safety of a person, is severely affecting women and girls, who already represent the mass of trafficked persons globally. From conflicts to climate change and particularly during the pandemic, we have seen the vulnerability and isolation of humanity. Being online was a haven for many, allowing them to connect with family and friends or continue their education. Yet, human traffickers have taken advantage of this time in cyber history by using sophisticated technology to identify, track, control, degrade and exploit victims. That is why my Wellbeing Foundation Africa has always emphasised the need for technology awareness, understanding, security, and education on this topic through our Adolescent Skills and Drill programme. As trusted frontline staff, we teach our youth internet safety to prevent and mitigate the risk of them falling victim online and transparently communicate the dangers they may face. Our WBFA #midwives continue to protect, support and are an ever dependable network for our youth to reach out to if they are uncertain or feel anxious regarding a cyber situation. Technology may enable human trafficking to a degree we have yet to fully fathom, but it can also be a critical tool in fighting against it. Through the collaboration and committed participation of governments, law enforcement, regulators, the private sector and civil society, we can invest in policies and innovative technology-based solutions to ensure a safe and secure space for all online. I look ahead to the United Nations Global Digital Compact at the 2023’s Summit of the Future, to standardise policy around good governance in the digital space. Our use of technology has great opportunity, we must harness its power, to protect our communities, and eradicate human trafficking. #EndHumanTrafficking
View this post on Instagram
FROM July 29th, 2022
We can’t wait to act on viral hepatitis, this #FrontlineFriday we must commit to bringing hepatitis care closer to primary health facilities and communities. My Wellbeing Foundation Africa and I are echoing the World Health Organization roadmap towards eliminating all types of hepatitis by #2030 and calling to end mother-to-child transmission of #HBV, which requires immediate action, investment, and the end of stigmatisation and discrimination. Nigeria has the highest prevalence of #hepatitis in Sub-Saharan Africa and is third globally, with over 20 million Nigerians infected, including an estimated 15% of pregnant women. A silent killer, often going undetected, means there are upwards of millions of more Nigerians who are unaware. WBFA through its flagship Mamacare360 programme aims to progress the prevention of mother-to-child transmission #PMTCT of hepatitis B and address the systemic barriers of access to essential, equitable, lifesaving care, by providing antenatal and postnatal care, sexual and reproductive health education, safe trusted spaces with our #midwife guidance to tackle topics such as screening, antiviral prophylaxis, infant vaccination, and aim to scale them up for the prevention of perinatal transmission of HBV infection in Nigeria. Diligently providing this integrated grassroots healthcare on the #frontlines ensures we empower and support mothers and communities to be primary partners in their wellbeing and in the elimination of #hepatitisB. With a person dying every 30 seconds from a hepatitis-related illness, we must act now to accelerate the fight and advocate for the importance of testing, treating and vaccinating. Immunisation and access to drugs are crucial; we must work together strategically and cooperatively from epidemiological considerations, availability of resources and political prioritisation to support the infrastructure for administration. Expectant mothers can’t wait for hepatitis screening and treatment, and newborn babies can’t wait for birth dose vaccination. #WorldHepatitisDay
View this post on Instagram
FROM July 27th, 2022
Systematically equitable and sustainable access to water and sanitation is an essential human right recognised by the United Nations, and ensures communities can be peaceful and resilient in the face of health and wellbeing risks and climate changes. My advocacy is committed to improving access to #WASH for the nearly one-third of Nigerian children who do not have enough water to meet their daily needs, with over 60 million people in Nigeria lacking access to a basic clean water supply. The most marginalised, women and girls, suffer disproportionately from inadequate water resources and WASH services, increasing the likelihood of #GBV and decreasing economic freedoms. My Wellbeing Foundation Africa is dedicated to Nigeria achieving the Sustainable Development Goals, and strategically integrates #SDG 6: availability and sustainable management of water and sanitation for all, through a results-oriented advocacy action plan that builds on our nation's situation analysis and context-specific indicators, with the progressive reduction and elimination of inequalities between communities at the forefront. We must make certain that water supply and infrastructure are clean, safe, affordable and socio-economically beneficial to all; this demands critical collaboration and co-investment at all levels of government, water providers, the private sector, and community-based organisations. By working together, we can guarantee a future where everyone can be water-rich.
View this post on Instagram
FROM July 20th, 2022
I was pleased to join H.E. First Lady of Lagos State, Dr Mrs Ibijoke Sanwoolu MBBS, PGDHM, MPH, MBA, and HRM Oba Kabiru Sotobi, The Ayangburen of Ikorodu, alongside the Honorable Commissioner For Health represented by Permanent Secretary Dr Olusegun Ogboye, Mrs Kemi Ogunyemi HSC Commissioner IV, and Lagos State Health Service Commission Nurses led by Director of Nursing Services, Mrs Adebukola Cole, as Special Guests of Honour at the 13th Annual Nurses Scientific Conference of Lagos, to advocate for the gaps found in the nursing profession in Nigeria while developing a road map toward further investment and secure global health. Nurses and midwives constitute the majority of the global health workforce and the largest health care expenditure. Efficient production, successful deployment, and ongoing retention based on carefully constructed policies regarding the career opportunities of nurses, midwives, and other providers in health care systems are key to ensuring universal health coverage, as the World Health Organization estimates that an additional 9 million nurses and midwives are needed if the world is to achieve UHC by 2030. Yet, daily, nurses are constrained by practice regulations, workplaces, and career ladder barriers solely from contributing to primary health care delivery, and improving the lives of others. That is why together with our global partners and donors, during our implementation of our various programs such as Mamacare360 Community Midwifery Antenatal and Postnatal Education Program, EmONC upskilling for health workers, Medela Cares NICU Specific Lactation Support, Nutritional International LO-ORS Zinc to Combat Diarrheal Disease, we deliver a quadrupled dividend, to the health worker, health care facility, mother, and neonate, through improved health outcomes and empowerment while giving health care staff the opportunity to further their learning, training and education. Combating the challenge of ensuring that nurses are assured of decent work, decent remuneration and a safe and dignified workplace is essential to the implementation and development of our programming and mission. Saving lives does not mean a nurse should risk her own. We hear constantly of nurses facing extreme adversities and barriers on the ground, from not only the lack of basic infrastructure and professional support to deliver high-quality care but to the lack of access to clean water and working spaces. Health workers need clean water, adequate tools, equipment and medicine, to facilitate a safe and healthy delivery and support families’ health and hygiene needs across their lives. From health workers pulling buckets of water up from wells themselves, purchasing their own examination gloves, and digging makeshift pits themselves to dispose of medical waste, without access to WASH, and supplies and commodities needed to provide timely, high-quality care, our system will collapse. Effective supply chain management and procurement are needed so nurses can easily access life-saving medicines. Positive and safe work environments are also a must, as the most trusted and engaged members of health care, and oftentimes sole point of access in rural communities, nurses must feel supported. At the workplace, there should be zero tolerance for sexual harassment and gender discrimination. Vertical segregation, where female health workers do not advance to higher leadership and remuneration as their male counterparts, needs to be addressed as it remains a challenge within primary health care and health systems. To combat these hurdles, I believe there is a strong role for innovative multi-sector partnerships to play in helping accelerate progress towards security and investment in the health workforce and global health. The private and public sectors must collaborate with the local community and civil society, to improve the implementation and impact of the health workforce. The private sector plays an important role in most of the world’s health systems, from a mix of goods and services including direct provision of health services, medicines and medical products, and financial products, to training for the health workforce, information technology, and infrastructure and support services. Investment into primary healthcare spaces, and in nursing-driven social care, is key to humanity's survival in the current century. By investing in healthcare and the health workforce, we are solidifying solutions for local communities. We must work towards a comprehensive community health paradigm that will decrease delays in healthcare, bridge gaps in service delivery, ensure the highest quality of care, and create an integrated facility that can provide dynamic and comprehensive medical interventions and education. Private sector investment can also tackle the issues of the retainment of young professionals and women. Women comprise roughly 70% of the global health workforce and perform the majority of the sector’s most challenging, dangerous, and labour-intensive jobs. Yet they hold only 25% of the health sector’s senior roles and are rarely represented adequately. Instead, they are often expected to remain passive actors, quietly finding ways to do their jobs in difficult – even impossible – circumstances. Nurses are leaders, advocates and innovators. They are the largest, most trusted cadre of health workers and yet they have been largely overlooked and excluded from health policy discussions and investment decisions. As key players in health promotion and the backbone of healthcare systems worldwide, nurses work on the front lines as often the unsung heroes in health care facilities and emergency response. Rebuilding and reinforcing every element of health care begins with investing in nurses for a secure global health future and is essential for resilient community health and wellbeing. We must urgently invest in nursing education and leadership training to improve recruitment, retention and respect within the nursing workforce. Based on the report by the World Health Organization (WHO) in partnership with the International Council of Nurses (ICN) and Nursing Now, I call on facilities and partners to increase funding to education and employ more nurses, strengthen the capacity to collect, analyse and act on data about the health workforce, monitor nurse mobility and migration and manage it responsibly and ethically educate and train nurses in the scientific, technological and sociological skills they need to drive progress in primary health care. Despite the critical role they play in health care, there is a shortage of their voices at the table which must be addressed and strengthened on a Nation level. Therefore I am also calling for the establishment of leadership positions in government and development, we must ensure that nurses are allowed to fulfil their full potential, by improving working conditions through safe staffing levels, fair salaries, and respecting rights to occupational health and safety, implementing gender-sensitive nursing workforce policies, modernising professional nursing regulation by harmonising education and practice standards and using systems that can recognize and process nurses’ credentials globally. In my remarks, I deeply appreciated the Award Of Honour bestowed upon me in recognition of the WBFA's longstanding frontline programs at health facilities across Lagos State. I also took the opportunity to commend the Lagos State Health Commission's declared investments into primary healthcare spaces, and nursing-driven social care, to achieving #UHC, 2030 #SDGs, and solidify solutions for local communities. I pay tribute to nurses’ incredible work, professionalism, selflessness, courage, strength, and perseverance and express gratitude for their tireless efforts. Even in the face of exhaustion, stress, and physical and emotional trauma, nurses have inspired confidence and hope for the future. We must respect nurses’ rights and well-being to secure global health, and to do so we need massive investment in the acceleration of nursing education, creation of nursing jobs, and leadership. It is a fact that without nurses, midwives, and other health workers, countries cannot win the battle against outbreaks, or achieve universal health coverage and the Sustainable Development Goals.
View this post on Instagram
FROM July 14th, 2022
This Thrive Thursday, I reflect on the importance of Maternal, Infant and Young Child Feeding Nutrition to promote new norms around feeding practices among mothers and families, cultivate greater understanding around good nutrition-related behaviour and improve nutrition outcomes for children in the first 1000 days. Early and exclusive breastfeeding for the first six months of life is the single most important nutritional determinant for child survival. Yet, in Nigeria, where over 850,000 children under the age of five die each year, a majority of new mothers do not engage in optimal breastfeeding practices or provide a minimum acceptable diet and dietary diversity need. The loss of life, productivity, human capital, future economic benefits, and increased cost to heath systems at country, regional and global levels, call for immediate scaling up of financing and implementation of policies, programs and interventions to meet the WHO World Health Assembly’s Global Nutrition Target of ‘increasing the rate of exclusive breastfeeding in the first six months up to at least 50%’ by 2025, en route to the 2030 UN Sustainable Development Goals. Nutrition is one of the most vital components of primary health care, and through an evidence-based framework and collaborative strategic approach my Wellbeing Foundation Africa partnership with Alive and Thrive, with the support of McCann Global Health, FHI360, the Bill & Melinda Gates Foundation, emphasised optimal breastfeeding and complementary feeding practices for infants and children, from birth to two years of age, and adequate nourishment and care for pregnant women. During the multi-year programme (2018-2020) our aim was to build momentum, break down barriers, support a better future for women and children, which was replicable and scalable across the nation, to save lives, prevent illness, and ensure healthy growth and development through optimal maternal nutrition, breastfeeding, and complementary feeding practices, changing Infant and Young Child Feeding behaviours. Our outreach and cross-fertilization of the WBFA Alive and Thrive Infant and Young Child Feeding programme successfully reached over 200,000 antenatal care attendees, 120,000 mothers of children less than 2 years and 15,000 family members with an increased counselling content of facility healthcare workers in IYCF. To date, our Mamacare360 programme continues to work actively and consistently with all our partners to promote early initiation and exclusive breastfeeding, providing the lactation support required for mothers across Nigeria to sustainably continue as advised on the most recent American Academy of Paediatrics’ New Breastfeeding Recommendations for 2 years or beyond, with appropriate complementary foods introduced at about 6 months. To further upskill our midwives, healthworkers, and inter-personal community interlocutors, ensuring they are empowered and engendered to build on the program’s success, independently and continuously, my Wellbeing Foundation Africa with the support of Laerdal Medical, donated state-of-the-art breastfeeding simulators to aid education and improve knowledge on the physical anatomy and physiology of lactation and breastfeeding so that our breastfeeding guardians may accelerate nutrition results for better health outcomes for women and their families in Nigeria. The breast is the shortest, most sustainable supply chain, and the smartest investment a country can make to build its future of prosperity.
View this post on Instagram
FROM July 6th, 2022
I was delighted recently, to present the success stories of the Wellbeing Foundation Africa - Nutrition International 2021-2022 Intervention Partnership in Sokoto State to H.E. Governor Aminu Waziri Tambuwal. Zinc and low-osmolarity oral rehydration salts prevent child deaths due to diarrhoeal disease making the goal to end the loss of millions of young lives within our grasp. That is why my Wellbeing Foundation Africa is proud to be partnered with Nutrition International in Scaling up Zinc and LO-ORS to Improve Childhood Diarrhoea treatment in Northern Nigeria, specifically in Kano State and Sokoto State. The project, funded by the Government of Canada, and in partnership with the Ministries of Health, seeks to increase timely care-seeking and treatment of diarrhoea with zinc and low-osmolarity oral rehydration salts. Diarrhoea is a leading cause of malnutrition and death in children under the age of five, with the prevalence of childhood diarrhoea in Nigeria at 18.8%, accounting for an estimated 151,700 preventable deaths per year. Currently in Nigeria, only 26% of childhood diarrhoea cases are treated with oral rehydration salts solution, due to a lack of accessibility, availability and trust. Through WBFA and Nutrition International increasing and sustaining availability and access to zinc and LO- ORS commodities by strengthening their Drug Revolving Fund #DRF schemes with strong governance, financial and supply chain management, and in united action with health systems strengthening, deploying dedicated midwifery and nursing workforce to reach community health care facilities and households, we are creating statewide behavioural change which deliver measurable improvements to the most vulnerable. Our targeting of caregivers, with messages and visits from our community healthcare workers, promoting prompt care-seeking for children with diarrhoea, adherence to treatment with zinc and LO-ORS, and improvement in #sanitation and #hygiene has led the charge to curb the menace of diarrhoea. In Sokoto, our successfully implemented first phase has increased the development and health and wellbeing across 8 Local Government Areas of the State. One of our success stories was with a year old baby girl who our Wellbeing Foundation Africa Sokoto State Project Implementation Team met at the Kofar Kade Primary Healthcare Centre as she had been stooling up to 4 times a day. Working with the in-facility staff to provide expert care, the WBFA-NI Team advised the caregiver to immediately discontinue the use of Flagyl and utilise Zinc/LO-ORS for the treatment. The WBFA-NI Team Midwife then educated the caregiver on the preparation of the Oral Rehydration Solution (ORS) and Salt Sugar Solution (SSS), advised her on adherence to the stipulated duration, and stressed the need for the environment where the family resides to always be kept clean in line with #WASH. A follow-up visit by the Project Implementation Team was made to the house of the caregiver. During this visit, the team observed that the baby’s health condition had improved significantly. However, the team concluded that poor hygiene and sanitation within the household was the cause of the recurring case of diarrhoea within the family. Our midwife went on to further advise the best environment and personal hygiene practices. Through a cohesive approach which combines the critical services and interventions needed to create healthy environments, promotes practices known to protect children from diarrhoea and ensures that every child has access to proven and appropriate preventive and treatment measures, we can facilitate Nigeria embracing and reaching the #SDG Target 3.2, Newborn and Child mortality: end preventable deaths of newborns and children under 5 years of age by 2030, and the World Health Organization informed mission to achieve universal access to clean water and basic sanitation, which are the primary preventive measures in reducing the burden of diarrhoea. Safe drinking water, sanitation and hygiene are essential for stopping preventable deaths across Nigeria, as good health and wellbeing are simply not possible without #WASH. With an integrated approach, using a combination of the cost-effective zinc and LO-ORS co-packs, safe drinking water, basic sanitation, exclusive breastfeeding, and improved nutrition, we can dramatically reduce diarrhoea in Nigeria. My Wellbeing Foundation Africa looks forward to continuing the lifesaving and life-enhancing programming with Nutritional International for those who need it the most.
FROM June 24th, 2022
As the Kigali Summit took place yesterday to urgently increase investments and commitments critical to ending malaria and neglected tropical diseases, I am calling on all world leaders to unlock the potential of smart partnerships to conquer malaria, reduce the burden of NTD's and build a healthier better world for us all. Incredible progress over the last two decades proves that ending malaria and NTDs is an achievable goal. Investment in the fight through the Global Fund has led to 10.6 million lives saved and prevented 1.7 billion malaria cases. To date, 46 countries have eliminated at least one NTD and 600 million people no longer require treatment for NTDs. Yet, we still need renewed investments made by Presidents, Prime Ministers, CEOs, philanthropists, scientific experts, global influencers and community champions to save more lives, drive economic growth and support health systems to detect and respond to emerging diseases in a timely manner. We are currently at a crucial time in the fight against malaria. I acknowledge the African Leaders Malaria Alliance (ALMA), a groundbreaking coalition of African Union Heads of State and Government, working towards eliminating malaria by 2030 with various partners in their advocacy for data-driven decision-making, transparency, accountability and action on malaria, child and maternal health, NTDs and nutrition. Countries around the world must pledge financial support for the Global Fund to Fight AIDS, Tuberculosis and Malaria to help ensure that the world stays on track to end all three epidemics within a generation, to build strong national health systems to better respond to emerging pandemics. My Wellbeing Foundation Africa has witnessed time and time again, how malaria and NTDs continue to multiply in areas of poverty, afflicting the lives and livelihoods of billions of people. We cannot allow half the world to continue to suffer from preventable and treatable diseases. I am thrilled to echo Dr Tedros’ announcement regarding the launch of my dear sister and former mentors namesake Dr Mwele Malecela Mentorship Programme to develop women leaders to beat NTDs. Dr Malecela was the Director of the WHO Department of Control of Neglected Tropical Diseases, and an inspirational figure to all in global health. I recall her mentorship alongside Global Water in 2020, which aided WBFA in our uptake of WASH. I continue on in her memory, through my advocacy with the The End Fund, while re-affirming my commitment to sustainable, inclusive and collaborative action. The Kigali Summit is a historic opportunity to End Malaria and Beat NTDs. Let us make history and be a part of the generation that ends malaria for good. My Wellbeing Foundation Africa and I endorse the Kigali Declaration and will continue to advocate for mobilising a fully resourced Global Fund Replenishment to End Malaria. We must take action now - zero malaria starts with us all!
View this post on Instagram
FROM June 7th, 2022
Food safety is everyone's business, let's create lasting change! On World Food Safety Day, I am proud to join SDG 2030 to discuss how safer food, leads to better health and how we can collectively achieve the UN Sustainable Development Goals. Amplifying and mobilising action to prevent, detect and manage foodborne risks and improve human health is essential to public health. Food safety and security are two complementing elements of our sustainable future, and necessary for an equitable world. As we become increasingly interconnected, glocal citizens need to choose safe foods and #foodsafety for our one people and our only one planet. Women and girls are vulnerable at all levels of food safety, from availability, access, utilisation and stability. They suffer the most from macro- and micronutrient deficiencies, especially during the reproductive years. Through my Wellbeing Foundation Africa Mamacare360 program and Adolescents PSHE WASH program, we provide the knowledge mothers, adolescents, children and families need to alter food consumption for improved nutrition, as we are what we eat. From engaging with families and involving children in food safety activities to promote safe food handling and WASH, following the World Health Organization Five Keys to Safer Food Advocating, to advocating for low-carbon and resource-efficient sustainable food and farming systems to nurture the health of our people and our planet, food safety is everyone's business, at home, in workplaces, at schools, markets, and for food vendors. Thank you, SDG 2030, for having me today. WBFA and I continue to actively work toward achieving the SDG 2030 goals, at home in Nigeria, and through advocacy across the globe, as we must preserve people's opportunities to live in dignity and prosperity across generations.
View this post on Instagram
FROM June 3rd, 2022
On United Nations Global Day of Parents, I am celebrating and appreciating all the parents throughout the world, and emphasising the importance of healthy families to achieve the Sustainable Development Goals by 2030. Parents play the most critical role in the rearing of a child, from nurture to protection. A lifelong role as anchors of the family, and the foundation of communities and social progress, health and wellbeing practices often stem from parents and the environment they construct. My Wellbeing Foundation Africa aims to implement, support and motivate the sustained changes needed to improve family health in Nigeria. Our WBFA midwives, through our Mamacare360 program, better position our mothers to promote quality safe parenting for the full and harmonious development of their child. Our Sanitation Angels are on a mission to minimise any preventable negative health consequences, by being the community leaders of sanitation and hygiene, advocating for the right to WASH as a family habit and activity. Through our grassroots collective action, we are providing the tools parents need to catalyse and address their health and wellbeing needs, empowering them to be the primary model, educator, and influencer of family health outcomes, benefiting future generations to come. It is necessary we enhance awareness amongst decision-makers and the public of the effective ways of meeting family needs to further invest in one nation, one health.
FROM May 31st, 2022
Unfortunately for global health outcomes, tobacco product use begins and is primarily established during adolescent years. Today, on World No Tobacco Day, I invite you to join me in amplifying the World Health Organization commitment to raise awareness on the harmful and deadly effects of tobacco use in all forms, second-hand smoke exposure, alongside this years 2022 global campaign ‘Tobacco: Threat to our environment’. Tobacco has major implications for the health and wellbeing of smokers, non-smokers, and our environment. The industry’s effort to youthfully modernise tobacco use, to the greenwash marketing of its reputation by falsely advertising as environmentally friendly, is detrimental to our rising generation. Infants exposed in-utero to tobacco smoke toxins, through maternal smoking or maternal exposure to second-hand smoke, frequently experience reduced lung growth and function - with an estimated 60,000 children dying before the age of 5. Teenagers exposed to second-hand smoke are at risk of the onset and exacerbation of asthma, pneumonia and bronchitis, and frequent lower respiratory infections. Those who live on into adulthood continue to suffer the health consequences of exposure. At my Wellbeing Foundation Africa, we prioritise facilitating ‘taboo’ conversations between our frontline staff, midwives and adolescents early on during our Adolescent PSHE WASH program, creating inclusive safe spaces where they are empowered to build their autonomy to address topics like tobacco and substance abuse with their peers, families and communities - extending the effects and learnings beyond the program. WBFA responds to the tobacco epidemic through not only education and advocacy, but by the full organisational implementation of the WHO Framework Convention on Tobacco Control (WHO FCTC) and by adopting the MPOWER measures in our own policy development. Lung and environmental health is essential to achieving overall health and wellbeing. In order to achieve the SDG targets of a one-third reduction in NCD premature mortality, and to protect the planet from degradation by 2030, tobacco control and elimination must be prioritised by all.
FROM May 27th, 2022
Today on Children’s Day 2022 I reimagine a better future for every child, because from birth to adulthood, #everychildcounts. No child should ever be left behind. For 15 years, the Millennium Development Goals (2000-2015) were a guiding force on many issues affecting the lives of children, young people and their families. During this time, I established Alaafia in 2004, a Wellbeing Foundation Africa initiative which promoted and positively impacted the health and wellbeing of women and children, families and communities in Kwara State. Guided to engender and empower key strategies and solutions towards achieving progress in the key measurable indices set out by the 2015 Millennium Development Goals, we made tremendous progress in reducing preventable child deaths, getting more children into schools, creating accessible spaces for children's growth and enjoyment such as the Kwara children’s playground and childhood disability donations, while ensuring more families had access to safe water and nutrition education, earning the Unicef accolade of a state #FitForAChild in 2010. Today, the WBFA's nationwide program interventions and initiatives continue to be guided by the targets of the 2030 Sustainable Development Goals. Working with our partner, Nutrition International in Sokoto and Kano States, we are currently in the second phase of implementing the Scaling Up Zinc and LO-ORS to Improve Childhood Diarrhoea Treatment in Northern Nigeria which seeks to reduce the number of deaths due to diarrhoea among children under 5 years. Through our homegrown Primary & Adolescents #PSHE #WASH In Schools programme, we equip children with the skills and knowledge to make informed decisions for their own health and wellbeing, enabling them to be agents of change and positively impact their surroundings in the future. Myself and my foundation are committed to breaking intergenerational cycles of disadvantage and inequality in health and wellbeing that undermine the stability of societies and even the security of our nation. Through a pragmatic and strategic approach, we place children's rights and wellbeing at the centre to catalyse sustainable development by breaking down the transfer of poverty and exclusion from one generation to the next. A child rights-based approach multiplies future development gains. Children's Day offers each of us an inspirational entry-point to advocate, promote and celebrate children's rights, translating into dialogues and actions that will build a better Nigeria for our children. Our children are the leaders of today, we must do everything in our power to create an environment in which they can thrive and succeed, from health, the economy to climate change and beyond.
View this post on Instagram
FROM May 27th, 2022
Day 4 at the Seventy-Fifth World Health Assembly was an excellent opportunity to reflect on the impact of longstanding allies and advocates - as my Wellbeing Foundation Africa Global Delegation attend ongoing in-person Plenary Committee meetings in the Palais des Nations and various interdisciplinary sessions. As I joined them for the exclusive one-day, hybrid DEVEX@WHA75: Reimagining Global Health Security event, I was delighted to engage with expert analysis and insider coverage of this week’s most important conversations and commitments. The past two years have proven that the world needs to be more prepared for the next pandemic, with a major theme of this year's Assembly focusing on health emergency preparedness and response. Even as COVID-19 bolstered the birth of new initiatives, interest in the creation of new institutions, and debate on how to change what has long been the status quo - the matter of ending the current pandemic remains high on the agenda. Connecting with other leaders in global health from around the globe, it was wonderful to listen to and see my good friend, and longtime advocacy companion, Dr. Githinji Gitahi, Group CEO, Amref Health Africa, discuss achieving vaccine equity, as another ally Loyce Pace, Assistant Secretary for Global Affairs, U.S. Department of Health and Human Services, discussed preparing for the next pandemic and the new preparedness instruments that would be needed, hear from Medtronic LABS, with a spotlight on better health for all through digital solutions, and see Nina Schwalbe, Adjunct Assistant Professor, Columbia University Mailman School of Public Health, Dr. Petra Khoury, Director for Health and Care Department, IFRC. With the World Economic Forum, taking place in Davos, ending today, this week in Switzerland has been compelling and poignant. Embodying both the World Economic Forum and the World Health Assembly, I truly believe a philosophy of collaborative, multistakeholder impact, in a uniquely accessible environment, was needed to reconnect, share insights, gain fresh perspectives, and build problem-solving communities and initiatives. As the global fractures and broken systems in health, politics and economics are highlighted, the convenings this week shed light on refreshed rooted trust, a starting point for a new era of global responsibility and cooperation.
FROM May 25th, 2022
“I am not African because I was born in Africa but because Africa was born in me”. ~ Kwame Nkrumah Happy Africa Day! Let us celebrate our continent’s unity, achievements, cultures and traditions. On this day, in 1963, the Organisation of African Unity – now known as the African Union – was established. As we commemorate this momentous day, with the African Union celebrating their 20th anniversary, I am proud to reflect on the accomplishments of our people across the continent. Yesterday, at #WHA75 my brother, Dr Tedros, was elected to serve a second five-year term as Director-General of the world's leading public health agency - The World Health Organization. The first African leader of the United Nations health agency, Dr Tedros’ tireless commitment to global health, care for humanity and humility is an inspiration for us all. His values embody the progress of our continent, and we are fortunate to have direct representation and a primary voice as our advocate. This year's Africa Day celebration is centred on nutrition, with the African Union Theme for the year 2022 “Strengthening Resilience in Nutrition and Food Security on the African Continent”. Myself and my Wellbeing Foundation Africa would like to emphasise the focused importance of addressing malnutrition and food insecurity, particularly in children. According to the findings of the Cost of Hunger in Africa Study, it is estimated that African countries are losing the equivalent of between 1.9 and 16.5% of their Gross Domestic Product (GDP) due to child under-nutrition. It is also estimated that malnourished children are at risk of losing more than 10% of their lifetime earning potential. That is why my WBFA addresses nutrition through our Adolescent Skills and Drills, Personal Social And Health Education programming, and Mamacare360 programme, to particularly empower the girl child and mothers, who often lacks iron and folic acid, as Africa's potential and bright future is centred around African women and youth. They are integral to the solution, especially in driving sustainable development, innovation and achieving the African Union’s vision of Agenda 2063. It is vital that we are supported by increased and well-targeted official development assistance, but above all by an increase in allocations of national resources, focused on the nutritional well-being of populations, including the most vulnerable ones. I trust that Dr Tedros, the WHO and WHOF, will continue to focus on the existing malnutrition challenges which have greatly exposed the economic vulnerability of African countries and the weaknesses of our health and food systems. Working together with all stakeholders, and with effective partnerships with UN Agencies, we can allow Africa the opportunity to thrive as the powerhouse it is, and contribute to achieving all the Sustainable Development Goals. As reinforced and combined action to strengthen resilience in nutrition and food security will lay a strong foundation to empower our continent. “God bless Africa, Guard her people, Guide her leaders, And give her peace.” ~ Trevor Huddleston
FROM May 24th, 2022
As the Seventy-Fifth World Health Assembly begins - the first in-person Health Assembly since the start of the COVID-19 pandemic - I am thrilled to join the World Health Organization in celebrating and amplifying the importance of health and wellbeing. Dedicated to the well-being of all people and guided by science, the WHO is committed to continuing to lead and champion global efforts to give everyone, everywhere an equal chance at a safe and healthy life. The World Health Assembly convenes each year, as it is the main decision-making body of WHO and comprises 194 Member States. Delegates from all Member States have come together to agree on the Organization’s priorities and policies with country delegates making decisions on health goals and strategies that will guide their own public health work. The theme of this year’s Health Assembly is health for peace and peace for health. The COVID-19 pandemic and other health emergencies with international reach have highlighted the leadership and coordinating role of WHO in responding to such events - necessitating a heightened focus on strengthening preparedness for and response to health emergencies. As the Inaugural Global Health Ambassador for the World Health Organization Foundation, myself and my Wellbeing Foundation Africa are actively working, through advocacy and programming, to achieve the WHO's “triple billion targets”. The targets are that, by 2025 (from a starting point of 2019), one billion more people will be benefiting from universal health coverage, one billion more people will be better protected from health emergencies, and one billion more people will be enjoying better health and well-being. This #WHA75, with pressing matters of civic importance at home in Nigeria, I am ably represented at the in-person strategic roundtable and normative sessions in Geneva by the WBFA Global Delegation, which looks forward to celebrating partnerships in Strengthening Africa's Architecture for Health Emergency Preparedness, Response and Resilience, this evening, with special gratitude to the Bill and Melinda Gates Foundation, in the presence of Africa CDC, the WHO AFRO and EMRO, and partners in global health emergencies. As the WBFA Global Delegation to WHA75 commences their engagements - I am confident that people-centred frontline impact will shape global policy deliberations and the important gender data around our core focus of RMNCAH, EMONC, Nutrition, One Health and WASH. I look forward to their reports on the implementation of the areas of work set, in order to determine what has been achieved and decide on strategies for addressing the gaps.
FROM May 18th, 2022
I was honoured today to join Pathfinder International and She Forum Africa as a panellist for their high-level convening to deepen awareness and build momentum for gender equality in Nigeria through “Partnerships for Goals: Advancing the Gender Agenda for Sustainable Development.” Coming together on International Day of Living Together in Peace, I reflected on the importance of accepting differences and having the ability to listen to, recognise, respect and appreciate others while encouraging our Nation to unite in differences and diversity, particularly when it comes to Gender Equality, allowing us to further contribute to the United Nations Sustainable Development Goals. Nigeria is a beautiful and unique example of cultural heterogeneity, with over 250 ethnic groups, 500 languages, and many religions. Amplifying the diversity in our national identity is essential to achieve reconciliation and promote harmony. I hold these beliefs and values dearly, as exemplified daily in my life and work with my Wellbeing Foundation Africa, as our efforts towards community behaviour change, and driving a community forward, can only prevail where peace exists. Currently, according to United Nations Children Fund (UNICEF), in 2022 Nigeria has 18.5 million out-of-school children, an increase from the 10.6 million in 2015, with over 60% being female, meaning around 10 million girls are out of school today. This heightening of gender inequity in the Nigerian society is the reason why only one in four girls from poor, rural families complete junior secondary school, and why one in every four children out-of-school in the world is from Nigeria. We have a national crisis on our hands due to the terrorist attacks on schools and education centres, gender inequality, and lack of adequate resources, negatively affecting access to education for children across the nation. Addressing the barriers that hinder the girl child's education is extremely important, and exactly why it is essential to have conversations surrounding the topics of ‘Partnerships for Goals: Advancing the Gender Agenda for Sustainable Development’ and ‘International Day of Living Together in Peace'. Our discussions, with representatives from the Government, CSOs, development partners, members of the diplomatic community, youth and disability organisations and various EVAWG stakeholders, including the private sector, focused on commitment to supporting, promoting, strengthening and intensifying solution-oriented advocacy around women and girls agency from a rights perspective through unity and collaboration. By sharing the work of my foundation, and how we analyse gender policies and bills, advocate at all levels to transform the system to further promote the agency and rights of women, girls, and marginalised groups, and identify opportunities to increase the participation of women and girls in SRHR decision-making, I hope to amplify how to regularly mobilise the efforts needed from the national and international community to tolerance, inclusion, understanding and solidarity. WBFA is wholly committed to helping Nigeria achieve the Sustainable Development Goals by 2030 with a particular emphasis on SDG 5, to achieve gender equality and empower all women and girls. While progress has been made, no country in the world has achieved gender equality or complete harmony. Our nation must continue on the path to uphold the desire to live and build together towards sustainable solidarity, foster compassion and understand one another. Our differences make us stronger and more dynamic; our diversity enhances our innovation, creativity and potential; our inclusivity encourages various perspectives and growth; our unity makes us Nigeria. Let us mobilise our efforts from corner to corner, I look forward to continuing this discussion with key stakeholders across all sectors, including working with communities, faith leaders and other relevant actors, to leverage and promote the rallying role of the UN Sustainable Development Goals while supporting and educating communities on gender equality and harmony. We need to equalise the equity of opportunity from birth to age - to achieve gender parity.
View this post on Instagram
FROM May 5th, 2022
To celebrate International Day of the Midwife #IDM2022 and the International Confederation of Midwives centennials anniversary #ICM100, I am thrilled to launch my book in the honour of midwives, maternity support workers and student midwives around the world. ‘Midwives at the ‘Front’ of Frontline Action’ is an anthology of my advocacy and action, with the aim of amplifying resources, respect and recognition for the midwifery profession globally. Featuring recommendations and letters of support from, but not limited to, Dr. Tedros Adhanom Ghebreyesus - Director General of the World Health Organization (WHO), Francis-Day Stirk - Former President of the International Confederation of Midwives (ICM), Jacqueline Dunkley-Bent - First Chief Midwifery Officer Of England And Professor Of Midwifery at King’s College London and London South Bank University, amongst many more. Over the many years of my advocacy, outreach and community programming journey, I have witnessed midwives meet extraordinary circumstances and risk their lives to provide excellent care to women and their families. As I commemorate their bravery and importance to healthcare, I also call on the international community of health to invest in midwives and maternity care. You can read my ‘Midwives at the ‘Front’ of Frontline Action’ by clicking here!
FROM May 5th, 2022
Today, I celebrate International Day of the Midwife and mark the International Confederation of Midwives centennial. I applaud our collective progress; acknowledge how far we have come in advocating for and delivering, investments in midwifery. Midwives support and protect women, newborns and families. They are crucial to reducing maternal and neonatal morbidity and mortality. Each day they stand up for the rights of women to receive respectful maternity care and fight on the frontlines. Midwifery spans an incredible breadth in healthcare, yet many midwives across the globe, who are predominantly women, face persistent struggles rooted in gender equality, a lack of investment in their profession, training and education, pay gaps and limited protection. Imagine a world where midwives have achieved the investments they deserve, from equitable compensation, fair working conditions and protections, standardised regulation frameworks, equal opportunities to local education, and policy which protects them from gender-based abuse and harassment; midwives would be well supported to avert roughly two-thirds of maternal, newborn deaths and stillbirths by 2035; 1.9 million stillbirths averted every year, 2 million neonatal deaths averted every year, 280K maternal deaths averted every year, saving 4.3 million lives per year. Midwives must be recognised for what they are: a pathway to achieving the #SDGs. Evidence demonstrates that in order to improve maternal and neonatal health, improve sexual and reproductive health and rights and meet the Sustainable Development Goals, midwife-led continuity of care is crucial. Policies which allow midwives to perform their full scope of practice, strengthen primary healthcare systems, and provide an innovative opening to achieving universal health coverage. The midwife, by virtue of her education, sphere, the scope of practice and unique relationship with women and their families, is in an ideal position to provide the information, services and support which women need in planning their families, as well as to influence the type of services based on the International Confederation of Midwives Global Standards for Midwifery Regulation. If midwives had equal access to education, they would have greater career satisfaction and longevity, and all families would have access to culturally relevant, professional sexual and reproductive healthcare, and maternal health. Women and other birthing people everywhere would benefit from life-enhancing, professional and respectful, care and the standards of midwifery practice all over the globe would be raised. The global evidence unequivocally indicates: that increased investments in midwives and midwifery have led to healthier, happier families and communities in every corner of the world. I see it daily with my Wellbeing Foundation Africa midwives, who conduct various programming from our flagship Mamacare360, which delivers care in line with the World Health Organization recommendations and bridges gaps by making the mother a premium partner in her outcome, through respectful maternity care, education and awareness, to our Sanitation Angel midwives, who deliver key WASH and SRHR knowledge and best practice to children and adolescents in schools, and health workers in public and private primary, secondary and tertiary health facilities across Nigeria. That is why I call on governments, policymakers, regulatory authorities, educational institutions and international and civil society organisations to turn their focus to paving the way for midwives, with universal access to sexual, reproductive, maternal, newborn and adolescent health services, addressing equity at all levels and leaving no one behind. It is simple: midwives equal sustainable healthcare. Today I thank the midwives who stand up for the rights of women to receive respectful maternity care. The midwives who offer contraception even though their societies refuse. The midwives who have supported pregnant women who are suffering from abuse and cannot return home. The midwives that say no to performing FGM. The midwives that have held perpetrators of rape and violence accountable, despite fear of the ramifications. The midwives that continue to hold the torch for gender equality and defend women and girls. Midwives need support at all levels of a nation to practise in a safe and enabling environment. Midwives should be free from harm going to work, at work and in their homes. Driven by one strong collective voice, we must continue advancing and mobilising the evidence to ensure the next 100 years are even more monumental for midwives, women, newborns and all people. I am in awe each day of midwives around the globe, and proud that each passing year feels more significant for midwives and midwifery than the one before it. We must continue to #PushForMidwives, around the globe.
View this post on Instagram
FROM April 1st, 2022
In holding true to ancient wisdom, we must continue to evolve and flow.
I was privileged yesterday to honour the invitation of His Imperial Majesty, Alaiyeluwa Arole Odua, Oba Enitan Ogunwusi Ojaja II, The Ooni of Ife, to Chair the Launch and Public Presentation of Unspoken: Oba Obinrin, a chronicle not of Queens, but of Female Kings of the ancient yoruba culture and tradition.
Celebrating historical female royal leadership, hitherto unspoken, and thus unknown and unlearnt by so many generations, was to me, a fitting path from a gender precipice to stronger engendered ground in our dear nation, on the last and final day of #WomensHistoryMonth around the world.
In my Chairman's address, I traced the journey and evolution of the role and status of women in Nigeria from precolonial times to the early 21st century - throughout which women have played a major role in social and economic activities, also highlighting also the strong recognition within our yoruba tradition of the philosophy and perception of Abiyamo: The Yoruba concept of Motherhood, as a unique matriarchal leadership model.
As a female leader, Pioneer Member and Steering Council Member of the UN Women’s African Women Leaders Network Initiative globally and in Nigeria respectively, a member of the ICPD25 International Steering Council and Founder and President of The Wellbeing Foundation Africa, an NGO which works to improve health and wellbeing outcomes for women, infants and children, advocacy for women and the girl child across Nigeria, I stand on the shoulders of the Yoruba heroines who have come before me. It is their strength, their sacrifice and their legacy that has allowed me to face all challenges with boldness and without fear.
As a member of His Imperial Majesty The Ooni of Ife’s Caucus of Eminent Yoruba Sons and Daughters, I am inspired by the works of Queen Moremi Ajasoro and the legendary Ooni Luwo Gbagada of the Ancient Ife, the trailblazing Pupupu of Ondo kingdom, Alaafin Orompotoniyun of Old Oyo kingdom and the memorable female Awujales of Ijebu-Ode.
Alaafia, my central motto promotes the attainment of a state of peace, wellbeing and harmony for our mothers, our Abiyamo, their newborns, their families and communities. My Wellbeing Foundation Africa frontline initiatives and my advocacy are based on the theme Alaafia, to establish, promote and positively impact the health and wellbeing of women and children, families and communities. Through the culture of promoting Alaafia throughout the 670 communities where we now work in Lagos, Cross River, Kaduna, Kwara, Osun, Sokoto, Kano States and the Federal Capital of Abuja, we are empowering and engendering the rise of our women and girls through effective frontline programmatic actions and strategic partnerships
Women in the Yoruba world view appear as 'water' the primordial element, thus there is a tendency to characterise women as an object that can flow across spaces and leave indelible marks in time. According to Yoruba beliefs, water is the essence of life. So is a woman who brings forth children. She ensures the continuity of the life of the lineage and of the community. Indeed, the ancient Yoruba declaratory prayer 'Oju-Oro ni ileke omi' implores those seeking success, strength and superiority to stay on top of water, and thus evolve and flow.
The Alaafia Agenda’s constant and consistent reinforcement, renewal and replenishment of sustainable development actions is in itself a validation of historical culture and tradition. It is only through our joint efforts as pathfinders that we can bring to current and contemporary life - the Yoruba tradition and culture and its pillars of female leadership enshrined in our history by Alaafin Omopoto the first woman to become "king" of the Oyo Empire and Ooni Lúwo Gbàgìdá the 21st Ooni of Ife in the 10th century. Our shared past has given us a special identity, Alaafia Abiyamo, and equally a shared future for our common and universal wellbeing as crowned, uncrowned and acknowledged Oba Obinrin.
We must and will rise to our obligation and the fulfilment that history has bestowed on us, as pathfinders, for our women, for our children, for our menfolk, our ecosystem of communities, and for our leaders of tomorrow.
FROM March 25th, 2022
I was pleased to join the Bricon Foundation, Co-founders Dr Niyi Adekeye and Mrs Abigail Simon-Hart, Trustee Mrs Sonja Ally and special guest Dr Adamu Umar, President of the Nigerian Cancer Society at the launch of The Bricon Foundation’s new fundraising campaign “ E Fit B u” to raise 50 Million Naira for cancer patient treatment on Sunday, March 20th, 2022. Cancer remains the leading cause of death worldwide, accounting for nearly one in six deaths, and with a new case of cancer being diagnosed every 2 seconds, changing lives completely. In 2018, I and my Wellbeing Foundation Africa commissioned the Report of the Rapid Assessment of Cancer Care in Nigeria by The Wellbeing Foundation Africa (WBFA) on behalf of Amref Health Africa. As the statistics prove, cancer is a personal story for all of us, with us all being affected. In February of this year, I lost a very close friend of mine, Dr Mwelecele Ntuli Malecela to cancer. She was a passionate advocate for eliminating neglected tropical diseases as Director of WHO’s Department of Control of NTDs. She was also a highly respected scientist, who specialised in lymphatic filariasis in Tanzania - a truly inspirational figure for young women in science, a dedicated leader and a committed listener. Unfortunately, cancer is a cruel and silent disease. It does not care about your age, gender, status, or personality to be diagnosed with it, but then to be treated for it, it does; the equity gap within cancer care is costing lives. People who seek cancer care hit barriers at every turn. Income, education, geographical location and discrimination based on ethnicity, race, gender, sexual orientation, age, disability and lifestyle, and the cancer care infrastructure and specialist nursing and midwifery workforce deficit are just a few of the factors that can negatively affect care. The most disadvantaged groups are also more likely to have increased exposure to a host of other risk factors, like tobacco, an unhealthy diet or environmental hazards. It is almost guaranteed that the cancer care gap affects you or people in your community. If we work collectively we can close the gap. The reality today is that who you are and where you live could mean the difference between life and death. It is not fair, but we can work to change this. We must bridge the gap and support organisations like Bricon in their admirable work to make the lives of people experiencing cancer and their families better and together, strive to make a difference in the Cancer Care landscape in Nigeria. Nigeria suffers from high morbidity and mortality of cancer, with a 60 percent death rate. This rate is disturbing and extremely high. By improving the gaps that exist throughout the cancer care supply chain; from policy to health system capacity, screening and early detection to financing treatments, and the available workforce in cancer care to cancer survivors and family support, we can support the 40% while raising the overall survival rate. According to the Wellbeing Foundation Africa and Amref Health Africa’s landmark 2018 Rapid Assessment of Cancer Care in Nigeria - which guided Nigeria’s policymakers in formulating National Cancer Strategy and Registries - the burden and trend of non-communicable diseases - including cancer - is on the increase in Nigeria - and it is instructive that the research was supported not by any domestic resource mobilisation, but by an international donor, Takeda. We found that most states had only one officer in their NCD unit who rarely comes to the workstation. Primary Health Cares have functional referral systems but most health workers in these facilities do not have the capacity to screen or make diagnoses at this level. The treatment in these facilities is not optimal because of inadequate financing, insufficient equipment and a low level of technical know-how in dealing with cancer. The supply chain of drugs and commodities are also very expensive, leading to the majority of the population experiencing a financial barrier to treatment. The report shows that at a stakeholders' level, the awareness of cancer is low, and according to the health workers, most of the patients present themselves to the health centres when cancer is at stage 3 or 4 when nothing much can be done beyond palliative care and counsel. The cancer care landscape in Nigeria is compounded with an acute shortage of health personnel, due to the ongoing brain drain of health personnel to high-income countries. For example, Clinical Nurse Specialists in Nigeria are long overdue for the development, recognition, and legal inclusion of the Midwifery and CNS roles and practices in the career structure of nurses at all levels of the health system and Midwifery Services Framework. In collaboration with national and international partners, my Wellbeing Foundation Africa’s Cancer Alliance is now committed to formulating a road map towards an important Push Policy that would: train, recognize and remunerate advanced degree nurses and Midwives in the clinical settings with appropriate salary scale; establish standards for CNS role and practice; and develop the CNS curriculum with master’s level courses that include opportunities for content-specific clinical experiences such as specialist training for cancer nursing. The Bricon Foundation recognises the lack of sufficient support structure (counselling and advice), equipment, financial assistance and trained medical personnel to cope with the ever-increasing numbers of cancer patients. Whilst screening and advocacy continue to bring cancer patients to the fore, the treatment and support structures cannot cope with these rising volumes. There is, therefore, a need to address the different areas of cancer care to ensure that patients who are found to have cancer, have choices of where to go to receive care, and more importantly can afford to have this care at all. We cannot overemphasise the importance of having the relevant medical infrastructure within the country, supported by well-trained motivated professionals and appropriate legislation. This can only be done if there is sufficient funding to the medical sector as a whole and if there are funding mechanisms to make more complex specialist care such as cancer treatment available to all citizens and not just the wealthy and informed. Helping raise awareness about cancer via education, advocacy and counselling, caring about the emotional well-being of those with cancer, and supporting fundraising for treatment, equipment and training are all necessary for the continued fight against cancer. In 2022, the Bricon Foundation remains committed to improving the quality of care available to cancer patients through support for the purchase of much-needed cancer drugs and medicaments, funding for treatment and diagnostic tests as well as much-needed emotional support to them and their families. They will also resume training programmes for healthcare workers in Breaking Bad News, end of life and Palliation. This battle requires a holistic approach, including increasing the awareness about the disease; educating on screening and early diagnosis; training and retraining of relevant health workers; and infrastructure upgrade in our facilities across the country. Let us all support Bricon in their commendable work to make sure cancer patients, survivors and their families are supported in all stages of this disease by contributing to the Bricon Foundation’s target of Raising 50 million Naira so that we can support the Foundation in this mission. Since I am committed to the cause of upskilling the nursing and midwifery profession to provide specialist care, I am working towards mobilising resources to create a dedicated grant to support the Bricon Foundation’s Macmillan based services. We may not cure cancer today, but we can contribute to the battle against it by doing what we can to support closing the care gap today!
FROM March 17th, 2022
We must create better opportunities for women and children with disabilities. When disparities due to gender, disability and age intersect, these driving factors widen inequities, intensifying exclusion. The time is now to turn the clock forward on women’s rights. March is an empowering and significant month for women and girls globally, with it being Women’s History Month, International Women’s Day (IWD), Women’s Week and the UN Commission on the Status of Women (CSW66). As we spend the month celebrating women and girls, their contributions to history, culture and society, and advocating for their further equity and opportunity, we must highlight women as active supporters and claimholders of development. No nation can advance progressively in any sector without the contributions of all women. Despite the enormous and undeniable contributions women and girls make to their communities, they continue to be marginalized and deprived due to gender inequality. “Gender equality today for a sustainable tomorrow” is this year’s IWD theme, and I had the pleasure to expand on this subject with Radio Nigeria on IWD - March 8th in association with Partnership for Maternal, Newborn and Child Health, in the lead up to the UN Commission on the Status of Women (14-25 March, 2022). I truly believe that achieving gender equality and the empowerment of all women and girls in the context of climate change, environmental and disaster risk reduction policies and programmes will require deliberate and intentional actions to integrate a #OneHealth approach. Disparities due to gender, along with factors such as disability and age, respectively, are driving factors for widening inequities. When the three intersect, the negative impact of exclusion is intensified. As a result, adolescent girls with disabilities are one of the population groups facing overwhelming barriers and are left furthest behind in all walks of life. I am humbled to, in association with my Wellbeing Foundation Africa, join PMNCH global alliance for women’s, children’s and adolescents’ health to highlight these persistent disparities and their consequences. Disability and poverty reinforce and perpetuate one another and as such, disability has a higher prevalence in lower-income countries. 80% of people with disabilities live in developing countries, facing more frequent socioeconomic inequities than their non-disabled peers, including a higher rate of poverty, lower education level and increased rate of unemployment. Girls with disabilities experience a range and variety of impairments, including physical, psychosocial, intellectual and sensory conditions, that may or may not come with functional limitations. Compared to men without disabilities, women with disabilities are three times more likely to have unmet needs for health care, three times more likely to be denied health care, four times more likely to be treated badly in the healthcare system and 50% more likely to suffer catastrophic health expenditure. While all people with disabilities face varying discrimination and are often invisible in policies, women and girls with disabilities are subjected to double discrimination: because of their gender as well as disability bias. Women and girls with disabilities are not a homogenous group: they include those with multiple and intersecting identities across all contexts, such as ethnic, religious, and racial backgrounds; their status as refugee, migrant, asylum-seeking, and internally displaced women; LGBTIQ+ identity; age; marital status; and living with or being affected by HIV. The disabilities being faced by women and girls are equally diverse, including physical, psychosocial, intellectual and sensory conditions, that may or may not come with functional limitations. The pre-existing inequities and discrimination that adolescent girls face on a daily basis have been further amplified during the COVID-19 pandemic. In places hit hard by COVID-19 and others with a much lower rate of infection—women and girls with disabilities are still being left behind. They are struggling to meet basic needs, to access needed health services including those specific to their gender and disability, and face disproportionate risks of violence. Systemic barriers coupled with the failure to prioritize the collection of data on the situation of women and girls with disabilities have perpetuated their ‘invisibility’ within societies, as multiple and intersecting forms of discrimination exclude them from various aspects of life. Girls with disabilities have lower school completion rates and lower literacy rates than all other children, for example, and girls and women with disability face particular barriers to sexual and reproductive health (SRH) services and information. Provision of accessible sexual and reproductive health and rights (SRHR) information and services for girls and young women with disabilities are largely non-existent, with service providers in health centres, schools, and institutions that house them ill-prepared to handle their specific needs. And when women and girls with disabilities try to access services, they can experience negative and hostile attitudes among service providers, lack of accessible buildings, equipment, and transportation, affordability of services, and isolation in institutions, camps, family homes, or group homes. Women and girls with disabilities also suffer up to three times greater risk of rape and are twice as likely to be survivors of domestic violence and other forms of gender-based violence (over a longer period and with more severe injuries) than women without disabilities. The absence of appropriate sanitation facilities for girls with disabilities in schools, including separate, accessible, and sheltered toilets, in addition to the lack of education, resources, and support for menstrual hygiene, compromise their ability to properly manage their hygiene and make them especially prone to diseases. This often leads to girls and young women with disabilities staying at home or being sent to special schools. It can also lead to grave violations of rights such as forced hysterectomies or forced use of contraception that can eliminate or reduce menstruation. Girls and young women with disabilities have the same sexual and reproductive health and rights as other girls and young women, as recognised in various internationally recognised conventions signed by many countries, for example, the Convention on the Rights of the Child (CRC), the Convention on the Elimination of all Forms of Discrimination Against Women (CEDAW), and the Convention on the Rights of Persons with Disabilities (CRPD), yet in practice, their needs are being overlooked or under-prioritised. This needs to change. The situation for girls and women with disabilities only worsens in humanitarian settings - conflict and displacement exacerbate and heighten the discrimination that they already face in times of peace and destroy their protection systems, making them more vulnerable to exploitation. In such vulnerable situations, for example, girls and women with disabilities face increased levels of sexual and gender-based violence (GBV) in and out of the home, especially those with intellectual and mental disabilities. Factors contributing to the lack of inclusion of women and girls with disabilities in humanitarian response include; gaps in policy development and implementation; negative attitudes of family members and communities; limited staff knowledge, attitudes, and practices; and lack of champions and local partners. My foundation - the Wellbeing Foundation Africa focuses on preventing birth injuries that may cause or lead to disabilities by improving maternal and child health from the very start. We emphasize and practice screening in order for preparedness, work with healthcare facilities to strengthen EmONC throughout Africa and the developing world and educate our mothers through the WBFA Mamacare360 flagship programme. We do this all while always practicing and preaching inclusion and accessibility of all. Universal access to EmONC is essential to reduce maternal mortality and requires that all pregnant women and newborns with complications have rapid access to well-functioning facilities that include a broad range of service delivery types and settings. We must ingrain this practice throughout Africa and rebuild the healthcare system. The 2030 Agenda for sustainable development is clear that disability cannot be a reason or criteria for lack of access to development programming and the realization of human rights. The SDGs include seven targets that explicitly refer to persons with disabilities. There is a need for an intersectional approach that empowers women and girls with disabilities and dedicates more resources and technical support, integrates innovative solutions, and develops guidance and practice which explicitly considers disability to create more enabling and accessible environments for persons with disabilities. Disability-related support services must also be classified as essential services. States must undertake long-term efforts to ensure the full respect, protection, and fulfillment of SRHR, the right to be free from violence, and related rights for women and girls with disabilities at all times. We need more data in this arena to support programme development. States need to prioritise the collection and dissemination of disability-related and disaggregated data and information to drive evidence-based programming and accountability. Adolescent girls with disabilities should be capacitated, empowered and meaningfully engaged in the development of all policies, programmes and legal processes that affect their health and well-being, which is one of the central tenets of PMNCH’s Adolescent Call to Action: https://www.adolescents2030.org/. We need to recognize that African culture hides disability, and therefore access to available basic needs becomes a problem. African Countries and policy makers must implement a One Health approach to tackle future pandemics and develop a system of support that provides a better platform for engagement with PWDs, to grant them more access to basic facilities in the country. One Health is gaining recognition as an effective way to fight health issues at the human-animal-environment interface, including zoonotic diseases, as the approach recognizes how intertwined the health of people is with the health of animals, plants, and our shared environment. This collaborative, multisectoral, and transdisciplinary approach when implemented at the local, regional, national, and global levels can achieve the goal of optimal health outcomes which recognise the intrinsic connection between all living matters. Successful public health interventions require the cooperation of human, animal, and environmental health partners. Professionals in human health (doctors, nurses, public health practitioners, epidemiologists), animal health (veterinarians, paraprofessionals, agricultural workers), environment (ecologists, wildlife experts), and other areas of expertise need to communicate, collaborate on, and coordinate activities. Even law enforcement, policymakers, agriculture, communities, and pet owners are relevant players in a One Health approach. No one person, organization, or sector can address issues at the animal-human-environment interface alone. To create a safer, more equitable future for our women and girls, we must advocate and put into action proactive and accessible policy which supports them from the get-go and not only when emergency situations arise. Through collective effort, we can create a sustainable tomorrow built upon and based on gender equality.
FROM March 2nd, 2022
Today I write in disappointment and dismay, but undaunted. I am filled with the determination that Nigeria’s women must succeed.
As I write this note, Nigeria’s lawmakers - elected and empowered primarily and federally to protect and uphold the rights and dignities of the Nigerian people - have once again cemented another painful setback for us, our women and girls.
On Tuesday the 1st of March, Members of the 9th Session of the National Assembly’s House of Representatives voted a loudly reverberating, and disregarding no to four gender-sensitive bills proffered within the review of 68 amendments to the 1999 Constitution:
A bill to provide 111 special seats for women in the National and State Houses of Assembly – Rejected
A bill to expand of the scope of citizenship by registration – Rejected
A bill for Affirmative Action for women in political party administration and leadership – Rejected.
A bill to reserve a quota for women (on political appointments) – Rejected.
The denial of passage of these bills illustrate the palpable opposition to opening the space for women’s participation in everyday politics, governance and in the exercise of our rights and power. We are furious.
Women are locked in a cage of underrepresentation in Nigeria. As of February 2021, only 3.6% of seats in parliament were held by women in a country where 49% of the population is female. Currently, only seven out of 109 senators and 22 of the 360 House of Representatives members are women. The legislature, like many arms of the Federal Government, is an old boys club where girls are not welcome.
[caption id="attachment_1658" align="alignnone" width="640"] Advocacy visit, 8th Senate, 2016[/caption]
Making gains has been difficult. In the previous 8th National Assembly, we came closer than ever before with the passage of transformative legislation. However, with yesterday’s raucous dismissal of the most recent gender-sensitive bills, announced amidst the belly laughs of Senators and Honourables, previously visited by the First Lady, and witnessed on the dire day by the Second Lady respectively, the 9th National Assembly is sending a glaring message to the world: greater political representation of women is not welcome in our hallowed chambers, and within the boundaries and coasts of our shores.
So I find myself asking, like many others, does Nigeria respect the rights of women?
It is greater representation and equality of opportunity that has been proven, through decades and across nations, to be the pivot and the panacea in building and sustaining strong, vibrant democracies. Where calm deliberations around inclusivity breeds responsive policies and enabling environments that are designed for the very people that need them. Yesterday’s actions only reveal that the perceived worth of women, and our ability to lead and participate with effectiveness and substance, to add value to our economies, government and communities - is largely disrespected and grossly undervalued.
Take for instance the matter of citizenship, which has come to be seen as something as universal as DNA - an innate equality. Citizenship is a juristic and political status where the individual enjoys full, legally sanctioned membership in his or her state and owes full allegiance to it, regardless of gender. Yet while a man can pass citizenship to his wife, much like passing on his DNA to his child, the 1999 Constitution discriminates against the woman seeking to pass citizenship on to her spouse. She is denied equal nationality rights, her spouse rendered stateless, unrecognised as a citizen in his wife’s country.
In roughly 50 countries such laws are often the legacy of practices implemented under colonial rule, digging insidious roots in old systems that hold women to be unequal to men. But even Africa is shedding this skin and stepping boldly into modernity. Our neighbours work to secure contemporary Nationality laws that don’t discriminate on the basis of gender and instead align with global consensus embodied through platforms such as the Convention on the Elimination of All Forms of Discrimination against Women (CEDAW), which explicitly obliges States to guarantee equal nationality rights to women (Article 9). Gender equality can never be realized in a country that maintains gender-discriminatory nationality laws.
But the actions of the 9th National Assembly go beyond equality. It reflects the lack of equity and opportunity for women and girls, and our entire female gender, under the Constitution. There is no justice for women without equality.
If understanding justice to be righting the wrong and compensating the marginalised - our lawmakers recognise no injustice.
The bill for Affirmative Action for women in political party administration and leadership has its foundation in this understanding of compensatory justice- that through greater representation, we are securing a systematic way of “righting the wrong'' for women, achieving both equality and reparation, without force. We have seen this approach come to life in countries like Rwanda and South Africa who have used a quota system to pave the way for women representation in politics. In Rwanda, over 50% of political positions are held by women and we see a similar case in Ethiopia’s 50% women cabinet. Role models have been nurtured, and pave the way of other women to rise to positions of power and aspire to leadership positions. Affirmative action is not the end, but merely a means to promote true, lasting diversity and open the gateways for political, economic and social equality.
For so long, Nigeria’s women have been handed the crumbs of the national cake, forced into a silent corner, only to cry into an open void. But enough is enough.
The state of our nation will never improve, until our representatives actually respect and accurately reflect our values, voices and realities, break the bias and ultimately balance that reflection with our national aspiration.
I remain dismayed not only because yesterday was truly a dark day of discrimination against women in Nigeria and indeed for women all around the world. But because I believe this act is beyond ineptitude - and signposts Misogyny: the misogyny against protecting our rights, and chance to live, thrive and flourish equally.
From a civil society perspective, there is a bright klieglight on the pathway to change.
With gender equality fuelling our advocacy and programme strategies, the Wellbeing Foundation Africa has played notable roles in the major events that have shaped the course of campaigns for the rights of women and girls globally since the Beijing Declaration in 1995. Most notably committing to the rise of women and girls through WBFA’s endorsement of The Girl Declaration launched in 2013, as a call to action that aims to ensure that adolescent girls are included in the post-2015 agenda, demanding that governments, organisations, individuals and other stakeholders LISTEN, and the Nairobi Statement on ICPD25: Accelerating the Promise, with its asks and commitments.
[caption id="attachment_1661" align="alignnone" width="638"]
Advocacy visit, 8th Senate, 2016[/caption]
Making gains has been difficult. In the previous 8th National Assembly, we came closer than ever before with the passage of transformative legislation. However, with yesterday’s raucous dismissal of the most recent gender-sensitive bills, announced amidst the belly laughs of Senators and Honourables, previously visited by the First Lady, and witnessed on the dire day by the Second Lady respectively, the 9th National Assembly is sending a glaring message to the world: greater political representation of women is not welcome in our hallowed chambers, and within the boundaries and coasts of our shores.
So I find myself asking, like many others, does Nigeria respect the rights of women?
It is greater representation and equality of opportunity that has been proven, through decades and across nations, to be the pivot and the panacea in building and sustaining strong, vibrant democracies. Where calm deliberations around inclusivity breeds responsive policies and enabling environments that are designed for the very people that need them. Yesterday’s actions only reveal that the perceived worth of women, and our ability to lead and participate with effectiveness and substance, to add value to our economies, government and communities - is largely disrespected and grossly undervalued.
Take for instance the matter of citizenship, which has come to be seen as something as universal as DNA - an innate equality. Citizenship is a juristic and political status where the individual enjoys full, legally sanctioned membership in his or her state and owes full allegiance to it, regardless of gender. Yet while a man can pass citizenship to his wife, much like passing on his DNA to his child, the 1999 Constitution discriminates against the woman seeking to pass citizenship on to her spouse. She is denied equal nationality rights, her spouse rendered stateless, unrecognised as a citizen in his wife’s country.
In roughly 50 countries such laws are often the legacy of practices implemented under colonial rule, digging insidious roots in old systems that hold women to be unequal to men. But even Africa is shedding this skin and stepping boldly into modernity. Our neighbours work to secure contemporary Nationality laws that don’t discriminate on the basis of gender and instead align with global consensus embodied through platforms such as the Convention on the Elimination of All Forms of Discrimination against Women (CEDAW), which explicitly obliges States to guarantee equal nationality rights to women (Article 9). Gender equality can never be realized in a country that maintains gender-discriminatory nationality laws.
But the actions of the 9th National Assembly go beyond equality. It reflects the lack of equity and opportunity for women and girls, and our entire female gender, under the Constitution. There is no justice for women without equality.
If understanding justice to be righting the wrong and compensating the marginalised - our lawmakers recognise no injustice.
The bill for Affirmative Action for women in political party administration and leadership has its foundation in this understanding of compensatory justice- that through greater representation, we are securing a systematic way of “righting the wrong'' for women, achieving both equality and reparation, without force. We have seen this approach come to life in countries like Rwanda and South Africa who have used a quota system to pave the way for women representation in politics. In Rwanda, over 50% of political positions are held by women and we see a similar case in Ethiopia’s 50% women cabinet. Role models have been nurtured, and pave the way of other women to rise to positions of power and aspire to leadership positions. Affirmative action is not the end, but merely a means to promote true, lasting diversity and open the gateways for political, economic and social equality.
For so long, Nigeria’s women have been handed the crumbs of the national cake, forced into a silent corner, only to cry into an open void. But enough is enough.
The state of our nation will never improve, until our representatives actually respect and accurately reflect our values, voices and realities, break the bias and ultimately balance that reflection with our national aspiration.
I remain dismayed not only because yesterday was truly a dark day of discrimination against women in Nigeria and indeed for women all around the world. But because I believe this act is beyond ineptitude - and signposts Misogyny: the misogyny against protecting our rights, and chance to live, thrive and flourish equally.
From a civil society perspective, there is a bright klieglight on the pathway to change.
With gender equality fuelling our advocacy and programme strategies, the Wellbeing Foundation Africa has played notable roles in the major events that have shaped the course of campaigns for the rights of women and girls globally since the Beijing Declaration in 1995. Most notably committing to the rise of women and girls through WBFA’s endorsement of The Girl Declaration launched in 2013, as a call to action that aims to ensure that adolescent girls are included in the post-2015 agenda, demanding that governments, organisations, individuals and other stakeholders LISTEN, and the Nairobi Statement on ICPD25: Accelerating the Promise, with its asks and commitments.
[caption id="attachment_1661" align="alignnone" width="638"]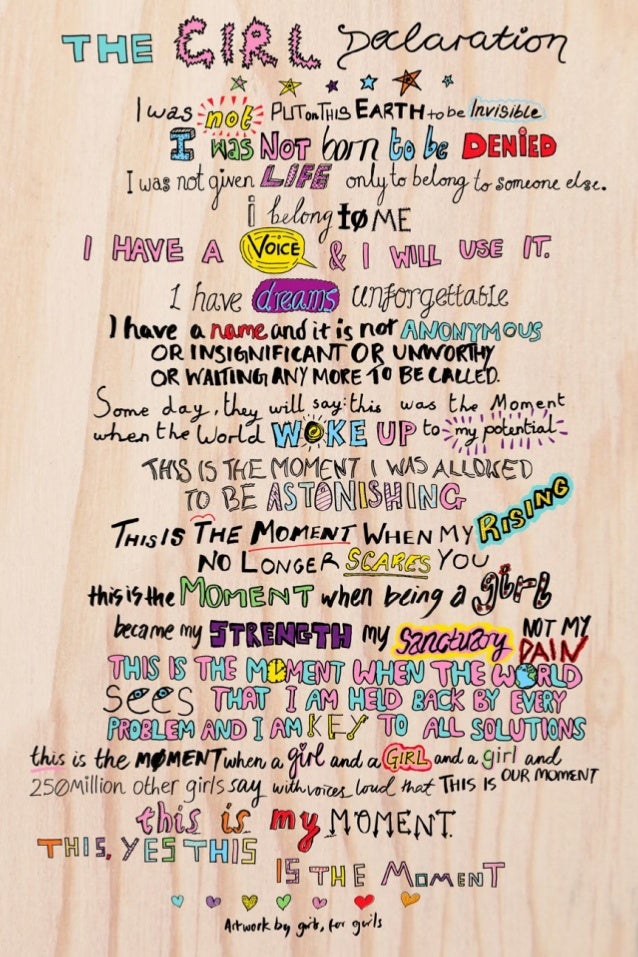 The Girl Declaration[/caption]
The Girl Declaration[/caption]
FROM February 25th, 2022
The WHO and UNICEF recently released their joint findings on the impact of marketing in the sector of formula milk. The study, commissioned by WHO and UNICEF, was undertaken between August 2019 and April 2021 by a specialist research team with commercial marketing and behaviour change expertise, and conducted in eight countries – Bangladesh, China, Mexico, Morocco, Nigeria, South Africa, the United Kingdom of Great Britain and Northern Ireland (UK), and Viet Nam. The largest-ever study of its kind, it draws on surveys with over 8500 pregnant women and mothers of young children (aged 0-18 months) and more than 300 health professionals. The report exposes the aggressive marketing practices used by the formula milk industry and highlights impacts on families' decisions about how to feed their infants and young children. It is apparent from the report that the marketing of formula milk influences our decisions on infant feeding. From the moment you are pregnant, you begin to research best practices to ensure you have the healthiest baby possible. Milk marketing executives are aware of this, and track your interest, logging you on their future sales spreadsheet. By drawing on your fears and insecurities as you navigate your new normal, they spin the truth about their products and utilize trusted sources to spread their misinformation. Formula milk marketing is powered by enormous budgets, which deliberately misuse science for profit. The ingrained messaging in our society is driving the over-consumption of formula milk and discouraging breastfeeding. It is also undermining women’s confidence and cynically exploiting parents’ instinct to do the best for their children. The consequences for children and families are significant, as consumption of milk formula can adversely affect children’s health, growth and development. It can also incur quite significant costs for families who can ill afford it. Let’s be clear: breastfeeding is the best possible source of nutrition for babies. Decades of research continue to reveal the incredible properties of mothers' own milk for growth, preventing infections, bonding, and brain development. Breastfeeding also supports the health of mothers. Formula milk has its place for women and parents who are not able to do so or those who can not do so due to the result of other factors – such as employment that is not supportive of breastfeeding. Yet, breastmilk and breastfeeding still remains the best possible option. Exploitative marketing practices continue to be immensely detrimental to maternal and child healthcare, and global health while feeding a misleading narrative into our communities. We must amplify breastfeeding as the best possible practice. My Wellbeing Foundation Africa is committed to doing so, and throughout our dedicated Alive and Thrive, Mamacare+Nlift, WBFA-Laerdal, and Mamacare360 baby-friendly lactation support promotion programming, and dedicated NICU-specific WBFA-MedelaCares Partnership to help Nigeria's 378,000 premature infants annually receive the benefits of breastmilk, WBFA fully endorses the International Code of Marketing of Breast-Milk Substitutes - The landmark public health agreement passed by the World Health Assembly in 1981. Breast milk helps keep your baby healthy, you healthy, and bonds you together through skin-to-skin contact. It truly is the perfect food for your baby.
FROM February 9th, 2022
2021 Year in Review Presented By Toyin Saraki Global Office & Philanthropy Full circle, reinforcement and replenishment to protect the progress - a healthy future for all. I am honoured to present my 2021 Global Office and Philanthropy Annual Review, based on our core mission, ensuring a healthy future for all. Our current climate inspired my programmatic, communications and advocacy strategy, in what has now become a full circle - reinforcement and replenishment to protect the progress towards a healthy future for all. We saw a metamorphosis take place so that our innovative and dedicated work could remain tenacious, compelling and dependable for all. This achievement embodies our continued labour over 18 years of devoted and enthusiastic philanthropic endeavours, comprehensive frontline programming, and synergetic global partnerships. I consider it an honour and a privilege to continue supporting the Wellbeing Foundation Africa’s 2022 mission and impact, which remains ingrained in our decades of research, awareness and implementation. We look forward to further advancing our goals and targets. You can download my 2021 Annual Review or read it below. [3d-flip-book id="2041" ][/3d-flip-book]
FROM February 7th, 2022
This past week, the Government of Nigeria launched their Revised National Policy on Population for Sustainable Development, emphasizing the immediate measures needed to combat a fertility rate that is increasing exponentially each day. Through expanding access to modern family planning, counseling and commodities, as well as promoting birth spacing, the government aims to improve the standard of living for all Nigerians and improve the health of women and children. Nigeria is the most populous country in Africa and seventh globally, with a fast-rising fertility rate. This, paired with the ever-challenging maternal and childbirth mortality and morbidity indices; and a significant education-occupation mismatch in the context of informality and development, continues to affect our national GDP. Half of the female population in Nigeria are in their reproductive years, and unfortunately, fewer than one out of five married women use family planning. The limited access due to supply chain failure, and lack of investment in education surrounding family planning for young people, has had a detrimental effect on our women, girls and children - putting their health at risk. The COVID-19 pandemic has devastated supply chain systems around the world, making it even more difficult for low-income countries to access potentially life-saving medical supplies and sexual and reproductive health services. While governments, NGOs such as my Wellbeing Foundation Africa, and private sector corporations are working together on innovative methods and policies to overcome these hurdles, the crippling effects will take time to recover from. The reproductive and sexual health commodities supply chain is one of the systems which is suffering, leading to unsafe, unplanned, pregnancies that are fuelling an unsustainable population growth in Nigeria. The larger the population grows without choice and accessible education and healthcare, the more difficulties we will see arise in economic prosperity. A weakened GDP will contribute to higher inflation yet stagnated average incomes fuelling the cycle of poverty which is already deep-seated throughout the Nation. Throughout the pandemic, my incredible WBFA frontline staff and midwives ensured that our Mamacare360 programs were able to continue safely, in an effort to tackle these growing gaps of inequality. Our Mamacare+Nlift in particular focused on family planning alongside IFA supplementation to combat anaemia. We expanded this program by recruiting more midwives and healthcare staff while broadening our reach to more healthcare facilities and healthcare service delivery areas, including home-care service and follow-up. This grassroots advocacy and programme implementation allowed for an increase in local ownership of health services and supply chain management, which ensured improved access and sustainability to family planning programming. Lack of access and supply chain failure are major factors in why women do not use contraceptives or discontinue doing so. Therefore, establishing, maintaining, and strengthening local supply chains is one of the fundamental components in achieving a demographic shift, economic growth and zero unmet need for modern family planning within Nigeria: to work towards a nation where every child is wanted, planned, and nurtured, from birth to age.
View this post on Instagram
FROM January 31st, 2022
On World NTD Day, I was honoured to be recognised by the Crown Prince Court of Abu Dhabi, the Global First Ladies Alliance and The End Fund, for the Wellbeing Foundation Africa's efforts in bringing NTD-education into maternal health check-ups, strong advocacy for investment in WASH services, and helping to recruit more partners and leaders to the fight against NTDs, including the Pharmaceutical Association of Nigeria. The global commitment to end NTDs in the past decade has made for undeniable positive development. As World NTD Week continues, we celebrate our progress, while advocating for the work that remains. Therefore, I am excited to welcome the launch of the Kigali Declaration on neglected tropical diseases – a high-level political declaration that aims to mobilise political will and secure commitments to achieve the Sustainable Development Goal 3 target on NTDs and to deliver the targets set out in the World Health Organization’s Neglected Tropical Disease Roadmap (2021-2030). So far forty-three countries have eliminated at least one NTD, with 600 million people no longer requiring treatment for NTDs. Some of these diseases have plagued humanity for centuries, proving that with dedication and perseverance ending NTDs is possible. The Kigali Declaration allows us to build on these previous achievements by implementing country ownership, highlighting private sector partnership and multilateral collaboration, and putting individuals and communities at the centre of the NTD response. I am proud to pledge my, and my Wellbeing Foundation Africa's ongoing commitment to advocating for embedding NTD services and interventions in our national health systems, ensuring the prioritisation of programmes to prevent, diagnose and treat NTDs are fully resourced and fully integrated, and that women, young people, persons with disabilities, and underrepresented groups are included in this decision-making. We are aware that NTDs are diseases of poverty and inequity. By tackling NTDs through political and policy engagement we will reduce poverty, address inequity, strengthen health systems, and build resilient communities, bringing us closer to achieving universal health coverage - these are a few of the many global health security benefits in supporting national NTD programmes. The efforts to tackle NTDs are a global health success story, but there is still a lot more work to be done before the world is free of NTDs. The Kigali declaration is for, and in service of, the 1.7 billion people who continue to suffer from NTDs. We must hold our ministers accountable, and ask them how the country is working to implement the Kigali Declaration for a brighter future for all. #EndTheNeglect #WorldNTDDay #BeatNTDS #100percentCommitted #LightUpTheWorld
FROM January 21st, 2022
Today on Frontline Friday I would like to highlight an incredible donation from our dedicated partner organisation, Medela Cares. Medela Cares was born out of Medela as a corporate social responsibility program to support the United Nations Global Compact and the Sustainable Development Goals (SDGs). Medela is a global player in breastfeeding research, products, technology and innovation, and is the #1 breast pump brand most recommended by doctors and use in hospitals. Founded in 1961 by Olle Larsson and headquartered in Switzerland, under the leadership of Olle Larsson’s son Michael, Medela has become a driving force in breastfeeding products and medical vacuum technology thanks to continued research, innovation and the evaluation of customers' needs. With my extensive advocacy and promotion on the benefits of early and exclusive breastfeeding for the mum and their baby, it is fitting that Medela Cares has partnered with my Wellbeing Foundation Africa to collaborate on our intrinsic synergies in alignment with UN’s Every Woman, Every Child. Breastfeeding is one of the most effective ways to ensure child health and survival. Breastmilk is the ideal food for infants providing all the energy and nutrients they need, especially premature babies in the NICU who are more susceptible to infections. It is safe, clean and contains antibodies that help protect against many common infant and childhood illnesses. Women who breastfeed also have a reduced risk of breast and ovarian cancers. Currently, Nigeria is the 6th for infant mortality globally, and in children younger than 5 years, 47% of deaths occur in the first 28 days of life, many of which are preventable and can be addressed through improved nutrition with mother’s milk. Unfortunately, Nigeria, with one of the highest premature delivery rates in the world, also has one of the lowest breastfeeding rates in the world with only 17% of mothers exclusively breastfeeding their children through 6 months. To improve these statistics, the United Nations set a global goal to improve breastfeeding rates to 50% by the year 2030, which WBFA and Medela Cares are actively working to reach. Together, Medela Cares and the Wellbeing Foundation Africa are improving the education, tools and support offered to NICU medical professionals and new mothers of premature babies in Nigeria by delivering NICU-specific education and training on the value of human milk and how to build sufficient milk supply for long-term breastfeeding. Ensuring new mothers are wholly supported to breastfeed is not only critical for the health and wellbeing of the baby: it is linked to all 17 of the United Nations Sustainable Development Goals. The Medela Cares life-saving donation to WBFA include:
View this post on Instagram
FROM January 18th, 2022
Wellbeing Foundation Africa and Nutrition International LO-ORS Zinc Case Studies Contribute Key Learning To Nigeria's National Product Supply Chain Management Program. My vision for the Wellbeing Foundation Africa (WBFA) was to build an NGO which promotes an environment where the wellbeing of all can thrive. In which every man, woman, adolescent, child, and infant has reliable, obtainable health care, at all stages of life. Through our vast global partnerships and in alignment with the United Nations Sustainable Development Goals (SDGs) with measurable and meaningful outcomes, we have successfully established this vision and advocated heavily for the betterment of universal health care and practices within Nigeria. This has led the Wellbeing Foundation Africa to actively commit to promoting comprehensive access, availability and management of Nigeria’s Essential Medicines List. One medicine in particular which we have been championing is Zinc and Low-Osmolarity oral Rehydration Solution (LO-ORS) to combat childhood diarrhoea. Diarrhoea is the second commonest cause of childhood mortality among children under 5 years of age globally. Each episode contributes to a significant nutritional deprivation that negatively affects child growth, particularly in more serious and prolonged episodes. The mortality of diarrhoea remains high in Africa, despite being easily treated with Zinc LO-ORS. Within Nigeria, Diarrhoea is the second largest cause of death in children, responsible for an estimated 151,700 children dying in Nigeria every year. It remains an immense threat to child survival in Nigeria with 10% of deaths in children under five resulting from this disease. The national diarrhoea prevalence rate also varies considerably from region to region, with the highest in the North-East and North-West of Nigeria at 24.7% and 14 % respectively, while lowest rate was recorded in the South-West region having a prevalence of 5.3%, largely influenced by socio-economic status of households. Our advocacy efforts bore fruit 2012, when WBFA in collaboration with the WHO PMNCH, UN Every Woman Every Child Initiative, the Clinton Health Access Initiative (CHAI) and the Federal Ministry of Health succeeded in integrating Zinc LO-ORS into Nigeria’s Essential Medicines List, which led to saving over 1,000,000 lives. Nigeria still suffers from a high death rate due to diarrhoea which undermines the accomplishment of the Sustainable Development Goals (SDGs) if left unmanaged, as the understanding and implementation of Zinc LO-ORS is not universally adopted in Nigeria. When WBFA identified these gaps, and that Diarrhoea prevalence and treatment in Nigeria is substantially higher in the Northern regions, we engaged Nutrition International (NI) as a partner to support the Scaling up Zinc and LO-ORS to improve Childhood Diarrhoea treatment in two states - Sokoto and Kano in Northern Nigeria - in order to further improve their performances towards ensuring equity in the distribution of wealth and healthcare services related to diarrhoea management across the country. Our partnership allows both technical and financial support to Kano and Sokoto to address key factors associated with high diarrhoea morbidity and mortality, including the bottlenecks associated with the supply chain in diarrhoea treatment. Therefore, this week the Wellbeing Foundation Africa is extremely proud to be presenting and participating at the Stakeholders Meeting on the National Product Supply Chain Management Program (NPSCMP) New Approaches to DRF/DMA Set-Up. WBFA’s journey in the implementation of Zinc and LO-ORS to improve childhood diarrhoea treatment in Northern Nigeria (Kano and Sokoto State) with a focus on DRF/DMA strengthening is of valuable knowledge for NPSCMP. The Wellbeing Foundation Africa’s ongoing program intervention with Nutrition International implementing - ‘Scaling up Zinc and LO-ORS to Improve Childhood Diarrhoea treatment in Northern Nigeria', supported by the Government of Canada, with a specific focus on supporting states Drug Revolving Fund mechanisms commenced in August 2021 in the two high-burden north-west states of Kano and Sokoto to:
View this post on Instagram
FROM January 12th, 2022
I am delighted to announce that the World Health Organization Foundation has named me their Inaugural Global Health Ambassador. Since the commencement of the WHO Foundation last year, I have been in awe of the dedication, energy and far-reaching ability of the organization to excite the global community towards the shared goal of strengthening our global health ecosystem. In the short space of time since its inception, the WHO Foundation has exemplified tackling the biggest global health challenges collaboratively. Their battle for equity and accessibility throughout the COVID-19 pandemic by way of managing the COVID-19 Solidarity Response Fund (SRF) has been inspiring. Additionally, the launch of the ‘Go Give One’ campaign has created a pathway for an individual to contribute towards vaccine equity, and a strong fundraising drive has led to an impressive $20 million being raised by the foundation in just over six months. This speaks volumes of not only the WHO Foundation’s visionary leadership, but of a united belief that the foundation can truly bring together every global citizen to play a role in world health and address the most pressing health challenges of today and tomorrow, to bring about the necessary change needed. As Founder-President of The Wellbeing Foundation Africa, and having served as a special adviser to WHO AFRO, I have been an active global advocate for women’s and children’s health and empowerment, with my advocacy covering reproductive, maternal, newborn, child and adolescent health; ending gender-based discrimination and violence; and improving education, socio-economic empowerment, and community livelihoods in sub-Saharan Africa. Therefore it feels like a natural progression for the blossoming collaboration between my advocacy, philanthropy, and the WHO Foundation values to unite. I truly believe our intrinsic synergies will create a powerful platform to fight the many challenges faced in global health. As I come into my role, I must acknowledge that now more than ever, it is clear that our health is not guaranteed. While healthcare and life expectancy has made great strides in our lifetimes, there is still much we have yet to understand or uncover, especially when it comes to preventative care. As we continue to see with COVID-19, we are also completely under-prepared to fight new viruses and emerging illnesses. Now with climate change becoming an incorporating factor in healthcare, these challenges, epidemics and pandemics are heightened. Our goal as advocates, thought-leaders, private sector driving forces and changemakers at large, is to support and strengthen the directives and efforts of Governments, CSOs, Policymakers and Agents of Change. Moving forward, societal support must look like contributions; financial and otherwise - particularly from the private pillars within society, industry influencers and members of the public. Global health needs us all, from every country, to work as one. We must all dedicate ourselves to keeping the world safe, and advocate for the protection of the most vulnerable. By working together, we can change the lives of future generations. I look forward to propelling one of the world’s most influential global health initiatives forward through the joint force and work we have initiated. We have set out to protect the health and well-being of everyone, in every part of the world, and I am honoured as the Inaugural Ambassador to reiterate my commitment to the development, growth and mission of the WHO Foundation, and to support the World Health Organization (WHO) and the global health community. Official Press Release
View this post on Instagram
FROM December 12th, 2021
Women deserve to live without fear of harassment or violence! I was honoured to join Global Citizen, UN Women, the Federal Minister of Women Affairs and several active national organisation in vowing to raise our collective voices to improve the lives and outcomes of the world’s most marginalised and vulnerable people - at the Global Citizen High-Level Roundtable in Abuja focused on ‘Action Against Gender-Based Violence: Full Domestication of VAPP Act by All States in Nigeria’. As a female leader, and Founder and President of The Wellbeing Foundation Africa, an NGO which works to improve health and wellbeing outcomes for women, infants and children, advocacy for women and children across Nigeria and the topic of gender-based violence is extremely near and dear to me. We are currently in the midst of a shadow pandemic that affects women and girls disproportionately. Gender-Based Violence remains a scourge in Nigeria society where women and girl children are more at the receiving end than their male counterparts. 30% of Nigerian women have experienced physical violence by age 15 and 28% of Nigerian women aged 25-29 have experienced some form of physical violence (NDHS 2013). From female genital mutilation to early forced marriage being a cultural norm in Nigeria, with 43% of girls married before the age of 18, Nigeria is currently ranked as the 7th most dangerous country for women to live in. GBV remains an oppressive form of gender inequality, posing a fundamental barrier to the equal participation of women and men in social, economic, and political spheres. This calls for emergency and urgent action to protect women and girls in our country. Much work has been done since 2012’s ‘Reducing Domestic Violence Campaign’when an unprecedented and independent WBFA survey and documentary collaboration with the Global Foundation For Elimination Of Domestic Violence and Peace One Day revealed that 1 in every 5 women in Nigeria had encountered some form of discrimination and GBV. GBV is a ‘secret sin’, many women and girls are victims, yet keep quiet. This is a matter that should never be trivialized. We as a society need to stop providing an environment that condones remaining in abusive relationships and situations. That Reducing Domestic Violence campaign ignited public discourse - and an increase in reporting - yet today in 2021, gender-based violence is still such a prevalent and recurring issue in Nigeria, affecting women and girls of all ages. Not long after, in 2014, Nigeria was confronted with the abduction of the Chibok Schoolgirls, prompting an international and local outcry. Yet, in May of 2020, we lost Vera Uwaila “Uwa” Omozuwa, a 22-year old student at the University of Benin who went to her church to read in a quiet space when she was brutally raped. The viral photos of her bludgeoned body have reverberated around the world, adding fire to the flames of the conversation about brutality, violence and lack of a framework for social justice and responsibility; she died of her injuries on the 30th of May 2020. During that same period of time, in Lagos, 16-year-old Tina Ezekwe was trying to get on a bus when a drunken, corrupt police officer attempted to bribe the driver, leading to a sloppy confrontation and shots fired: the bullet pierced through the upper left side of her lap. The battle to save her life lasted for two days, and she died on the 28th of May 2020. These cases spotlight what has been blindingly evident since the forced abductions of the Chibok and Dapchi Schoolgirls: we are continuously failing our women and girls. When the Violence Against Persons (Prohibition) Act was signed into law in May 2015, it shed a glimmering light of hope for many women and girls across the country. Unfortunately, to date, not all states have passed the Act. With strong advocacy from the Nigerian Governors Wives Forum, UN Women, and Stand to End Rape, we were able to reach 30 out of 36 states which have passed the Act through their state legislative house. This is not good enough, we must amplify and drive the Roadmap to 36 States: Full Domestication and Implementation of the VAPP Act campaign. My organization, Wellbeing Foundation Africa, works to strengthen our primary health, education and workplace structures by integrating PSVI at the frontline will bring equity and efficiency to our preventive and response mechanisms. Because we cannot ordinarily intrude into the home and household behaviours, we need a one-stop approach at our first external levels, at the first outside points of health, work/enterprise and education. Pervasive, gender-based violence is not inevitable - It can and must be prevented. The Wellbeing Foundation Africa creates safe spaces for women and girls by believing survivors, adopting comprehensive and inclusive approaches that tackle the root causes, transforming harmful social norms, and empowering women and girls. This approach has especially been integrated throughout our Mamacare360 Antenatal and Postnatal Community Midwifery and Adolescent PSHE WASH Program which affords professional safe space counselling and referrals in instances of GBV. Through our continuous program delivery, WBFA frontline health workers reach countless pregnant and newly delivered women, adolescent girls, their educators and families each month - and are skilled to provide these resources. The Wellbeing Foundation is also committed to achieving the 3 zeros of Zero unmet needs for family planning and services, zero preventable maternal and infant deaths, zero sexual and gender-based violence including early and forced marriage, as well as female genital mutilation. WBFA is doing so by advancing universal access to sexual and reproductive health, reinforcing the goal to end preventable maternal deaths and empowering the younger generation to know their social, sexual and reproductive health and rights. We must also create a national strategy to educate, empower and heal the nation from the ingrained stigma and predominance of GBV. This would include actualising Nigeria’s National Action Plan on Women, Peace and Security, which incorporates PSVI, accountability and ensuring its adoption is consistent as we continue the advocacy and work. Successful national implementation of the VAPP Act would of course have to take into account the characteristics of Nigeria and our people. In our culture, we do not like to talk about sexual violence - consider what it must be like for those in a conflict setting; for the marginalized women and girls who are already on the brink of being bereft of all their rights. When the empowered ones amongst us do not like to talk about it, what about the ones with no rights at all? We need to invest in women’s groups to lead grassroots efforts and engage with political and religious leaders so that we can shift the shame and stigma of sexual violence from the victims onto the perpetrators and get this act signed in the last remaining six states. In November 2019, I joined the Commonwealth Secretariat in launching the Commonwealth Gender Equality Policy and the Commonwealth SAYS NO MORE Initiative at the kind invitation of Secretary-General Patricia Scotland, to raise public awareness of Violence Against Women, to measure progress towards eliminating it, and to continue to mobilise people everywhere to bring about change by leveraging successful strategies to end domestic violence and sexual assault. If we strengthen our global, national and sub-national community as a whole beyond the government, then that community is better placed to support those in distress; those who have been the victim of conflict and sexual violence. This is a necessity that must resonate across all our states. The African continent, and Nigeria within it, are facing a displacement and refugee crisis. We must create a model which aids survivors in Northern Nigeria and IDP camps - one which uses public hospitals as a base to provide comprehensive services which each survivor needs - medical care, psychosocial support, police and legal support, and a collection of legal evidence. We know that in some cases women in displacement camps in Nigeria have resorted to exchanging sex for food or money, so they can feed their families. A national strategy must restore dignity and safety to these women, no woman or child should ever be forced into sexual transactions, begging for change or modern slavery for survival. I would like to see the mainstreaming of counsellors and clinics in every camp so the help is there where needed, and a formal referral mechanism between the camp authorities and humanitarian organizations so that displaced women and girls can, as standard, access gender-based violence screening services. Let's start with asking women if they have been the victim of bullying; rather than even talking about violence immediately. That way we won’t miss the issue, because someone who is already so vulnerable is far more likely to confess to being bullied or coerced than to rape or sexual violence. Following the lockdown during the COVID-19 pandemic in 2020, where there are restrictions to movement and families staying together more, the incidence of GBV grew exponentially, leaving the more vulnerable gender to groan in silence. The Wellbeing Foundation Africa, through our midwives, was at the forefront of campaigning and advocating against any form of physical, sexual, emotional and psychological abuse, threats, coercion and economic or educational deprivation against women and girls. Unfortunately, there was an upsurge in reports of rape across Nigeria during this period. Rape still remains at an epidemic level in Nigeria, and there are no accurate statistics on its prevalence. Most cases of rape go unreported, due to the fear of stigmatisation, victim-blaming and a lack of trust in the police and judiciary. In 2019, I had advocated for SARC Centres to be established at hospitals - GBV cases should be promptly prosecuted within reasonable timeframes, and in line with the law, regardless of interference by interested parties. Through this, we can begin to build trust and data which will help inform the national strategy and create a safer Nigeria. As the pandemic persists, we cannot afford to see another 297% increase in reported domestic violence as we saw between March and April of 2020 in Lagos, Ogun and Abuja. The VAPP act also needs to be wholly adopted, as some states which have passed the act are significantly reducing punishments for violence against women and girls. There should be no modification or lessening of this act, we cannot afford for more women and young girls to lose their lives in vain with no justice whatsoever. It is time for accountability. We need to not only involve civil society but also the duty bearers. The main duty bearer here is the Government which should set up a proper social referral system within existing structures. We must call for more collaboration among states, non-governmental organisations, civil society organisations as well as government agencies such as the National Agency for the Prohibition of Trafficking in Persons to expose and prosecute sexual offenders, and promote the implementation of VAPP across the remaining states. Therefore, today on behalf of all Nigerian women and girls, I would like to restate the demand for the domestication of the VAPP Act in all 36 States and the FCT to enable a nationally coordinated implementation strategy against GBV. Until all 36 states are on board, we will not be able to build standard services across the nation, which we need to respond to individuals, families and communities facing this crisis. Thank you to everyone who has joined the discussion today to commit to preventing gender-based violence in Nigeria and for your ongoing partnership in this area. I look forward to further discussions and, most importantly, joint and collaborative actions, together - to normalize and mainstream PSVI actions until ending gender-based violence is our standard and regular routine community of practice.
FROM December 4th, 2021
I was pleased to join the UNHCR at the 36 Million Solutions: Africa Private Sector Forum on Forced Displacement throughout the week. From my important high-level yet candid bilateral conversation with UNHCR Deputy High Commissioner, Kelly T Clements, to joining Michel Sidibé of the Africa Union Special Envoy for The African Medicine Agency, Dr. Githinji Gitahi - CEO Amref Health Africa, Diana Mulili - Chief Growth Officer at Xetova and Nancy Moloantoa of Open Society Foundation on the panel for Inclusive Health Systems - The Only Way, this week highlighted the importance of uniting Africa’s business and industry leaders with philanthropists, refugee change-makers, and the public sector when designing market-based approaches to leverage the potential and power of the 36 million solutions who are forcibly displaced across our continent. Africa hosts the largest number of forcibly displaced persons worldwide: 36 million. 36 million families and neighbours. 36 million customers and suppliers. 36 million innovators, entrepreneurs, and employers. The intimate forum and gathering hosted by the UNHCR was a unique opportunity to inspire and encourage African-led solutions to the issues of forced displacement across our continent. As an advocate for healthcare - I was pleased to join the panel for Inclusive Health Systems - The Only Way. Every person deserves the right to dignified healthcare, regardless of their migration status. Yet, health systems too often fail forcibly displaced people, who already face numerous obstacles in accessing high-quality care. COVID-19 has exposed the inequities in healthcare and the reality that its delivery cannot be separated from the unique economic, cultural and social circumstances of communities in need. African countries have historically opened their borders and hearts to families fleeing war, violence, conflict, or persecution. Countries that receive and host refugees, often for extended periods, make an immense contribution from their own limited resources to the collective good and to the cause of humanity. In Nigeria for example, we have 3 million people internally displaced and another 74,000 refugees and asylum seekers. Many of these people have been in this situation for years, and greater support and services are required to help them rebuild their lives. Along with this, we have a population of 206 million people with nearly half living below the poverty line. These numbers may give us insight, but they often fail to tell the full story of the dire situation that has befallen so many due to the lack of universal health care or access to healthcare that can allow people to live longer, increase their incomes, and lead to positive socio-economic gains for their families. The major constraint of our current system is that vulnerable people usually lack the funds to pay for healthcare. Health care financing in Nigeria is mainly through out of pocket payment, and most people cannot afford to pay. Another challenge we face is the quality of health care available in most rural communities. The system is very weak, even our best hospitals have poor infrastructure, with few properly trained personnel, very little equipment, and a lack of sustainable medications supply model. Combining both of these with a lack of education surrounding maternal health, creates a critical and urgent situation for many women, children and vulnerable people in Nigeria. My Wellbeing Foundation Africa has operated for close to 20 years with a set of 10 core rights-based principles to improve the health and wellbeing of childbearing women and their newborns. We believe that we must support a call to mobilise resources to deliver the same standard to the women and children of Nigeria, and refugee and displaced communities:
FROM November 30th, 2021
The marginalised can not continue to be penalised for circumstances beyond their control. The Wellbeing Foundation Africa joins Women in Global Health, and the World Health Organization member states and non-states in the timely and important discussions regarding the Pandemic Treaty this week. For the Treaty to strengthen pandemic prevention and responses, it must also recognise the consistent inequalities faced throughout COVID-19 and ensure equitability is highlighted. Gender equity in particular must be at the forefront of our post-pandemic rebuild. Creating a healthier, safer, and fairer world, means advocating for the most vulnerable through prioritizing human rights, gender mainstreaming, universal health system strengthening and improved funding mechanisms. As the 16 Days of Activism against Gender-Based Violence continues, we have seen first-hand how the pandemic increased the care workload, obstructed access to sexual and reproductive health services, and increased violence for women and girls primarily. Yet, women’s experiences and voices continue to be marginalised. The WHO must promote gender parity and diversity in COVID-19 leadership. Women and girls in the Global South have been disproportionately impacted throughout the pandemic and this has penetrated into the healthcare system as well. Women make up 70% of the health workforce yet are still overlooked, with COVID-19 task forces globally only having 24% representation from women. Women must be participants in all stages of decision-making processes, and mainstream a gender perspective in the COVID-19 response and recovery. This extends to scientific advisor groups, panels and consultations as they have the first-hand experience to provide an insight that will design a resilient, accessible and quality care health system. This evidence-based policy making and advocacy, paired with enhanced data collection and analysis will enable better health and social outcomes to occur. These critical issues filter into establishing a human rights first approach. Equitable universality principles must be embodied throughout our future preparedness and response so that we can properly assess and provide support to infection and incidence. This includes collaboration with human rights and civil society groups in preparedness, as they are at the frontlines bearing the brunt of the epidemic lifecycle on the most vulnerable groups. A well-assessed treaty will improve human rights obligations while augmenting the existing international human rights law and standards. Currently, fewer than 6% of people in the African continent have been fully vaccinated against COVID-19, with health workers and vulnerable populations still waiting for their first dose. This is due to a lack of funding and inequitable access, which plays a critical role in the surveillance of emergent variants. We cannot ignore the hardest hit and most vulnerable populations during a public health emergency. Funding mechanisms must be expanded to reach low-income countries, possibly with a system in place for high-income countries to support low-income countries in an accountable manner. By the end of 2022, over 12 billion doses of vaccines will have been produced, enough to vaccinate the entire world, yet we still face such low-rates due to accessibility and information access issues in the Global South. We are exhibiting first-hand the global inequality that has led to a grossly uneven distribution of vaccines, vital healthcare tools and PPE which has made fragile health systems crumble throughout developing nations. To tackle this, the Treaty must commit to sharing knowledge, data, information, and resources to create a worldwide health system that is ready to respond to the next pandemic. This One Health approach will foster trust and accountability, allowing pandemic preparedness to become standard. Of all Wellbeing Africa Foundation programming across Nigeria, the 2 programs that were most prophetic of the skills and capacities needed to combat COVID-19 during the restrictions of socially distanced physical lockdowns, were the organic introduction of Mamacare360 and MaternalMonday Whatsapp Groups to continue the conversations in our Mamacare360 antenatal and post-natal classes, along with WASH For Wellbeing program, teaching clean hygiene to mothers and medical workers in HCF, and its counterpart Primary and Adolescent PSHE-WASH in Schools. These focused platforms were initiated in April 2018, as responsive commitments to both the UN Secretary General’s call for improved WASH, the WHO Resolution on Hygiene in Health Care Facilities, and the WBFA stark finding that only 22% of Delivery Rooms in Nigeria had direct access to a basin, soap, and clean water. As Covid-19 appeared, WBFA was positioned in 670 communities, to ramp up the key learnings for social behavioural change, right in the communities and households, schools and marketplaces where trusted learning needed to reach. The Wellbeing Foundation Africa continues in its quest to develop a concrete Nigerian-wide public health informed approach that looks at the factors and responds with key actions for individual women, children, their families and the schools and health facilities within their communities in which they live that make it more or less likely that vulnerability and adversity in childhood has a lasting impact on their lives. A holistic inclusive approach, that takes the community midwifery approach further into a school nurse-visitor information, education and learning approach, and a reporting index will address inequality and the broader causes of vulnerability which might otherwise be overlooked to support decision-making and prioritisation. The Wellbeing Foundation Africa is leading a Call-To-Action for: Implementation of Gender Mainstreaming Strategy: Vaccine Equity; Funding Stronger Healthcare Systems and Consistent Respect for Human Rights. Universal Health Coverage must be assessed by the states in Nigeria as primary health services should be accessible to all during all health crises. Women health workers are our global health security, they deserve better, they need better pay and leadership opportunities. As the pandemic persists they continue to be mentally exhausted and undervalued. For this Treaty to produce viable outcomes, it must recognize that our global health emergency responses cannot be constructed on the most vulnerable and marginalized women. It is clear that an equity-first approach will be needed to tackle these severe disparities, and those with a voice must advocate for that equity so that we may rebuild and re-envision a stronger healthier world.
FROM November 26th, 2021
I am delighted to start this year's 16 Days of Activism by advocating to the participants of the National Institute for Legislative and Democratic Studies NILDS, United Nations Development Program UNDP and the United Nations Entity for Gender Equality and the Empowerment of Women UNWomen Capacity Building Workshop for Female Legislators and Female Politicians on Lawmaking and Lobbying, at Abuja. It is indeed a very timely initiative, as today, November 25th, marks the start of 16 Days of Activism and activities marked annually, to highlight Ending Violence Against Women and Girls. As a Pioneer Member and Steering Council Member of the UN Women’s African Women Leaders Network Initiative globally and in Nigeria respectively, I am thrilled that this workshop will inspire new energy and technical skills needed to accelerate working together for Gender Equality, namely: - Women’s Political Participation - Women’s Economic Empowerment - Women Peace And Security and Humanitarian Action - Ending Violence Against Women Thus, the enactment of gender-sensitive legislation and domestication of international conventions, statutes and promotion of women's participation in politics and governance in Nigeria is on the front burner of gender equality and the empowerment of all women and girls for a just and fair society (a pointer to SDG 5). Lack of political representation is a major cause of both gender inequality and generation inequality. Of all national parliaments at the beginning of 2019, only 24.3% of the seats were filled by women. As of June 2019, 11 Heads of State were women. Despite progress in this area over the years, women are still grossly underrepresented in government and the political process. This means that certain issues that female politicians tend to bring up- such as parental leave and childcare, pensions, gender equality laws and gender-based violence are often neglected. Regarding the target of generation equality, the Wellbeing For Women Africa Youth Voices Initiative's 2020 Wa Wimbi Report found that the political, social and economic dispensation in Africa is highly defined and structured whereby culture defines the socio-economic and political discourse. Furthermore, there are pockets of scenarios where leadership is passed from masculine generation to generation. Potentially, these situations can lead to conflicts and partisan control of public resources and access to opportunities. While these factors are not solely the causes of strife and conflict - where women suffer the most - they are a catalyst. Through human capital development especially for young people, there are opportunities to initiate and drive socio-economic processes to socially and economically empower young professional women. As a build-up to this action, the WBW Youth Voices Initiative engaged its youth partners to conduct a survey, the primary objective of which was to provide empirical data on probable bottlenecks faced by young women in access to and uptake of leadership and decision-making opportunities across Africa. The survey sought to: a) Collect and analyse cultural and socio-economic scenarios faced by young women in leadership and decision making spaces; b) Analyse the current employment market to identify professional opportunity trends where sustained and dignified professional engagements are attained based on merit; c) Document constraints and barriers faced by young and vulnerable women in the labour market; and, d) Provide an analytical review of the most viable scenarios that could help young women as beneficiaries. The study included a total of 239 participants both on and offline, there were 75 online respondents, 19 KII and 145 participants from 15 FGD. The study involved responses from 18 African countries namely Botswana, Burkina Faso, Comoros, Cameroon, DRC, Egypt, Ghana, Eswatini, Kenya, Lesotho, Malawi, Morocco, Mozambique, Seychelles, South Africa, Uganda, Zambia and Zimbabwe. According to this survey on the bottlenecks women face in leadership and governance, on a broad scale, most respondents find women indistinguishable from men on key leadership actions such as influence, merit, capacity and mental willpower to lead, organise and implement. The study analysis presented in this report confirms that presently, leadership and governance are dominated by men despite the existence of administrative and policy provisions in many organisations seeking to frontload women as equals in merit. Furthermore, the submissions by the survey respondents indicate that whilst there is a general push for women to take up leadership positions, as evidenced in access to leadership spaces (albeit limited), policy provisions and merit over gender among others, there are still overbearing social and cultural norms which seem to continually limit the spaces and counter strides made. Young women’s leadership is undermined in the civic space despite the advances in youth engagement over the years. The current configuration of youth organisations is not enough to ensure or sustain the effective leadership of young women in international development and any progress within youth spaces is still largely affected by the preferences of young men in power. Within the current global context, women are given promises of equal representation but often find the reins of power in the hands of others. To improve access to leadership and governance spaces in a demand-driven system in the context of development, it is imperative to involve women in all components of development programming. Institutions must recognise and take up this driving factor as an enabler to achieving equity and ensuring strategic opportunities for all. One of the core objectives at WBFA is advocating for gender equality with the acknowledgement that the status of women, children and families in Africa require improved resources, support, and advocacy. Our policy goals on women, girls, and gender development span various interventions with a core towards advocating for the right of every woman to leadership and political participation. This is achieved by promoting women’s leadership and participation in all sectors, ensuring that women are accorded equal opportunities and supported to lead and participate in politics either through elections or by appointments. It is for this very reason that my Wellbeing Foundation Africa is committed to its ongoing leadership of Nigeria Country Mobilisation for the ICPD25 International Conference on Population and Development Commitments towards the 3 zero’s of: 1) Zero Preventable Maternal Deaths, 2) Zero Unmet Need for Family Planning, and 3) Zero Sexual and Gender-Based Violence. While we commend the passage and implementation progress of the VAPP Legislation, tangential to these targets, there is a need to continue to work collectively towards the prevention of sexual violence in conflict (PSVI), and the domestication of United Nations Security Council Resolution 1325 on Women Peace and Security. We must also redouble efforts towards the reintroduction and eventual passage of the Gender Equality and Opportunity Bill into law. Therefore, it is my hope that the participants at this 2-day event will leverage on knowledge gained to stimulate their interest more in lawmaking and lobbying and equip themselves with the technical capacity on legislations and domestication of international conventions and statutes with the desired outcomes of increasing women in politics and leadership positions to make positive impacts that will continue to make the world a better place.
FROM November 23rd, 2021
I am delighted to announce the launch of the field implementation component of the Wellbeing Foundation Africa and Nutrition International Scaling Up Zinc and LO-ORS project to combat diarrhoea in Kano and Sokoto states in Nigeria. The project is funded by the Government of Canada and seeks to increase timely care-seeking and treatment of diarrhoea with zinc and low-osmolarity oral rehydration salts. In partnership with the Ministries of Health in both states, my Wellbeing Foundation Africa and Nutrition International will target caregivers with messages promoting prompt care-seeking for children with diarrhoea and adherence to treatment with zinc and LO-ORS. As the implementing partner on the Wellbeing Foundation Africa-Nutrition International Scaling Up Zinc and LO-ORS Project in Kano and Sokoto states, I am delighted that this intervention is aptly taking place at a time when diarrhoea and other water-borne diseases are threatening the livelihoods of Nigerians, especially in the northwestern part. We are grateful to the Ministry of Health, State Primary Health Care Development Agencies and other ministries, departments and agencies within the states for their dedication and commitment to this project, and also to all the frontline health workers who are leading the charge to curb the menace of diarrhoea within northwestern Nigeria. The states will also receive technical and financial support to build the capacity of healthcare providers to treat diarrhoeal cases with zinc and LO-ORS and communicate with caregivers about the treatment, ensuring they can provide care for cases seen in health facilities or within the community. Nutrition International truly believes in enhancing child survival, and that scaling up zinc and LO-ORS to improve childhood diarrhoea treatment contributes heavily to that. Diarrhoea is preventable and we must focus on continuously improving our prompt health-seeking behaviour, while sustaining availability and access to quality zinc and LO-ORS in public health facilities in the states. The project has already trained nearly 200 health workers and administrators of selected primary and secondary health facilities in Kano and Sokoto states. By 2023, we are looking to increase the number of caregivers who seek prompt care for cases of childhood diarrhoea by an additional 2,238,439. Diarrhoea is a leading cause of malnutrition and death in children under the age of five, and malnutrition is also known to prolong episodes of diarrhoea and increase mortality. That is why it is essential for a project like this to be in place, training and retraining health workers on the integrated management of childhood illnesses to enhance the capacity of the health workers.
FROM November 16th, 2021
As we mark the second anniversary of the Nairobi Summit, stakeholders across the globe are firmly voicing their recommitment to the implementation of the ICPD Programme of Action. A landmark moment, in which various interest groups came together in partnership, recognizes the accelerated efforts needed to make progress in gender equality, youth, political and community leadership, and innovation and data. This reinvigorated engagement launched at a challenging time, as only months later, the world grappled with the COVID-19 pandemic. Throughout this period we have seen how crucial it is to immediately address various issues from the Summit, particularly in the realm of sexual and reproductive health and rights. The Wellbeing Foundation Africa prioritizes the most amplified issues from the summit; having a global impact that advocates for women, children and families, through empowering and educating frontline health workers while increasing accessibility to health care and proper hygiene. As a community stakeholder committed to the Summits re-emphasized themes, WBFA is committed to; zero unmet needs for family planning and services, zero preventable maternal and infant deaths, zero sexual and gender-based violence including early and forced marriage, as well as female genital mutilation. WBFA is doing so by advancing universal access to sexual and reproductive health, reinforcing the goal to end preventable maternal deaths by creating safe spaces, and empowering the younger generation to know their social, sexual and reproductive health and rights. WBFA is doing so through the implementation of various programs such as our Mamacare360 Community Midwifery Antenatal and Postnatal Education Program which reaches on average 3700 women per month across Nigeria and delivers improved health outcomes and empowerment through education for women to make informed health decisions. To date, the program has serviced over 200,000 women. WBFA’s Adolescent Skills and Drills PSHE WASH Program also promotes respectful rights and relationships, highlighting the need to end gender-based violence and harmful practices by providing safe space counselling and access to Sexual Assault Referral Centres which reach over 1000 adolescent girls, their educators and families each month. These are just a few of the many programs initiated by WBFA which reflect our commitment to ICPD 25. These measurable actions allow us to learn and reflect as an organization, but also on a global level as we work towards a gender-equal and healthy community across the globe. As WBFA actively works towards exceeding our goals, we want to promise that we will, and encourage our counterparts to, transparently report on progress made to fulfil these commitments. Open discourse and collaboration will be the only way to support one another and facilitate re-building back better from COVID-19 and reaching our longstanding goals. Accountability is key. WBFA also welcomes voices from all paths, as we need young and diverse perspectives in leadership to monitor the commitments made. This is our opportunity to build a stronger health system with a higher quality of care that is tailored to various groups. As the summit was non-binding, countries and stakeholders have a choice in choosing to support the Nairobi Statement in part, entirety or not at all. That is why emphasis needs to be put on the anniversary of the Nairobi summit, as meaningful follow-up and encouragement will ensure commitments remain in the forefront and can be done so in a timely and actionable manner. We are proud to witness and report on the progress that has been made, yet there are still millions of vulnerable women and girls around the globe waiting to see their promises be fulfilled. We must raise our voices and continue to march forward to create a systemic difference so equality and safety can prevail.
FROM November 9th, 2021
I am so pleased to usher in Gender Day at the COP 26 joint session with the start of the Reykjavík Global Forum - Women Leaders, chaired by the Head of WP Leaders, distinguished Prime Minister of Iceland and honourable Speaker of Parliament. Discussing the climate crisis through a gender lens has never been so pertinent. Gender Day affords us the opportunity to recognise, and celebrate, gender equality and the empowerment of women and girls in both climate policy and action.
 Women continue to be disproportionally at risk for violence, discrimination and disenfranchisement around the world. But there is reason to hope. In “Finding the Path to Net Zero’ I thoroughly enjoyed the rich perspectives from my fellow panelists Marjut Falkstedt, Secretary General of the European Investment Bank, Sarah Riggs Amico, Executive Chairperson, Jack Cooper Holdings Corp, and Adenike Oladosu, Climate Activist; Founder, ILeadClimate in a reveling conversation moderated by Bayartsetseg Jigmiddash, State Secretary of Justice, Mongolia 1 (2012-2016), Senior Prevention Specialist, Green Climate Fund. Sharing pertinent point of views from industry, finance, agriculture and beyond, all ensuring that gender equality and women’s human rights are central to ongoing discussions.
It is clear that COP26 has brought people, the planet, and prosperity together in an inspiring and energising way.
Global leaders have presented that they understand the urgency, but there is still more work to be done in recognising the frontline challenges of health and well-being in regards to the climate crisis and leveraging local knowledge and action.
Women continue to be disproportionally at risk for violence, discrimination and disenfranchisement around the world. But there is reason to hope. In “Finding the Path to Net Zero’ I thoroughly enjoyed the rich perspectives from my fellow panelists Marjut Falkstedt, Secretary General of the European Investment Bank, Sarah Riggs Amico, Executive Chairperson, Jack Cooper Holdings Corp, and Adenike Oladosu, Climate Activist; Founder, ILeadClimate in a reveling conversation moderated by Bayartsetseg Jigmiddash, State Secretary of Justice, Mongolia 1 (2012-2016), Senior Prevention Specialist, Green Climate Fund. Sharing pertinent point of views from industry, finance, agriculture and beyond, all ensuring that gender equality and women’s human rights are central to ongoing discussions.
It is clear that COP26 has brought people, the planet, and prosperity together in an inspiring and energising way.
Global leaders have presented that they understand the urgency, but there is still more work to be done in recognising the frontline challenges of health and well-being in regards to the climate crisis and leveraging local knowledge and action.
NGOs such as my Wellbeing Foundation Africa, therefore, play a vital role in not only establishing their own mission and work but aiding vulnerable communities in adapting and understanding the effects of the climate crisis as it is interlinked with almost every aspect of life, particularly health care. Human lives and health are being impacted in a variety of ways, from a lack of clean air, safe drinking water, nutritious food supply, and safe shelter. These challenges will only worsen if we do not act immediately. That is why WBFA will be working with our partners to enable and encourage countries affected by climate change to; protect and restore ecosystems, build defences, warning systems and resilient infrastructure and agriculture to avoid loss of homes, livelihoods and even lives. Global political leaders need and must continue to work with NGOs to understand that inaction on climate will also set us back decades in the societal missions and advancements made by NGOs for those who are already marginalized and disproportionately affected.View this post on Instagram
FROM October 29th, 2021
I am delighted that my Wellbeing Foundation Africa has commenced its partnership project with Nutrition International and the Governments of Kano and Sokoto States in Scaling up Zinc and LO-ORS to Improve Childhood Diarrhoea treatment in Northern Nigeria.
 Childhood diarrhoea remains a threat to child survival in Nigeria; 10% of deaths in children under five are due to this disease. The country still records national prevalence as high as 13%. State-specific variations in prevalence of diarrhoea are also recognised; the prevalence in the north-western states is considerably higher at 20.7% in Kano, 18.6% in Katsina, and 21.7% in Zamfara.
While the number of global under-five deaths dropped to its lowest point on record in 2019 – down to 5.2 million, from 12.5 million in 1990, there are fears that numbers could rise on the back of COVID-induced disruptions to child and maternal health services, recent estimates from UNICEF, indicate.
Over the past 30 years, health services to prevent or treat causes of child death such as preterm, low birth weight, complications during birth, neonatal sepsis, pneumonia, diarrhoea and malaria, as well as vaccination, have played a large role in saving millions of lives, added the agencies.
Accelerating Frontline practices is an essential factor in improving health for all.
In seeking to contribute to reducing the number of deaths due to diarrhoea among children under five In Nigeria, the project is providing both technical and financial support to Kano and Sokoto to address key factors associated with increased diarrhoea morbidity and mortality - supporting the promotion of prompt care-seeking for children with diarrhoea among caregivers as well as adherence to standard treatment (zinc and low-osmolarity oral rehydration solution [LO-ORS]).
Childhood diarrhoea remains a threat to child survival in Nigeria; 10% of deaths in children under five are due to this disease. The country still records national prevalence as high as 13%. State-specific variations in prevalence of diarrhoea are also recognised; the prevalence in the north-western states is considerably higher at 20.7% in Kano, 18.6% in Katsina, and 21.7% in Zamfara.
While the number of global under-five deaths dropped to its lowest point on record in 2019 – down to 5.2 million, from 12.5 million in 1990, there are fears that numbers could rise on the back of COVID-induced disruptions to child and maternal health services, recent estimates from UNICEF, indicate.
Over the past 30 years, health services to prevent or treat causes of child death such as preterm, low birth weight, complications during birth, neonatal sepsis, pneumonia, diarrhoea and malaria, as well as vaccination, have played a large role in saving millions of lives, added the agencies.
Accelerating Frontline practices is an essential factor in improving health for all.
In seeking to contribute to reducing the number of deaths due to diarrhoea among children under five In Nigeria, the project is providing both technical and financial support to Kano and Sokoto to address key factors associated with increased diarrhoea morbidity and mortality - supporting the promotion of prompt care-seeking for children with diarrhoea among caregivers as well as adherence to standard treatment (zinc and low-osmolarity oral rehydration solution [LO-ORS]).
 The WBFA is dedicated to implementing targeted technical and financial support to improve the capacity (knowledge, skill and attitude) of health care providers to provide quality zinc and LO-ORS and appropriate interpersonal communications for the treatment of all diarrhoea cases seen at health facility or community level service points. In addition, we aim, supported by Nutrition International, to improve the commitment of state actors, such as health managers and policy makers, to implement complementary drug revolving fund (DRF) schemes for effective availability and sustainability of health commodities, including zinc and LO-ORS.
The WBFA is dedicated to implementing targeted technical and financial support to improve the capacity (knowledge, skill and attitude) of health care providers to provide quality zinc and LO-ORS and appropriate interpersonal communications for the treatment of all diarrhoea cases seen at health facility or community level service points. In addition, we aim, supported by Nutrition International, to improve the commitment of state actors, such as health managers and policy makers, to implement complementary drug revolving fund (DRF) schemes for effective availability and sustainability of health commodities, including zinc and LO-ORS.

FROM October 1st, 2021
 61 years after Nigeria seized the reins of independence, October 1st is a day of national reflection. The task of nation-building is a lengthy and laborious endeavour and honest introspection of our collective gains and losses must be undertaken as we map our path forward towards the goal of shared peace and prosperity.
Nigeria’s achievements in human-centred development are not in question.
We have excelled and exceeded in a multitude of fields with legacies in business, sports, the arts and science etching the knobs and shifting the dials on the various indicators by which we measure national ‘success’.
Yet these successes have an overriding common factor: They have been steered, achieved, and celebrated predominantly by male figures.
61 years after Nigeria seized the reins of independence, October 1st is a day of national reflection. The task of nation-building is a lengthy and laborious endeavour and honest introspection of our collective gains and losses must be undertaken as we map our path forward towards the goal of shared peace and prosperity.
Nigeria’s achievements in human-centred development are not in question.
We have excelled and exceeded in a multitude of fields with legacies in business, sports, the arts and science etching the knobs and shifting the dials on the various indicators by which we measure national ‘success’.
Yet these successes have an overriding common factor: They have been steered, achieved, and celebrated predominantly by male figures.
 Icons and heroines of the past such as activist, political campaigner, and founder of the Nigerian Women's Union, Funmilayo Ransome-Kuti, Margeret Ekpo, the pioneering female politician in the country's First Republic and the architect of modern pottery in Nigeria Ladi Dosei Kwali pushed open the doors of female inclusion and representation in the national space.
Icons and heroines of the past such as activist, political campaigner, and founder of the Nigerian Women's Union, Funmilayo Ransome-Kuti, Margeret Ekpo, the pioneering female politician in the country's First Republic and the architect of modern pottery in Nigeria Ladi Dosei Kwali pushed open the doors of female inclusion and representation in the national space.
 In the male-dominated arena of finance eight women currently serve as Chief Executive Officers (CEOs) or Managing Directors (MDs) of the country’s leading banks. In the fields of human rights and social welfare, in which women remain the conscience of the nation, trailblazers such as Sadiya Umar Farouq continue to fight for increased intervention.
On the global stage, Nigerian women continue to shine, with the World Trade Organization (WTO) being led by Dr Ngozi Okonjo-Iweala, the maverick former Nigerian Minister of Finance. The same level of global trust in the Nigerian women’s ability has witnessed the rise of Amina J. Mohammed as Deputy Secretary-General of the United Nations and Chair of the United Nations Sustainable Development Group, whilst in the field of literature Chimamanda Ngozi Adichie continues to keep the world spellbound, engaged and mesmerized.
In the male-dominated arena of finance eight women currently serve as Chief Executive Officers (CEOs) or Managing Directors (MDs) of the country’s leading banks. In the fields of human rights and social welfare, in which women remain the conscience of the nation, trailblazers such as Sadiya Umar Farouq continue to fight for increased intervention.
On the global stage, Nigerian women continue to shine, with the World Trade Organization (WTO) being led by Dr Ngozi Okonjo-Iweala, the maverick former Nigerian Minister of Finance. The same level of global trust in the Nigerian women’s ability has witnessed the rise of Amina J. Mohammed as Deputy Secretary-General of the United Nations and Chair of the United Nations Sustainable Development Group, whilst in the field of literature Chimamanda Ngozi Adichie continues to keep the world spellbound, engaged and mesmerized.
 As global advocates of women’s rights, health and well-being, the calls for equity and equality in all sectors and especially in the health sector in the face of the COVID-19 pandemic, have risen from murmurs to bellows. Women represent 70 percent of the 43 million workers in the global health care industry yet occupy only 5% of leadership positions. Ninety percent of registered nurses globally are women, women remain the backbone of the informal workforce of unpaid caregivers of sick relatives, community members and children at home. Yet, their immense contribution does not only remain generally unacknowledged, a women’s effort is yet to translate to representation on policy and decision-making tables.
Health is fundamental to national, as well as global security. A gender-balanced health sector leadership in any nation, deliberately ensuring inclusiveness, while eliminating structural inequities, will deliver the population health essential to reaching the national goals of development and progressiveness.
Nigerian women in health have shown great fortitude and stellar results when present in the room. Sign-post examples include women like late Dora Akunyili, whose immense work produced game-changing policies in the Nigerian national drug-supply chain, and the late Dr. Stella Adadevoh, whose foresight changed the trajectory of the Ebola pandemic in Nigeria in 2014, which as the most populous African nation, proved to be an essential pivotal moment in the global threat of Ebola.
On a less national level, Nigerian women are at the fore-front of the health development programs, as they deliver life-saving health implementation activities of malaria prevention, nutrition and, water and sanitation, essentially as house-hold partners and implementers to the national health programs.
In spite of these documented examples from the bottom and the ones at the top, the public health sector leadership in Nigeria is still male-dominated, and far too much work delivered by women is not credited to them; whereas women-driven civil society leadership such as the strong advocacy trajectory of Nigeria's Wellbeing Foundation Africa continue, consistently to deliver frontline impact and women-centred results. The Nigerian health sector stands to benefit from the immense talent and perspectives that a more gender-balanced leadership that an increase in female leadership will bring.
Women in global health Nigeria, a chapter of Women in global Health, was founded in response to this, and its aims to ensure this balance. It connects the work of Nigerian women, from all levels of the life-course to ensure the inclusion of a gender lens in national policy development.
Women in global health Nigeria ensures that more Nigerian women will contribute from the point of view of leadership in the national health discourse, and that Nigerian women in health will receive the commensurate credit for all their contribution to the health sector; by closing the pay-gap for female health workers, and amplifying the essential work that other levels of committed Nigerian women do.
Leadership at the frontline must also cascade to the household where social protection systems and networks that address the risks towards women and provide support for those facing situations of vulnerability or crisis must be strengthened. They play a vital role in protecting women from poverty and insecurity whilst helping them to cope and recover from shocks ultimately leading to the change in a woman's outcomes.
At the forefront of encouraging and inspiring transformative women leadership in all spheres is the African Women Leaders Network. The COVID-19 pandemic and its disproportionate gendered impacts have challenged AWLN to overcome the setbacks in their goal of creating a continent-wide force of women leaders who contribute to Africa's growth, progress and prosperity by advocating on imperative causes such as reproductive health, gender-based violence, the rights of women and gender equality. This can only be achieved by elevating the status of women’s leadership in Africa and passing on the knowledge learnt by these leaders to the next generation.
The assessment of global progress towards achieving gender equality, 25 years after the Beijing Conference on Women, reveals that gains have been slow and uneven and in some cases, significant pushbacks to this agenda persist. The area where most progress has been recorded is in the adoption of laws and policies to advance women’s rights. In this respect, Nigeria’s record aligns with that of most countries.
Nigeria scored highly with respect to having in place legal frameworks that promote, enforce and monitor gender equality, according to UN Women’s Gender-specific SDG indicators (Women Count). However, the greatest hurdle remains insufficient and proper implementation and follow-up.
Nigeria has continued to make gains in women’s active inclusion in social, economic, and political spheres- however more needs to be done.
Recent data from UN Women’s Women Count Data Hub[1] indicate that in Nigeria, there is a 62% literacy rate of girls aged 15 years and above and growing concerns over the school retention and transition rates. With all the gains made, it is crucial that gender-disaggregated data is available so as to enable effective gender programming and budgeting.
In 2020, UN Women spearheaded the ‘Generation Equality’ campaign, a global multi-stakeholder movement rallying civil society, government, activists and private sector to take bold actions as catalysts toward the vision of the Beijing Declaration and Platform for Action - an undisputable blueprint for a gender-equal world cosigned by women across the globe.
Gender equality is the unfinished business of each generation.
A key action of the movement in Nigeria was to facilitate intergenerational exchange between Nigerian women leaders who were present at the Beijing World Conference on Women in 1995 and today’s generation of Nigerian young women. Thanks to the 1995 generation, the Ministry of Women Affairs was born and because of the 2020 generation, women and girls issues continue to be placed at the forefront of Nigeria’s agenda.
This is the generation that tirelessly spotlighted the plight of sexual and gender-based violence in learning institutions and across leading to the declaration of a State of Emergency on GBV. This is the generation that has organised and mobilised civic action on important issues of democracy and governance. In response to the State of Emergency, at least 23 states have now domesticated the Violence Against Person’s Prohibition (VAPP) Act compared to less than 10 in 2018. Already, ahead of the 2023 elections, youth are the highest constituency group already registering to vote and contest. Generation Equality recognizes the important roles of next generations in being changemakers and working together with gender equality advocates in their local communities - in raising awareness on gender equality with the goal of leaving no one behind.
Nigerian young women are the movers and shakers of political and civic leadership, culture and thought as well as entrepreneurship and innovation.
To paraphrase the National Prayer, they are the generation that is ensuring the labours of Nigerian women heroes are not in vain. Concerted efforts must be made to ensure intentional intergenerational exchange to sustain the gains made since the Beijing Platform for Action.
It is time for the nation to embrace a leadership shift, through an enabling environment - from politics to business and society - that opens the space for young and old to have a transformative impact on our ability to make social change happen.
[1] https://data.unwomen.org/country/nigeria
As global advocates of women’s rights, health and well-being, the calls for equity and equality in all sectors and especially in the health sector in the face of the COVID-19 pandemic, have risen from murmurs to bellows. Women represent 70 percent of the 43 million workers in the global health care industry yet occupy only 5% of leadership positions. Ninety percent of registered nurses globally are women, women remain the backbone of the informal workforce of unpaid caregivers of sick relatives, community members and children at home. Yet, their immense contribution does not only remain generally unacknowledged, a women’s effort is yet to translate to representation on policy and decision-making tables.
Health is fundamental to national, as well as global security. A gender-balanced health sector leadership in any nation, deliberately ensuring inclusiveness, while eliminating structural inequities, will deliver the population health essential to reaching the national goals of development and progressiveness.
Nigerian women in health have shown great fortitude and stellar results when present in the room. Sign-post examples include women like late Dora Akunyili, whose immense work produced game-changing policies in the Nigerian national drug-supply chain, and the late Dr. Stella Adadevoh, whose foresight changed the trajectory of the Ebola pandemic in Nigeria in 2014, which as the most populous African nation, proved to be an essential pivotal moment in the global threat of Ebola.
On a less national level, Nigerian women are at the fore-front of the health development programs, as they deliver life-saving health implementation activities of malaria prevention, nutrition and, water and sanitation, essentially as house-hold partners and implementers to the national health programs.
In spite of these documented examples from the bottom and the ones at the top, the public health sector leadership in Nigeria is still male-dominated, and far too much work delivered by women is not credited to them; whereas women-driven civil society leadership such as the strong advocacy trajectory of Nigeria's Wellbeing Foundation Africa continue, consistently to deliver frontline impact and women-centred results. The Nigerian health sector stands to benefit from the immense talent and perspectives that a more gender-balanced leadership that an increase in female leadership will bring.
Women in global health Nigeria, a chapter of Women in global Health, was founded in response to this, and its aims to ensure this balance. It connects the work of Nigerian women, from all levels of the life-course to ensure the inclusion of a gender lens in national policy development.
Women in global health Nigeria ensures that more Nigerian women will contribute from the point of view of leadership in the national health discourse, and that Nigerian women in health will receive the commensurate credit for all their contribution to the health sector; by closing the pay-gap for female health workers, and amplifying the essential work that other levels of committed Nigerian women do.
Leadership at the frontline must also cascade to the household where social protection systems and networks that address the risks towards women and provide support for those facing situations of vulnerability or crisis must be strengthened. They play a vital role in protecting women from poverty and insecurity whilst helping them to cope and recover from shocks ultimately leading to the change in a woman's outcomes.
At the forefront of encouraging and inspiring transformative women leadership in all spheres is the African Women Leaders Network. The COVID-19 pandemic and its disproportionate gendered impacts have challenged AWLN to overcome the setbacks in their goal of creating a continent-wide force of women leaders who contribute to Africa's growth, progress and prosperity by advocating on imperative causes such as reproductive health, gender-based violence, the rights of women and gender equality. This can only be achieved by elevating the status of women’s leadership in Africa and passing on the knowledge learnt by these leaders to the next generation.
The assessment of global progress towards achieving gender equality, 25 years after the Beijing Conference on Women, reveals that gains have been slow and uneven and in some cases, significant pushbacks to this agenda persist. The area where most progress has been recorded is in the adoption of laws and policies to advance women’s rights. In this respect, Nigeria’s record aligns with that of most countries.
Nigeria scored highly with respect to having in place legal frameworks that promote, enforce and monitor gender equality, according to UN Women’s Gender-specific SDG indicators (Women Count). However, the greatest hurdle remains insufficient and proper implementation and follow-up.
Nigeria has continued to make gains in women’s active inclusion in social, economic, and political spheres- however more needs to be done.
Recent data from UN Women’s Women Count Data Hub[1] indicate that in Nigeria, there is a 62% literacy rate of girls aged 15 years and above and growing concerns over the school retention and transition rates. With all the gains made, it is crucial that gender-disaggregated data is available so as to enable effective gender programming and budgeting.
In 2020, UN Women spearheaded the ‘Generation Equality’ campaign, a global multi-stakeholder movement rallying civil society, government, activists and private sector to take bold actions as catalysts toward the vision of the Beijing Declaration and Platform for Action - an undisputable blueprint for a gender-equal world cosigned by women across the globe.
Gender equality is the unfinished business of each generation.
A key action of the movement in Nigeria was to facilitate intergenerational exchange between Nigerian women leaders who were present at the Beijing World Conference on Women in 1995 and today’s generation of Nigerian young women. Thanks to the 1995 generation, the Ministry of Women Affairs was born and because of the 2020 generation, women and girls issues continue to be placed at the forefront of Nigeria’s agenda.
This is the generation that tirelessly spotlighted the plight of sexual and gender-based violence in learning institutions and across leading to the declaration of a State of Emergency on GBV. This is the generation that has organised and mobilised civic action on important issues of democracy and governance. In response to the State of Emergency, at least 23 states have now domesticated the Violence Against Person’s Prohibition (VAPP) Act compared to less than 10 in 2018. Already, ahead of the 2023 elections, youth are the highest constituency group already registering to vote and contest. Generation Equality recognizes the important roles of next generations in being changemakers and working together with gender equality advocates in their local communities - in raising awareness on gender equality with the goal of leaving no one behind.
Nigerian young women are the movers and shakers of political and civic leadership, culture and thought as well as entrepreneurship and innovation.
To paraphrase the National Prayer, they are the generation that is ensuring the labours of Nigerian women heroes are not in vain. Concerted efforts must be made to ensure intentional intergenerational exchange to sustain the gains made since the Beijing Platform for Action.
It is time for the nation to embrace a leadership shift, through an enabling environment - from politics to business and society - that opens the space for young and old to have a transformative impact on our ability to make social change happen.
[1] https://data.unwomen.org/country/nigeria
FROM September 24th, 2021

Building Resilience Through Actionable Hope – To Recover from COVID-19, Rebuild Sustainable Systems, Respond to the Needs of the Planet, Respect the Rights of People, Replenish And Redeem The Promise Of Multilateralism At The Frontline, And At Scale
Download Her Excellency Toyin Saraki Global Office and Philanthropy and The Wellbeing Foundation UNGA76 Advocacy And Activity Statement here:
Keeping A Better World In View
The COVID-19 pandemic has proved to be the most challenging period the world, and the global health and development community has seen since the Second World War. It’s given way to the new disturbing normal – deepening inequalities and vulnerabilities, decimating economies and plunging millions into extreme poverty. Yet we all agree that the world must prioritize a sustainable recovery, rooted in the 2030 Agenda, and supporting countries and communities as we work to rebuild systems shattered by the pandemic. The backdrop to this year’s 76th UN General Assembly, UN Global Compact, and the important Concordia Leadership Council and Concordia Summit is a world that feels fractured — just when we need to come together against the continued ravages of COVID-19, the accelerating climate emergency, unfolding humanitarian disasters, rising inequality, and much more. Fixing it will take bold leadership, brave choices, and sustained commitments. At UNGA, it means bringing together world leaders, civil society champions, young people, global businesses and many others to reinforce and reinvigorate our collective determination to solve our shared problems.Our ongoing project with our global partner, Nutrition International has seen our program implementation model expand to Northern Nigeria where reported health indices represent the lowest and worst levels in the country. The WBFA ‘Scaling up Zinc and LO-ORS to Improve Childhood Diarrhoea Treatment’ programme which commenced in July 2021 in the two highest-burden of diarrheal disease localities, Kano State (the second most populous state in Nigeria after the megacity, Lagos) and Sokoto State - aims to redefine the health system services to sick children via improved availability and uptake of Zinc and low-osmolarity oral rehydration solution (LO-ORS) which are critical in the treatment of childhood diarrhoea. We advocate that Zinc reduces diarrhoea-specific mortality by 23% and LO-ORS decreases this mortality by an additional 84%3. For this reason, the World Health Organization recommends treatment with zinc and LO-ORS for the clinical management of acute diarrhea. Our objectives to improve the provision of appropriate information to caregivers and influencers, develop the capacity of and improve the supportive supervision for health workers, and the states to increase and sustain availability and access to zinc and LO- ORS commodities demonstrates our commitment to improving the survival rates and health outcomes of infants whose future should be protected.
Download Her Excellency Toyin Saraki Global Office and Philanthropy and The Wellbeing Foundation UNGA76 Advocacy And Activity Statement here: Keeping A Better World In View
FROM September 6th, 2021
[embed]https://youtu.be/fN7y4KEglIg[/embed]
Earlier this week I spent precious time #withRefugees at the UNHCR Nigeria supported UNHCR Refugees settlement communities in Ogoja, Cross Rivers State.
My first stop was Adagom where I was cheerfully welcomed by over 67,000 mothers, men and children once forced to flee, now residing in the Refugee Resettlement Community. Followed by an insightful discussion with the Women Leaders of both the refugee and wonderfully kind Adagom host communities. Adagom is a community full of vibrance and resilience but like so many other displaced communities, burdened with a lack of resources and basic provisions in health, education, and access to gainful livelihoods.
[gallery link="none" size="large" ids="1570,1571,1569"]
I am pleased that my Wellbeing Foundation Africa team, National Program Coordinator and Lead WBFA Community Midwife were on hand to deliver food boxes, dignity kits, education learning materials, and undertake our WBFA baseline needs assessment. We demonstrated our flagship MamaCare class, whilst imparting successful breastfeeding practices with the assistance of WBFA manuals and IEC material.
There are more displaced peoples in Nigeria—over two million—than the populations of Equatorial Guinea, Seychelles and Cape Verde, combined. COVID-19 has affected such communities disproportionately, most especially the women and girls therein in need of maternal health support and timely antenatal care. We have to act fast to get these settlement communities back on track and ensure no woman, no expectant mother, no girl child is left behind.
[gallery size="large" ids="1572,1573,1574"]
These numbers within the global 82 million refugees globally often fail to tell the full story of the tragic situation that has befallen so many residing in Nigeria's North East, and Cross River, Benue, Taraba, and Akwa Ibom States.
The scale of this situation in Nigeria will be a tragedy for our people and our economy if we fail to plan, provide and act, for on their behalf. They are our own brothers and sisters for whom we have shared responsibility to support and include in our existing programmes.
That's why I joined hands with UNHCR, UNHCR Nigeria, and UNHCR Private Sector Partnerships who support such vulnerable communities across the continent and the world by protecting and empowering displace men, women, and youth and to promote social inclusion and foster good relationships with their local communities.
The time is now to convene and inspire others towards action. I echo the words of the UN High Commissioner For Refugees that “solutions require global leaders and those with influence to put aside their differences, end an egoistic approach to politics, and instead focus on preventing and solving conflict and ensuring respect for human rights".The biggest achievement derived from the 1951 Geneva Convention itself, is that many of the challenges faced by IDP and Refugees are now categorised as international problems. In the same vein, individuals must remain exactly that - individuals; affording them a truly localised and personal approach to reintegration and community-level support.
In doing so, we manage traumas correctly, minimise further displacement and ensure that all policies and societal practices reflect each citizen - by birth, heritage or displacement - right up until the last mile.
I am encouraged by the learnings that private sector philanthropies and civil society can contribute in this journey, through collaborative efforts, to rethink and re-imagine the possibilities of donorship and of timely life-saving interventions for the millions of refugees and we must remember: no one is truly safe until everyone is safe.
I am pleased to join UNHCR, partnering to ensure all refugees and displaced people have access to their basic human rights and dignities.

FROM August 13th, 2021
This is a moment for heightened urgency in addressing the investments and attention being paid to our public health systems in Nigeria, as globally. Deep inequities and unbalanced approaches to channelling much needed remuneration, respect and investments to prioritise our frontline force have been exaggerated since the onset of the Pandemic. The unnerving, recent announcement by Nigeria’s National Association of Resident Doctors public strike is the fourth work stoppage by medical residents since the pandemic began. As the backbone of our public health - health and care workers and CHWs have provided essential health services to communities with the least access to quality care, especially in remote and rural areas- accelerating the attainment of universal health coverage - despite inadequate attention being applied to facilitating decent work, safety, dignity, fair pay and equal leadership they deserve - as the key mutual and multi-directional duty of care. I remain deeply concerned especially that the state of primary healthcare centres across Nigeria, and how the frontline potential for PHC's being the first port of call for serious injury and disease, a barrier between life and death for many - is being underutilized. For years, Nigeria, like many other lower-middle income countries, has struggled to address health worker shortage lagging far behind the WHO suggested doctor-patient ratio of 1:600. With the 19,000 protesting medical residents making up the bulk of health care workers at government hospitals throughout Nigeria, also staffing the majority of the government-run treatment facilities for COVID-19 - their absence at this crucial time is an alarming concern. This is a period that calls for whole system support as a duty of care - and a greater push for resources, resilience, replenishment towards recommended ratios which of course integrates regular remunerations. Taking learnings from paradigm shifts recorded in countries such as India, whose medical education system has been able to pull through a major turnaround, successfully doubling the numbers of MBBS graduate (modern medicine training) positions during recent decades - it is not enough to fixate on the excuse of doctor scarcity. As we move forward there is an urgent need to focus on augmenting the fiscal capacity as well as developing much needed infrastructure both in public and private health sectors toward addressing pressing healthcare needs of our growing population.
FROM June 23rd, 2021
COVID-19 has enabled global citizens to hold a greater understanding of the integral role WASH plays in public health, and our lives at large. It has caused policymakers, advocates and donor to review a culture that previously undermined the relationship we all had with WASH and disease prevalence. The current data sadly shows that Nigeria carries over 20% of our African continent’s NTD burden.
FROM June 10th, 2021
 Bearing the regal approval and presence of His Royal Majesty, Oba (Dr.) Abdulfatah Aremu Oyeyinka Aromire, Oyegbemi II, The Ojora of Ijora Kingdom and Iganmu Lands, I appreciate the honour bestowed upon me by His Royal Majesty, Oba Abdulwasiu Omogbolahan Lawal, Abisogun II, The Oniru of Iru Land, who conferred my humble self with the recognition of being appointed and installed as the Erelu Bobajiro of Iru Land on 10th June, 2021, during the week long 1st Year Coronation Anniversary Celebration of His Royal Majesty Abisogun II, Oniru of Iru Land.
I congratulate Kabiyesi Oba Omogbolahan Lawal on the first anniversary of his coronation, and all chieftaincy honorees dedicated to the visionary mission to bring meaningful progress and development to Iru Land, supported by the Iru Land Oba-In-Council Cabinet of Chiefs.
I am grateful for the inestimable love and support of my Royal Father, The Ojora of Ijora Kingdom and Iganmu Lands, Kabiyesi, His Royal Majesty, Oba (Dr) Abdulfatah Aremu Oyeyinka Aromire, Oyegbemi II, His Council of Chiefs, and the good people of the Ijora Kingdom and Iganmu Lands for honoring my homecoming to Ijora Oloye with the highest privilege of Apesin Ceremonial Procession. I equally congratulate His Royal Majesty, Oba (Dr) Abdulfatah Aromire, Oyegbemi II, Apasa Kekeniju, on the 27th Anniversary of his purposeful and successful continued reign as The Ojora of Ijora Kingdom and Iganmu Lands.
I am appreciative of the amity, kinship and prayers bestowed towards me by Royal Stools and Royal Families across the length and breadth of Nigeria and beyond, most notably and especially, the gracious presence of Their Royal Majesties, The Amanyanabo Ebitimi Banigo, King of Okpoama Kingdom, Brass, Bayelsa State, his lovely Queen Pelebo Banigo, and their Royal Cabinet. I also appreciate the presence of The Erelu Kuti IV, HRH Princess Abiola Dosunmu, and the attendance of the Ilorin Emirate Princes, personally and as the delegated envoys of His Royal Majesty, The Emir of Ilorin, Mai Martaba, Dr. Ibrahim Sulu Gambari CFR.
I recognize and appreciate the presence and attendance of Their Excellencies, Former Governors, Senator Liyel Imoke of Cross River State, Dr Abdulfatah Ahmed of Kwara State, Alhaji Shaba Lafiaji of Kwara State, Chief Olusegun Osoba and Beere 'Derin Osoba of Ogun State, Alhaji Ibrahim Hassan Dankwambo of Gombe State, current and former Distinguished Senators, Honorable Members of the House of Representatives and State House of Assembly, current and former Honorable Ministers, current and former States Commissioners and Local Government Functionaries, national and states political parties functionaries and members, and the supportive presence of women and youth leaders, groups, cooperatives and associations.
I am forever thankful for the unflinching and loving support and encouragement of my dear husband, His Excellency, Dr Abubakar Bukola Saraki, MBBS, CON, The Waziri Ngeri of Ilorin Emirate,13th President of the Senate and Chair, 8th Session of the National Assembly 2015~2019, together with the blessings of my lovingly respected parents, Their Royal Highnesses, The Otunba Adekunle Ojora OFR, CON, and The Erelu Odu’a Ojuolape Ojora, MON. I appreciate too, the personal visit, recognition and kinship of His Imperial Majesty, Alaiyeluwa, Arole Oodua, Olofin Adimula,The Ooni of Ife, Dr. Adeyeye Enitan Babatunde Ogunwusi, Ojaja II.
With utmost respect and gratitude, I appreciate the attendance of my personal friends, international development and private sector partners, my immediate and extended family, and the good citizens of both Lagos and Kwara States. who honoured me with the joy and privilege of their distinguished presence at the Traditional Iwuye Ceremony at The Oniru’s Palace, Iru Land, and the Ijora Oloye Homecoming Apesin Procession at The Ojora of Ijora Palace, Ijora Kingdom.
I pray for the light of knowledge, wisdom and peace for all, and journey mercies to our respective homes. Amen.
Bearing the regal approval and presence of His Royal Majesty, Oba (Dr.) Abdulfatah Aremu Oyeyinka Aromire, Oyegbemi II, The Ojora of Ijora Kingdom and Iganmu Lands, I appreciate the honour bestowed upon me by His Royal Majesty, Oba Abdulwasiu Omogbolahan Lawal, Abisogun II, The Oniru of Iru Land, who conferred my humble self with the recognition of being appointed and installed as the Erelu Bobajiro of Iru Land on 10th June, 2021, during the week long 1st Year Coronation Anniversary Celebration of His Royal Majesty Abisogun II, Oniru of Iru Land.
I congratulate Kabiyesi Oba Omogbolahan Lawal on the first anniversary of his coronation, and all chieftaincy honorees dedicated to the visionary mission to bring meaningful progress and development to Iru Land, supported by the Iru Land Oba-In-Council Cabinet of Chiefs.
I am grateful for the inestimable love and support of my Royal Father, The Ojora of Ijora Kingdom and Iganmu Lands, Kabiyesi, His Royal Majesty, Oba (Dr) Abdulfatah Aremu Oyeyinka Aromire, Oyegbemi II, His Council of Chiefs, and the good people of the Ijora Kingdom and Iganmu Lands for honoring my homecoming to Ijora Oloye with the highest privilege of Apesin Ceremonial Procession. I equally congratulate His Royal Majesty, Oba (Dr) Abdulfatah Aromire, Oyegbemi II, Apasa Kekeniju, on the 27th Anniversary of his purposeful and successful continued reign as The Ojora of Ijora Kingdom and Iganmu Lands.
I am appreciative of the amity, kinship and prayers bestowed towards me by Royal Stools and Royal Families across the length and breadth of Nigeria and beyond, most notably and especially, the gracious presence of Their Royal Majesties, The Amanyanabo Ebitimi Banigo, King of Okpoama Kingdom, Brass, Bayelsa State, his lovely Queen Pelebo Banigo, and their Royal Cabinet. I also appreciate the presence of The Erelu Kuti IV, HRH Princess Abiola Dosunmu, and the attendance of the Ilorin Emirate Princes, personally and as the delegated envoys of His Royal Majesty, The Emir of Ilorin, Mai Martaba, Dr. Ibrahim Sulu Gambari CFR.
I recognize and appreciate the presence and attendance of Their Excellencies, Former Governors, Senator Liyel Imoke of Cross River State, Dr Abdulfatah Ahmed of Kwara State, Alhaji Shaba Lafiaji of Kwara State, Chief Olusegun Osoba and Beere 'Derin Osoba of Ogun State, Alhaji Ibrahim Hassan Dankwambo of Gombe State, current and former Distinguished Senators, Honorable Members of the House of Representatives and State House of Assembly, current and former Honorable Ministers, current and former States Commissioners and Local Government Functionaries, national and states political parties functionaries and members, and the supportive presence of women and youth leaders, groups, cooperatives and associations.
I am forever thankful for the unflinching and loving support and encouragement of my dear husband, His Excellency, Dr Abubakar Bukola Saraki, MBBS, CON, The Waziri Ngeri of Ilorin Emirate,13th President of the Senate and Chair, 8th Session of the National Assembly 2015~2019, together with the blessings of my lovingly respected parents, Their Royal Highnesses, The Otunba Adekunle Ojora OFR, CON, and The Erelu Odu’a Ojuolape Ojora, MON. I appreciate too, the personal visit, recognition and kinship of His Imperial Majesty, Alaiyeluwa, Arole Oodua, Olofin Adimula,The Ooni of Ife, Dr. Adeyeye Enitan Babatunde Ogunwusi, Ojaja II.
With utmost respect and gratitude, I appreciate the attendance of my personal friends, international development and private sector partners, my immediate and extended family, and the good citizens of both Lagos and Kwara States. who honoured me with the joy and privilege of their distinguished presence at the Traditional Iwuye Ceremony at The Oniru’s Palace, Iru Land, and the Ijora Oloye Homecoming Apesin Procession at The Ojora of Ijora Palace, Ijora Kingdom.
I pray for the light of knowledge, wisdom and peace for all, and journey mercies to our respective homes. Amen.
FROM May 31st, 2021
[embed]https://www.youtube.com/watch?v=aK6FtsOnKJw[/embed] I am delighted to join our partners, the Liverpool of Tropical Medicine, Johnson and Johnson Global Health, the Kwara State Government and all stakeholders today as we disseminate the results and impact of our 5-year program to improve the availability and quality of maternal newborn care services delivered by health workers in Kwara State. From the first moment I witnessed the impact of hands-on anatomically delivered simulation model training globally, I knew that building a community of well-practiced multi-disciplinary delivery teams could address the local frontline barriers to improving care services rapidly and whole-heartedly, at both the health system and societal level, in Nigeria. Thus, in 2015, my WBFA leapt at the golden opportunity to partner together with the Liverpool School of Tropical Medicine, CMNH-LSTM Nigeria and Johnson and Johnson Global Health to up-skill health care practitioners in the area of certificated Emergency Obstetric Care Skills and Drills. The main drive of the project pioneered across Kwara State, Nigeria, was to equip doctors, nurses and midwives so as to recalibrate a collective team and introduce the skills needed to overcome these obstetric emergencies. With hopes to improve maternal health significantly, we have continued to identify and lift away the barriers that limit access, availability and quality of maternal and newborn health services. 80% of all maternal deaths are as a result of five complications; all of which can- be managed by adequately trained healthcare professionals. Haemorrhages, sepsis, eclampsia, complications of abortion and obstructed labour are among the common attributional factors of maternal and neonatal complications, but they also contribute to mortality and morbidity, too. The introduction of specialist professional and regular training acts presents as a form of diligence while reinvigorating frontline workforce autonomy. As we focused our intervention on local government areas within the state with the largest population of women of reproductive age, we landed in Kwara located in north-central Nigeria, It’s 3 million inhabitants and an estimated 120,000 births per year, coupled with my own personal state-centred nostalgia and birth experience, made it the perfect beginning for such a dissemination of key skills and learning. Through a partnership with the Liverpool School of Tropical Medicine and with support from Johnson and Johnson Corporate Citizenship Trust, Wellbeing Foundation Africa implemented a project to increase the availability and quality of care for mothers and babies at public and private healthcare facilities in Kwara State, Nigeria. Having sustained the early and encouraging impact being made by the introduction of EmONC skills and drills training, and expanding the program in 2018, we continued by paying joint advocacy visits to the Kwara State House of Assembly to advocate at the sub-national level for the training espoused by our EmONC program which was pioneering sustainable change across 21 public HCFs in the state. I hope that our strong evidence now demonstrates that anatomical models based skills and drills training must be recognised as a professional education curriculum requirement, and fast. As we conclude the 5th year of this pioneering introduction in Kwara State, we now have convincing proof of a concept beyond suitable for whole nation deployment. The results are clear, we’ve recorded a 38% reduction in facility stillbirth rate since 2015, and we know that the improvements and upskilling in Kwara can, must and will inspire change across the country. I thank our partners, the Liverpool School of Tropical Medicine’s Centre For Maternal and Newborn Health, and Johnson and Johnson Global Health, for the trust and confidence invested in the Wellbeing Foundation Africa and United Nations Every Woman Every Child Commitments to the Global Strategy on Women and Childrens’ Health, which powered our partnership, and their arrival to Nigeria to implement such a significant program. I beam with pride and with a grateful heart at the readiness demonstrated by a robust frontline, and look forward to the actualisation of a continuum of care that will contribute to the total zeroing of maternal and neonatal deaths in Nigeria. It is often said that the true test of innovation and impact is sustainable local engagement, so I am delighted that the partnership was able to establish skills laboratories and centres of excellence at selected facilities. I congratulate our partners and the National Council of Nursing and Midwifery as the program impact progresses, again supported by Johnson and Johnson Global Health, on the strategic and intentional path towards national pre-service training scale. Towards holistically aligning and guaranteeing mothers access to higher quality respectful maternity care, the Wellbeing Foundation Africa continues to strengthen, deepen and widen its independent community midwifery-led Mamacare Antenatal and Postnatal Education Program, educating expectant and nursing mothers, ensuring they access and achieve the WHO recommended 8-visits throughout their childbirth journey - with the confidence of knowing that their professionally qualified delivery attendants are upskilled to deliver a safe, healthy and therefore happy outcome. We must continue on the quest to lift and leap over barriers, to deliver new life safely, and ultimately save millions more lives. Thank you all. [embed]https://www.youtube.com/watch?v=bhMUE5VZMZc[/embed]
FROM May 5th, 2021

FROM April 19th, 2021
I am delighted to welcome and participate in the first day of the Institutionalising Community Health Conference , which focuses on Accelerating PHC at the Community Level. For many years, I successfully led Nigeria’s CSO PHC Revitalization Support Group which advocated successfully for Nigeria's redemption of the Abuja Declaration Pledge of 1% Consolidated Revenue Fund to Health. The 2018 Basic Healthcare Provision Fund BHCPF HUWE, Comprehensive Community Healthcare has remained a core target of my Wellbeing Foundation Africa's mission, vision and actions ever since. By addressing the wider factors that may delay or hinder the holistic delivery of Community Health Management and Quality, enables us to place a strategic lens on how optimal health outcomes, and increased equitable access to care can, and should remain a priority. Globally, when we demonstrate an intentional, collective and results-based commitment to the facilitation of Universal Health Coverage and a quantifiable delivery of a Continuity of Care, we are able to actualise equal access to health care, move into promoting a truly universal and affordable healthcare system, and most importantly, place quality at the heart of community care - for any and all. It is important to galvanise funding and action in order to strengthen primary care access and in order to keep essential public health services functioning. How do we succeed in doing so? By ensuring that the primary conversations held ahead of any disbursement, allocation, policy creation or protocol implementation is being had with the most remote and vulnerable people in mind - and within view. This is how we collectively maintain our social and civic responsibility, as well as keeping the integrated health services of every community alive. Multi-sectoral policy and action must reflect and empower the very people and communities it is formed to serve, and the health and wellbeing of said individuals is the effective and most precedential place to begin - and continue. For me, strengthening localised approaches to UHC, means we can successfully begin the transition into delivering community health coverage (CHC) - a journey where the task and charge is to minimise discrimination, strengthen and revive strained approaches to cultural sensitivity, and straighten the pathway to putting the ‘U’ in universalism. We must increase targeted and inclusive investments and make the road to care more generally accessible - starting with Maternal and neonatal health. When we recognise the importance of EmONC training, facilitation and care - including displaced persons and refugees - we make the case for equitable access even stronger. Factors such as malnutrition, language barriers, no fixed address and underlying health / obstetric conditions place these women and neonates within a higher risk category and makes them more prone to complications; preconception, antenatally, intrapartum and postnatally. What then is the purpose of Institutionalizing Community Health? A revival; a call to action that requires true, palpable and equitable action to take place.
FROM April 9th, 2021
It is time to build a fairer, healthier world. It is time to build back better If the global COVID-19 pandemic has taught us anything, it is that our basic human rights and access to decent health and care is far from being a lived reality for millions of people around the world. Timely, optimal and affordable healthcare which is facilitated to an appropriate quality and standard, is often a dream for the 1.8 billion men, women and children who face appalling conditions inside hospitals and local health clinics. The problems they often face? A lack of Water, Sanitation and Hygiene (WASH) among others. Today, 50% of healthcare facilities in Least Developed Countries lack even basic water services - a resource and a solution in tandem, that if provided, would both cure and prevent a number of complications, illnesses and deaths. We cannot actualise health equity if we do not consider and prioritise the role and place of adequate WASH across any and all facilities. In 2019, my Wellbeing Foundation Africa committed to training 500 healthcare workers and educating 35,000 pregnant and nursing mothers across Nigeria on hand and personal hygiene practices by 2020. We also committed to advocating for improved WASH structures in healthcare facilities in 2019 and 2020 to enable healthcare workers in Nigeria to perform their duties effectively - a timely initiative which I firmly believe ingrained the practice’s importance in the hearts of Nigeria’s women and families just in time for the pandemic. We are proud to be part of the 100 global commitments to WASH in Healthcare Facilities made over the last 3 years, driving a rally cry to transform this "neglected crisis" within global health into a global health movement with Global Water 2020 and Global Health Council. In the words of Dr. Maria Neira, Director of Public Health and Environment at the World Health Organization, "a healthcare facility without WASH is not a healthcare facility." I join UN Secretary General Guterres, WHO Director-General Dr. Tedros, UNICEF Executive Director Fore, heads of state and First Ladies, Ministers of Health, Vatican officials, the Dalai Lama and so many more in a global call for funding, technical assistance, research, training, maintenance and advocacy. WASH is an essential service and progress to get it into healthcare facilities will be among the most critical global health advances we can make in our journey to equal health for all. Crowning the 2021 World Health Care Worker Week by lending my solidarity and by commending, honouring and celebrating our global frontline, who championed the importance of WASH through aseptic techniques when facilitating care, by committing to WASH long before the global pandemic, thoroughly during the height of the waves, and hopefully so, going forward. Thank you. #WorldHealthDay # WASHinHCF #WASHWednesday
FROM April 1st, 2021
I’m delighted to join WHO in welcoming its 2021-2030 Neglected Tropical Diseases Roadmap, and anticipate the emergence of the renewed Global Strategy for Water, Sanitation and Hygiene. Ending the neglect to attain the Sustainable Development Goals: a road map for neglected tropical diseases 2021−2030 was prepared through an extensive global consultation pursuant to decision EB146(9) of the Executive Board at its 146th session in February 2020 that culminated in the endorsement of the document by the Seventy-third World Health Assembly in November 2020. The road map sets global targets and milestones to prevent, control, eliminate or eradicate 20 diseases and disease groups as well as cross-cutting targets aligned with the Sustainable Development Goals. Three foundational pillars will support global efforts to achieve the targets: accelerate programmatic action (pillar 1), intensify cross-cutting approaches (pillar 2) and change operating models and culture to facilitate country ownership (pillar 3). The disease summaries annexed to the road map detail the current epidemiological status and burden of disease, core strategic interventions and progress towards the 2020 targets of the previous road map. The targets, sub-targets and milestones for 2030, and the critical actions required to achieve them, were used to generate the evidence in the road map document endorsed by the World Health Assembly. My Wellbeing Foundation Africa serves as an example of the powerful role that community facilitation of WASH plays in successfully inhibiting all 20 NTDs; from outright prevention and effective treatment, to reducing the prevalence of many more by between 33 to 70 percent (including intestinal worms which half a billion school children are at risk of.) Ensuring that access to WASH is made truly equitable remains an ongoing priority - the global strides taken to end all of the 20 NTDs mentioned within the roadmap will accelerate this much needed equity. As we continue to underpin WASH in every Covid-19 response worldwide, we further strengthen and reiterate its importance, and in so doing, place greater value on water as a resource greatly required by every girl, boy, woman, man and child. We must embrace a multilateral approach across a plethora of sectors, and join WHO in reiterating the importance of increased and targeted investments and global awareness raising strategies that highlight the reach and impact of collective action now.
FROM March 24th, 2021
Every day, nearly 4000 people lose their lives around the world to Tuberculosis. That’s over 160 people an hour and at least 2 people every minute.
The clock is ticking and the priority remains to accelerate preventative action globally, to address health risks and social determinants of the disease nationally, and to further promote access to #UHC at the subnational and local levels to end TB.
According to the World Health Organisation's 2020 Global TB Report, in 2019, 440,000 people fell ill with TB in Nigeria and 155,000 avoidable death certificates were attributed to this deadly disease. As at 2019, TB treatment coverage stood at 27% - a far cry from the 2025 target of 90% operational target to end TB; although promising, the treatment success rate was 87%.
People can and do recover - but, we must do more and do better to detect, prevent, treat and support our communities.
My Wellbeing Foundation Africa team works daily to improve RMNCAH+N - alongside prevention, detection, treatment, and support which provides the pathway to achieving the vision of ending Tuberculosis by the year 2030. Last year, through collaborating with Nigeria's National Tuberculosis and Leprosy Control Program (NTBLCP), we visited health facilities and communities in the FCT and Nassarawa state, to health and care workers at the front of the frontline fight against the disease.
During a lecture regarding the spread of TB in Nigeria led by our WBFA Abuja Mission Lead Dr Otun Adewale, Dr. Ogedengbe Babatunde, Provost Divine Jubilation College of Health Technology for Masaka, Nasarawa State shared, “it is sad to learn that Nigeria is being hit the worst in Africa and 5th in the world when it comes to TB. It’s even harder to hear that the largest impact is attributed to children, women of reproductive age and people living with HIV.”
[caption id="attachment_1516" align="alignnone" width="1024"] Dr. Ogedengbe Babatunde, Nassarawa State[/caption]
His conclusions further emphasise the need for targeted educational efforts, and empowerment of people - before they become patients.
I commend every effort made by my own foundation’s frontline staff, and our global health heroes, and will continue to call for whole-system support for professionals and patients alike. We must continue to focus our progress in the direction of uplifting frontline morale, devising authentic and targeted approaches taken to maintaining their own health and wellbeing at the most localised level. We can do this by ensuring that equipment and PPE are made available and investments and donations are made in the direction of training and continued up-skilling.
A further and key component in addition to increased donorship is that the actualisation of Universal Health coverage and health security are closely interlinked. Dr Tedros Adhanom Ghebreyesus, Director-General of the WHO, refers to Universal Health Coverage as a “political choice, and that it is the responsibility of every country and national government to pursue it.” In Nigeria and in many other countries, he is also right to point out that health security and universal health coverage are closely interlinked.
Public campaigns and mobilisation must seek to educate all individuals and raise awareness, so that early detection and prevention are possible. While resources may be scarce, innovative and strategic management is key to overcome structural hurdles.
These are the practical steps we can take as the clock turns. Together, and even in the mammoth shadow of the Covid-19 pandemic, we can achieve zero TB-related deaths and save lives, before the clock runs out.
Wishing you a targeted and more progressive #WorldTBDay.
Dr. Ogedengbe Babatunde, Nassarawa State[/caption]
His conclusions further emphasise the need for targeted educational efforts, and empowerment of people - before they become patients.
I commend every effort made by my own foundation’s frontline staff, and our global health heroes, and will continue to call for whole-system support for professionals and patients alike. We must continue to focus our progress in the direction of uplifting frontline morale, devising authentic and targeted approaches taken to maintaining their own health and wellbeing at the most localised level. We can do this by ensuring that equipment and PPE are made available and investments and donations are made in the direction of training and continued up-skilling.
A further and key component in addition to increased donorship is that the actualisation of Universal Health coverage and health security are closely interlinked. Dr Tedros Adhanom Ghebreyesus, Director-General of the WHO, refers to Universal Health Coverage as a “political choice, and that it is the responsibility of every country and national government to pursue it.” In Nigeria and in many other countries, he is also right to point out that health security and universal health coverage are closely interlinked.
Public campaigns and mobilisation must seek to educate all individuals and raise awareness, so that early detection and prevention are possible. While resources may be scarce, innovative and strategic management is key to overcome structural hurdles.
These are the practical steps we can take as the clock turns. Together, and even in the mammoth shadow of the Covid-19 pandemic, we can achieve zero TB-related deaths and save lives, before the clock runs out.
Wishing you a targeted and more progressive #WorldTBDay.
FROM March 20th, 2021
I am both horrified and saddened by the atrocities and breaches of human rights reported as presently occurring in the Ethiopian province of Tigray.
Following many years of the country’s collaborative attempts to recalibrate societal attitudes and behaviours, by promoting unity and tolerance for all persons, we are today, met with the devastating news and evidence of inexplicable acts of harm and violence towards women and girls.
War is the destructive debasing of a united people - but to then fall victim to rape is a devastating low of sexual violence in conflict, in a war which unfairly divides and deprives humanity of dignity and autonomy.
Cowardly and inhumane crimes such as these must be dealt with and stamped out, fast - and appropriately.
I am urging for government and policymakers, people of power and community members to speak up for the application of United Nations Resolution 1325 on women, peace and security, and the prevention of sexual violence in conflict. Perpetrators should be identified and reprimanded swiftly and appropriately.
FROM March 8th, 2021
FROM March 7th, 2021

FROM January 30th, 2021
This World NTD Day, the Neglected Tropical Disease (NTD) community is further shining a light on the critical role that access to clean water and sanitation plays in the prevention of these illnesses. The just-launched World Health Organization (WHO) NTD road map is a clear indication that tides and times are changing, with a much needed focus being placed on the need for increased incorporation of water, sanitation and hygiene (WASH). According to the CDC, 100 percent of low-income countries are simultaneously affected by at least five of the 20 parasitic, bacterial, viral and protozoan infections grouped together as NTDs, and 149 countries and territories are affected by at least one NTD. 1.7 billion people worldwide live with these diseases that deform bodies, blind and kill, disrupt children’s education, limit lifetime productivity; and ultimately traps families and communities in cycles of poverty that contribute to crippling economies. My Wellbeing Foundation Africa serves as an example of the powerful role that the facilitation of WASH plays in successfully inhibiting all 20 NTDs; from outright prevention and effective treatment, to reducing prevalence of many more by between 33 to 70 percent (including intestinal worms which half a billion school children are at risk of.) Except... three billion people do not have access to water in their home. 900 million children go to schools without accessible handwashing facilities, and in the battlegrounds of disease itself, nearly 2 billion patients and healthcare staff must rely on healthcare facilities without water where care is provided. Sadly, access to WASH is that neglected. I believe and continue to demonstrate that the solution for combatting NTD’s starts and ends with WASH – a message that the onset of the global pandemic successfully communicated to members of the NTD community. The global health focus must continue to shift from solely reflecting treatment as the primary solution, and embrace the power of prevention through WASH. The Covid-19 pandemic has caused policymakers, global health advocates and donors to step away from a culture that previously undermined the relationship between WASH and disease prevalence. For a fifth year in a row, last year one billion people were treated for NTDs. While this is extraordinary outreach, it begs us to question how much of that suffering could have been prevented all together if children weren’t drinking intestinal worm-laden water and women weren’t irreversibly blinded at four times the rate of men by flies thriving in open waste? Despite excellent work being done to bring needed attention to these 20 diseases that attack the most vulnerable, and the efforts to get medications to them, the economic toll remains high and the human suffering remains devastating. This is no small problem and my country, Nigeria, is a case in point. According to WaterAid, 95 percent of healthcare centers in Nigeria are without basic WASH provisions, as well as 79 percent of all households. It is both alarming, and no surprise, that in a country where the majority of its citizens lack WASH and ranks first among nations in open defecation, half of its population—an estimated 100 million people—are at risk for at least one NTD. Nigeria carries 25 percent of Africa’s entire NTD burden. In 2013, the Federal Ministry of Health sought to reduce NTD morbidity and mortality, including by scaling-up WASH and other interventions—a step in the right direction. Guinea worm has been eliminated in Nigeria with a dramatic decline in three other NTDs (lymphatic filariasis, onchocerciasis, and trachoma which causes irreversible blindness). But Nigerians are far from NTD-free and even farther from having the water and sanitation they deserve. One of the goals of my organization, The Wellbeing Foundation Africa (WBFA), is to improve health outcomes for women, children, and infants. We are committed to improving and increasing access to WASH in healthcare facilities, schools and communities across Nigeria, in a bid to reduce and eventually eradicate the prevalence of NTDs. WBFA’s team of midwives, in partnership with Unilever Lifebuoy Nigeria and Sightsavers, have reached more than two million children at-risk of NTDs, all while improving the education and hygiene practices. These school-based efforts reinforced in children, their families and communities the importance of prioritising WASH interventions, including handwashing with soap. The new WHO NTD road map is a much welcomed northern star. For the first time, there is a global target for WASH that countries must meet over the next 10 years – a solidified set of directions that will mark long-term change at each juncture. A companion strategy on integrating WASH will follow later this spring and making way for new collaboration calls for investments, programming and policies to assure universal and sustainable WASH coverage in NTD endemic areas, otherwise, we risk losing the gains made in reducing NTDs over this past decade and into the future. COVID-19 has ushered in greater understanding of the integral role WASH plays in public health. It is fair to say, that unacceptable WASH conditions not only fan the flames of COVID-19 where people cannot adequately wash their hands, they contribute to many less infamous but pervasive diseases that cause great harm, like, NTDs. At a time when the world is focused on global health, the NTD community is offering important leadership that I hope will encourage many other global health efforts to stop neglecting what is the singular foundation upon which to build better health. About the Author: Her Excellency Mrs. Toyin Saraki is Founder/President of the Wellbeing Foundation Africa (WBFA). She is a former regional First Lady and Nigerian philanthropist who has spent two decades as a global advocate on behalf of women. She is a former two-term Global Goodwill Ambassador for the International Confederation of Midwives and a Special Advisor to the Independent Advisory Group of the WHO’s Regional Office for Africa. @ToyinSaraki
FROM January 29th, 2021
Reflecting on the challenge of reinforcing and replenishing community-centred care during covid-19.
FROM December 31st, 2020
We acknowledge and appreciate the support of all respected and esteemed friends and associates from all walks of life, including many others that we may have forgotten to mention.
Perhaps you sent a lovely card, or sat quietly in a chair, perhaps you sent beautiful flowers. If so, we saw them there. Perhaps you sent or spoke kind words and prayers, as any friend could say; perhaps you were not there at all, just thought of us that day. Whatever you did to console the heart, we thank you so much, whatever the part.
Your kindness provided a soothing balm to the tragedy that Prince Adedapo’s sudden departure represents to us. Adedapo was our warrior Prince, our symbol of courage, bravery, valour and peace, who has gone to meet our ancestors.
It is within our sober knowledge and wisdom that in every sunshine, a little rain must fall. We thank you for standing by us in our time of sorrow and we pray that Almighty God will continue to bless you all.
Respectfully, and with grateful appreciation,
Adeyinka Adekunle Ojora and Toyin Ojora Saraki
On behalf of the Ojora Royal Family of Lagos.
FROM December 12th, 2020
The Ojora Family of Lagos sadly regrets to inform of the death of our dearly beloved son, brother, uncle and father, Omo-Oba Adedapo Adelanke Abdulfatah Ojora on Friday 11th December, at his Ikoyi, Lagos residence.
We are grateful to the Lagos State Police Command for immediately commencing an investigation into the circumstances of his death - the outcome of which we await.
As we mourn our irreparable and devastating loss, we appreciate the condolence messages and prayers that we have received, and seek your understanding that the family be allowed to grieve in private. Funeral arrangements will be announced in due course.
We ask that you continue to pray for the repose of Adedapo's soul. Amen.
FROM December 10th, 2020
It’s time to put the ‘move’ in movement; assessing the Role of Nigeria’s Multi-Disciplinary Health Response in Identifying, Establishing & Delivering Interventions in Cases of Violence Against Women and Girls (VAWG) On Thursday December 10th the Wellbeing Foundation Africa (WBFA) held its innovative #EndViolence Webinar. The well attended and highly discursive event was the culmination of the United Nations (UN) 16 days of activism against Gender Based Violence (GBV) which took place from November 25th to December 10th. The Wellbeing Foundation Africa’s commitment to ending gender-based violence and harmful practices as per the SDG’s three zeroes, extends beyond childbearing women at health facilities, and daily transcends into teaching our Adolescent Skills and Drills PSHE curriculum in schools across Nigeria. Our commitment here is to teaching adolescents what is deemed a healthy relationship and how to spot and respond to abuse including child marriages in a safe and trusted authentic space. Our health workers also seek to provide adolescents with personal social and health education on sexual and reproductive health and rights. The webinar brought together healthcare practitioners, midwives, policymakers, WBFA staff and those in the field of broadcast media/journalism with the objective of introducing them to WBFA’s newly developed protocol for recognising, referring and aiding victims of violence against women and girls whilst also identifying areas of co-operation to combat the growing cases of GBV in Nigeria. Speakers on the day parted with a multitude of knowledge, expertise and experiences which included the keynote address by the Founder-President of the Wellbeing Foundation HE Toyin Saraki, Dr Otun Adewale Olalekun, Abuja state team lead, WBFA, Dr Muna Abudullah, Health System Specialist at the United Nations Population Fund (UNFPA), Fati Abubakar a renowned photojournalist from Maiduguri, Borno State and Aisha Salaudeen, a multimedia journalist with CNN International. Throughout all our work, the Wellbeing Foundation Africa promotes and achieves the WHO’s recommendations on how countries can improve quality of care in their health facilities and prevent maternal and newborn deaths, based on its standards for improving quality of maternal and newborn care in health facilities, and even before a woman with child arrives - as our accountability policy and targets - and we deliver this through our investment in community midwifery, localising care: 1) Pregnant women should receive the right care, at the right times 2) Newborns should receive essential care immediately after birth 3) Small and sick babies should be well cared for in a facility 4) All women and newborns must receive care that prevents hospital-acquired infections 5) Health facilities must have an appropriate physical environment 6) Communication with women and their families must be effective and respond to their needs 7) Women and newborns who need referrals can obtain them without delay 8) No woman should be subjected to harmful practices during labour, childbirth, and the early postnatal period 9) Health facilities need well-trained and motivated staff consistently available to provide care- 10) Every woman and newborn should have a complete, accurate, and standardized medical record. Addressing the silent pandemic of violence against women and girls (VAWG) is one of the cardinal focal points of WBFA’s engagement and policy strategy. According to UN Women, one in three women worldwide experience physical or sexual violence mostly by an intimate partner. Further studies estimate that in Africa, between 23 to 49% of pregnant women experience physical, sexual and emotional violence from an intimate partner during their pregnancy. There has been an increase in reports of gender based violence cases in all six geopolitical zones in Nigeria since the pandemic began but a lack of systematic data collection and a political/cultural system that favours the accused rather than the victim has meant that indices of violence against women continue to grow. This gave added importance to WBFA’s #EndViolence Webinar. The theme of the webinar was ‘Assessing the role of the multidisciplinary team in recognising, reporting and ultimately, reprimanding perpetrators in cases of VAWG’. The speakers actively discussed and detailed their roles as stakeholders in providing intervention plans for survivors and victims. H.E Toyin Saraki in her keynote speech detailed the intervention programmes of the Wellbeing Foundation Africa via their Wellbeing Midwives who have been trained to spot the early warning signs of a GBV victim, whilst the foundations Mamacare classes have remained a point of communication, community and safety for women throughout their pregnancy. Dr Abudullah described the tireless work of the UNFPA’s advocacy efforts in Africa in the areas of data gathering and analysis, increased training of healthcare workers to tackle the rising cases of GBV and by building a referral pathway system for the safe reporting of GBV victims. Photojournalist Fati Abubakar gave a candid insight into her work which has seen her go into the epicentre of the Boko Haram scourge & detail through a visual medium the tragedy taking place in north east Nigeria. She emphasised the importance of visualisation which gives strength to the story of the victim. Journalist Aisha Salaudeen, helped participants to understand the variety of ways to help illuminate the story of GBV cases, emphasising that news agencies must ensure not only the safety of the victim when describing their travails but also to adhere to a code of conduct to protect the dignity of survivors of GBV whilst also telling their story with empathy. Dr Otun Olalekun provided a thorough case study of the ongoing advocacy projects and Initiatives the WBFA are currently conducting in the fight against GBV. This includes the creation of the community based adolescent program which helps teach young girls about GBV and how they can protect themselves and the continuation of the far reaching MamaCare program which has educated and engaged midwives and health workers in over 40 different facilities throughout Nigeria in the areas of S/GBV. The webinar provided a discursive platform for a plethora of professionals, advocates, health workers and policy makers to engage in an issue of great importance. It was resolved that collective efforts will be undertaken to engage key stakeholders in tackling S/GBV whilst focusing on enhancing frontline efforts, aiding security and shadowing facilitation and strengthening abuse referral processes. When I launched the Wellbeing Foundation Africa Global Foundation For Elimination of Domestic Violence by way of the Peace One Day collaboration back in 2012, I was on a trajectory towards what is today, the actualisation of my commitment to the #ICPD25 three zeros; zero unmet need for contraception; zero preventable maternal deaths; and zero gender-based violence and harmful practices, such as child marriage and female genital mutilation. Since then, my commitment to #endingviolence has remained a daily priority, and is personified through my Wellbeing Foundation Africa’s community midwives. The continuum of care offered by way of the #Mamacare360 maternity programs, and every educator and practitioner’s efforts to remain working in tandem with the next generation of young men and women and their families through PSHE to tackle and contribute to the lessening of these dire figures remains both critical and crucial. As we unite to fund, respond, prevent and collect the key evidence and expertise to end this ongoing silent pandemic, I remain resolute in advocacy and actions towards recognising and championing human rights, safety, protection and justice to #endVAWG.
FROM November 25th, 2020
The most powerful way for an advocate to authenticate her message, is to remain at the heart of the demographic requiring its voice to be heard, but equally so, to join forces with other committed voices. My mission to confirm collective needs, develop solutions and provide for society's most vulnerable citizens means galvanising action and joining forces voices - during these #16days of activism and beyond. Women and girls must be made safe, and we must #EndViolence, now. Comfort Lamptey H.E. Jesper Kamp Siddharth Chatterjee Segun Awosanya Kingsley Moghalu and our own dear Wellbeing Foundation Africa Vice President Dr Alero Roberts Thank you. We are for others, who we are for ourselves. #16days #WBFA16days [embed]https://youtu.be/O1bb09DeATw[/embed]
FROM October 21st, 2020
Our nation’s young citizens were shot in cold blood as many of them sat on the ground singing our national anthem. They were shot by their own army, by soldiers whose job it is to protect them. And they were shot in the complete absence of members of Nigeria’s Police Force, whose job it likewise is to protect the lives and property of civilians, and who have sadly proven themselves to be under-trained, under-equipped and thus over-strained in times of crisis, incapable and unwilling to exercise the standard stewardship of crowd control.
It is no secret that the peaceful protests concern the glaring impunity and militarization of the Nigeria Police Force’s Special Anti-Robbery Squad’s brutality towards young Nigerians which had reached the fever pitch of a public safety emergency, culminating in widespread reports of intimidation, harassment and extrajudicial killings – and that young people had organically risen, together, yet leaderless, to peacefully oppose this constant threat to their normal lives. In the last 24 hours, these protests were visibly disrupted in several cities by armed thugs. While the latter appeared to have the backing of the organs of state, in some instances they even killed innocent policemen. Last night, the Nigerian Army came out of its expansive barracks to ‘control’ a group of protesters on the Lekki Bridge Toll Gate, linking two of Lagos’s most exclusive residential communities. The young people had gathered peacefully behind a barrier as can be seen from all manner of media footage. The army fired live rounds not into the air but into the crowd, at close range, killing several and injuring an indeterminate number – in a flagrant contravention of the protocols of the International Covenant on Civil and Political Rights and the Rome Statute of the International Criminal Court. Moreover, in so doing the commanding officer ignored the human rights of freedom of speech and assembly, and the right to protest peacefully, despite Nigeria being a signatory to the ICCPR.My ears have rung with the mournful blare of howling sirens ever since, as ambulances contributed by private hospitals made their way, with difficulty through the curfews and against the odds, to the scene of bloodshed and death, to try to provide care, for the injured, and the murdered dying.
Behind every statistic of inhumanity and injustice is a story, and behind each human being and young citizen is a family. The Nigerian flag, standing for peace, progress and unity, has been indelibly stained with the blood of our young citizens, who themselves were protesting against the SARS’s notorious record of thousands of incidents of rape, torture, un-anaesthetised testicular castrations, and extra-judicial killings, not to mention wanton acts of theft – the very crime it was established to curb. As a mother and grandmother, and I know I am not alone, I fully understand the determination of the youth movement advocating peacefully to #EndSARS and #ReformPoliceNG in Nigeria. At the same time, as a patriot, I am deeply concerned by the disruptions to the nation's safety, peace and productivity.To build a nation, youth empowerment and youth development should be supported as a process where young people are encouraged to take charge of their lives. They should be supported as they address their situation, transform their consciousness through their own beliefs, values, and attitudes, and take action in order to improve their lives. Youth empowerment is a gateway to much needed inter-generational equity, civic engagement and democracy building.
All they had were their voices, hopes, aspirations and patriotism. If their words were swords, then we know how frightening words must be for the current administration. How can an invitation to sit down at a table for proposed dialogue be so frightening as to be simultaneously accompanied by fatal aggression and bloodshed? Who called our army out to kill, maim and injure our nation’s youth – all of whom eagerly and enthusiastically give a year of their efforts and energies to our mandatory National Youth Service Corps.
It is a travesty, and a crime, that young Nigerians should be shot in cold blood simply because they empowered themselves to develop and declare five wishes to live, work and prosper with respect and rights, as occurred on 20th October, 2020. Silence is not an acceptable answer amidst the public calls for dialogue, and Nigeria must hold itself to account.
I urge Nigerian officials and the Nigerian military, to immediately cease the violent and in part fatal crackdown on peaceful protesters in Nigeria. I urge the Nigerian Police to redouble its discipline to safely secure lives and property. My heart is broken along with all those who have lost a loved one in the violence. I ask the world and the diplomatic community to stand with Nigerians who are peacefully demonstrating for police reform and an end to injustice and corruption in our democracy.
I thank the churches and religious leaders, who threw open their parish doors to offer our nation’s young citizens refuge and have sought to encourage the government to engage in a good-faith dialogue with civil society. It is time to address these long-standing grievances and work together for a just, inclusive, peaceful and united Nigeria. I thank the hospitals that have worked tirelessly and free of charge to do what they could to treat the gunshot wounds many young people had. It was an act of profound solidarity at a time when our nation’s officials abandoned our young. For the blood of Nigeria’s young citizens that has been spilled, for daring to raise their voices to peacefully demand a better future of inter-generational equity and accountability for all, we must do our utmost to ensure that their blood was not shed in vain. Our nation just celebrated 60 years of independence, autonomy, agency and governance. We remain in measured hope as we pray that our young citizens continue to surpass us in their achievements, and we will not forget.FROM October 15th, 2020
FROM October 12th, 2020
The anguished scenes coming from our beloved nation Nigeria, of peaceful young protesters being forcefully dispersed, arrested and even injured and killed, are cause for sobering concern, even as many have noted the announcement that the SARS is to be immediately disbanded. The scenes speak to the state of the nation's wellbeing, and what affects one citizen, affects us all. The Economic and Social Research Council, which supports police reform in Nigeria, has assessed that between 2015 and 2019, over 40,000 lives were lost to violent crime, civil unrest and banditry, over 1,000 police officers died or were missing in the line of duty, over N600 billion Naira is estimated to have been lost to violent unrest and crime, while thousands of complaints have been filed to and by the police. Among those is a complaint regarding the molestation of a group of 70 women alleged to be sex-workers in Abuja in 2018 and 2019. That these women were treated by the authorities as less than human is at once a grave offense to their dignity and at the same time, an all-too-common occurrence. Our commitments and endorsement of United Nations Resolution 1325 specifically call for a reduction on violence against the female gender particularly because it is ultimately women and girls who bear the brunt in conflict. That our police system so blatantly flies in the face of internationally recognised orders that promote the healthy development of a country is antithetical to its purpose and existentially damaging to our nation's progress. It is poignant that yesterday was International Day of the Girl, and it was notable that I saw images of steadfast female activist Aisha Yesufu insist on social justice, and so many other young women rising to provide representation and relief. I see hope and practical expressions of loyalty to our nation's ideals in our women and youth. Our young citizens have made five requests of our nation's leaders:
FROM October 11th, 2020
 Left: Sefi Atta, author and playwright
Left: Sefi Atta, author and playwrightFROM October 5th, 2020
This weekend, the Wellbeing Foundation Africa's MamaCare Antenatal & Postnatal Education Program's Whatsapp Maternity Support had the honour to be featured in British Vogue Magazine's Forces For Change October Edition about their work reaching every last mile to care and counsel mums, babies, and their families. I am so proud of their embracing the promise of technology to democratize access to accurate information from conception and the cradle, to age. MamaCare’s WhatsApp world is far from your typical online talkfest. It’s a safe space for pregnant women and new mums in Nigeria to connect, commiserate, congratulate, and voice their honest concerns — including the stuff deemed uncomfortable or taboo — knowing they can count on getting a prompt, accurate response in return. Our midwives, sometimes referred to endearingly as “Mama” by their group members, field questions about everything from breast feeding and nutrition to pregnancy sex and postpartum spotting. By harnessing the power of digital communication I believe that MamaCare will amplify its impact. What’s currently reaching 8,000 mothers a month, can soon evolve into well over 200,000. And with about seven million babies born in Nigeria each year and our goal of providing every single one of them and their families with a safe delivery and quality care, the new WBFA chatbot will be a major step in fast-tracking that ambition. Our tech is going to underpin our frontline. We want to be able to deliver lessons, immunisation reminders, nutrition advice, all by WhatsApp. If something as obtainable as WhatsApp has the capacity to improve medical outcomes for Nigeria’s most disadvantaged women through the diffusion of reliable information, then the world might not be as far from widespread healthcare reform as we once thought. As the developers of a wide range of home and health facilities based health records, the Wellbeing Foundation Africa believes that the role of data collation and analysis is crucial to the evolution of egalitarian healthcare systems. When we’re at a crossroads and we’re not sure what to do, data, if it’s openly and freely available, can lead us forward, hovwever we can’t access data if we’re not accessing the promise and realities of technology. I’m hoping that the WBFA’s use of technology will add this extra layer to all of our programming, and democratise it. Read more about my Forces For Change interview: WhatsApp Is The Key To Democratising Global Healthcare>>
FROM October 1st, 2020
During my childhood in the 1960's, I remember singing our Independence Anthem confidently in the affirmation that though our tribes and tongues may differ, we stand in brotherhood, proud to serve our sovereign motherland. Our flag is a symbol that truth and justice should reign, and our collective dream of being able to hand on to our children, a banner without stain, as we prayed to the Lord of all creation to grant our request to help us build a nation where no man would be oppressed, and so with peace and unity, Nigeria would be blessed. Nigeria is 60 today, and we have much to celebrate: our indomitable spirit, our endurance, fortitude and resilience - and our hard earned unity. We have an unquenching optimism for progress, and I know that my motherland has come a long way from Independence Day on 1st October 1960 and the vision of our founding fathers till today. Reflecting on our nascent years I can declare that Nigeria was indeed blessed, albeit simply, with abundant natural resources to grow a healthy population and prosperous future for all. At the same time, agitation for equitable management of our abundant natural resources, and the resulting humanitarian crisis directed our first experiences of multilateralism. International donor agencies arrived to assist the suffering and displaced victims of our civil war, as the nation strove to heal its wounds. The multilateral agencies remain with us today, implementing key services towards the sustainable development goals, working alongside national and frontline organisations. In those early formative years, lacking encounters with the basic day-to-day development challenges that shape creative public policy, our youthful nation paid little intentional and deliberate attention to the status of women and girls. We were so busy building our national unity, which at times was imperiled, that it didn’t occur to us to be intentional in our support for young women and girls to rise, even though culturally we have always revered and respected matriarchs and motherhood. This dichotomy has contributed to shaping some of the most dire realities of not meeting the needs of our women and girls that we as a nation face and experience today, where despite 50% of the electorate being women, the male gender occupies a disproportionate amount of cross-sectoral leadership positions.
The problems we face as a nation are a manifestation of the way in which we built our country, but today, at 60, and surely matured, we have an opportunity to catalyse an inclusive and cohesive course correction. We are centred on reiterating the national call to arise and serve our fatherland with love, strength and faith. We must reiterate that the labour of our heroes’ past shall never be in vain, and to serve our peoples with heart and might: one nation bound in freedom, peace and unity - to reach every last mile.
Right now, Nigeria’s Covid-19 deaths are comparatively low, and our nation’s endurance is high and strong; to me, possibly the product of a fortuitous resilience shaped by our long epidemiological history. However it is clear that the race to combat, contain and control Covid-19 is a marathon and not a sprint. According to The Economist’s Covid Collective Report, states like Nigeria are at risk of being “disproportionately affected because they have the least resources and infrastructure to grapple with the pandemic’s dire health and economic repercussions.” While richer countries are able to do more testing and prepare economic safeguards and recovery, Nigeria has recorded fewer tests per thousand people and has fewer resources to plan recovery. Examples of collaboration among scientists, however, show that models for better cooperation are possible, and indeed a timely focus on home-grown research and development from Nigeria may yet have much to teach the world. Stronger frameworks and mechanisms for international cooperation are required to mitigate the adverse effects on lives and livelihoods globally, and in fragile settings in particular. The fact that 172 countries globally are engaged in discussions to participate in COVAX – a Covid-19 vaccine global access facility – demonstrates just how powerful global cooperation can be in finding collective solutions to collective problems. On our 60th celebration of independence, we reaffirm our patriotic call to direct our noble cause: that our leaders are guided right, our youth are helped to know the truth, grow in love and honesty, living just and true, attain great and lofty heights, to build a nation where peace and justice shall reign, a pledge to the progress of our nation. But we cannot deny that Covid-19 has laid bare fissures in the multilateral system with far-reaching implications. From climate change to economic recessions, geopolitical tensions to AI disruption, truly global challenges are only going to become more frequent in our increasingly-interdependent world. Every country is only as strong as the weakest link in the chain thus we know that the gaps in domestic and international safety nets are not just a threat to the world’s vulnerable populations but also to the functioning of the global economy and society as a whole. As we celebrate the transformative power of patriotism, we must remember that no nation thrives entirely alone, and should work towards reviving multilateralism’s promise to ‘leave no one behind’ with particular focus on the effect of the pandemic on our most vulnerable women and girls. With the pandemic upending the world’s structural norms, Nigeria has an opportunity to come out of this dark time with a new energy based on the evidence of what works—and what does not work— to achieve our goals sustainably and for all. To meet the challenges of the 21st century, each and every one of us as individuals, along with our national governments, multilateral actors and humanitarian leaders must heed Covid-19’s wake-up call and unite to give multilateralism the “teeth” it needs to reform, replenish and strengthen national and global resilience both now and when the next crisis emerges, to ensure that our beloved nation Nigeria, and our people will survive, transform and thrive.
FROM September 26th, 2020
FROM September 18th, 2020
FROM September 15th, 2020
I am deeply concerned by the recent findings that Nigeria has overtaken India as the world capital for under-five deaths, according to the UNICEF report 'Levels and Trends in Child Mortality,’ particularly as we had previously seen significant improvements in Nigeria between 1990 and 2015. This distressing news comes just as we congregate virtually this year for the United Nations General Assembly. The report compiles data spanning three decades from 1990 to 2019, and it reveals that 49% of all under-five deaths in 2019 occurred in just five countries: Nigeria, India, Pakistan, the Democratic Republic of Congo and Ethiopia. It finds that Nigeria and India alone account for almost a third of the deaths, and what is evermore worrying is that it is clear that there is a strong potential of a continued mortality crisis in 2020 with the additional strain of the coronavirus pandemic.
FROM September 11th, 2020
This week, my Wellbeing Foundation Africa's partners at Amref Health Africa led an excellent session - "A Health Accountability Framework, Holding Governments Accountable for their Health Commitments” . I warmly welcomed the discussion of the importance of supporting strong accountability frameworks, such as the Right to Health Index, that can hold governments to account on their health commitments.
The Right To Health Index is grounded in the recognition that health accountability needs to move away from using general statistics and focus instead on identifying specific indicators for use in human rights. In doing so, accountability frameworks can facilitate the realization of health as a human right and universal health coverage for all.
Health as a human right has always been central to The Wellbeing Foundation Africa’s work, particularly the infusion of poverty alleviation, rights and gender-based programming into the WBFA's Alaafia Universal Health Coverage Scheme Fund in partnership with the PharmAccess Foundation and Hygeia Community Health Plan.
 The Fund, supported the Kwara State Health Insurance Scheme established since 2007 by advocating for the 2012 and 2017 enabling state health insurance legislation, and by directly providing yearly capacitation fees for 5000 pregnant and newly delivered women, as well as adolescents, people living with HIV/AIDS, and elderly beneficiaries annually, within it's over 100,000 enrollees from 2015 onwards.
Certainly, this availability of quality affordable care has contributed in no small measure to Kwara State maintaining its status as the state with the lowest maternal and under-5 mortality in Nigeria, at a time when the nation has been confronted with the unfortunate fact of having overtaken India as having the highest and worst preventable deaths of mothers and their young children globally - underscoring the importance of sustaining focused efforts across all 36 states of the federation to arrest this devastating trend of neglect.
https://www.youtube.com/watch?v=lVfErQTKH6Y&feature=youtu.be
H.E. Senator Dr Abubakar Bukola Saraki, MBBS, CON, 13th President of the Senate and Chair, 8th Session National Assembly, Federal Republic of Nigeria, Former Kwara State Governor and Chair, Nigeria Governors Forum, at the Scale Up Ceremony of Kwara Community Health Insurance Scheme, Afon, Kwara State, 2009
I was also delighted to learn this week that the health insurance scheme has been recently re-launched with a target of 10,000 more mandatory enrollees. I heartily commend the PharmAccess Foundation and other partners for their focused tenacity in ensuring that the exemplary health insurance-driven universal health coverage model that all partners worked so hard to create and innovate, driven by the mutual vision of H.E Dr Abubakar Bukola Saraki and the late acclaimed global health expert and medical research scientist Joep Lange to render affordable quality health care for all will continue to support and benefit many more people into the future.
[caption id="attachment_1199" align="aligncenter" width="603"]
The Fund, supported the Kwara State Health Insurance Scheme established since 2007 by advocating for the 2012 and 2017 enabling state health insurance legislation, and by directly providing yearly capacitation fees for 5000 pregnant and newly delivered women, as well as adolescents, people living with HIV/AIDS, and elderly beneficiaries annually, within it's over 100,000 enrollees from 2015 onwards.
Certainly, this availability of quality affordable care has contributed in no small measure to Kwara State maintaining its status as the state with the lowest maternal and under-5 mortality in Nigeria, at a time when the nation has been confronted with the unfortunate fact of having overtaken India as having the highest and worst preventable deaths of mothers and their young children globally - underscoring the importance of sustaining focused efforts across all 36 states of the federation to arrest this devastating trend of neglect.
https://www.youtube.com/watch?v=lVfErQTKH6Y&feature=youtu.be
H.E. Senator Dr Abubakar Bukola Saraki, MBBS, CON, 13th President of the Senate and Chair, 8th Session National Assembly, Federal Republic of Nigeria, Former Kwara State Governor and Chair, Nigeria Governors Forum, at the Scale Up Ceremony of Kwara Community Health Insurance Scheme, Afon, Kwara State, 2009
I was also delighted to learn this week that the health insurance scheme has been recently re-launched with a target of 10,000 more mandatory enrollees. I heartily commend the PharmAccess Foundation and other partners for their focused tenacity in ensuring that the exemplary health insurance-driven universal health coverage model that all partners worked so hard to create and innovate, driven by the mutual vision of H.E Dr Abubakar Bukola Saraki and the late acclaimed global health expert and medical research scientist Joep Lange to render affordable quality health care for all will continue to support and benefit many more people into the future.
[caption id="attachment_1199" align="aligncenter" width="603"] Wellbeing Foundation Africa, Hygeia Community Health Plan, Pharmaccess Foundation, World Bank Nigeria, Federal Ministry of Health at Alaafia Universal Health Care Scheme Fund Conclusion Breakfast Meeting, Abuja, Nigeria, January 2017[/caption]
Wellbeing Foundation Africa, Hygeia Community Health Plan, Pharmaccess Foundation, World Bank Nigeria, Federal Ministry of Health at Alaafia Universal Health Care Scheme Fund Conclusion Breakfast Meeting, Abuja, Nigeria, January 2017[/caption]
FROM September 2nd, 2020
FROM August 25th, 2020
FROM August 11th, 2020
 Riskiat and her children accepting the donation from the Wellbeing Foundation Africa[/caption]
As a child, Riskiat went to primary and secondary school, but didn’t sit her final examinations because her parents could not pay the fees, as she explained to PUNCHNG. Instead, her parents enrolled Riskiat in an apprenticeship, and following the apprenticeship, she worked in a shop where she met her husband, Abdulwasiu, in her early 20s.
After courting for a year, Riskiat and Abdulwasiu married, and Riskiat quickly gave birth to three children: five-year-old Kaosara and one set of twins, two-year-olds Hasanat Kehinde and Taiwo. The daughters, Kaosara and Hasanat Kehinde, inherited Riskiat’s distinct eye colour, while Taiwo, the son, had traditional brown eyes. The family lived together in Abdulwasiu’s family home, and Abdulwasiu, a vulcaniser, struggled to support the children’s diet and education, particularly as the COVID-19 pandemic brought Nigeria to a halt.
It is clear through Riskiat’s interview that Abdulwasiu’s family was distrustful of Riskiat already—but the trigger point that led to the family breakdown happened when the male twin, Taiwo, fell ill earlier this year. As Riskiat illustrates in PUNCHNG, the family could not financially support his care, and ultimately, Taiwo died from his illness. The grief and devastation eroded the family’s cohesion even further: distraught because of the loss of his son, poverty-stricken and pressured by his family’s scepticism about the fact that Riskiat and the blue-eyed daughters had survived, Abdulwasiu instructed Riskiat to move out of his parents’ home.
“He told me that his parents said they could not live with children with blue eyes. My husband also said his parents told him to marry a woman that would produce children with normal eyes,” she told PUNCHNG.
We have always known that unplanned point-of-care medical expenses can throw families into poverty, but Risikat’s story shows us the devastating effect that unavailability of medical coverage can wreak. It impacts lives negatively far beyond the original community coverage aims of health for all.
What Riskiat has yet to experience is self-sustaining autonomy via her own economic empowerment. As a child she was barred from further education because her family could not afford the fees. As a young adult, she attempted to make a living for herself, but instead married young and then struggled to feed, educate and protect her family because she relied on her husband, who could not support them. At 30, Riskiat has fire in her belly and light in her blue eyes: she insists that she does not want her husband back, and is steadfast in her interest in finding the best path forward for her children.
“God who created us has plans for every individual. I don’t have any specific thing (planned) for her and her sister. I only wish that they would become great in future” she said to PUNCHNG.
[video width="848" height="480" mp4="https://toyinsaraki.org/wp-content/uploads/2020/08/WhatsApp-Video-2020-08-08-at-2.25.56-PM.mp4"][/video]
Riskiat’s inability to control and plan her own life is the story of many women just like her, particularly in Nigeria. Country-wide, at age 20, less than 4% of men are married, compared to about 50% of women in rural areas. In some areas, around 40% of girls are married and 11% give birth all before age 15, which robs them of their educational attainment, career mobility and earning power, and makes them vulnerable to dangerous pregnancy complications like fistula. Moreover, we know that when we invest in women and girls, they invest in everyone else around them. That’s why I was not surprised to read that Risikat took a decision to sell her small patent medicines shop to raise the resources to feed her family during trying times. Women typically invest a higher proportion of their earnings in their families and communities than men. Women’s economic participation and ownership of their own finances helps overcome poverty and improves children’s nutrition, health, and school attendance.
Reading about how Risikat lost her twin son Taiwo, due to not being able to afford the necessary medical care in Kwara State in 2020, shocked my core beliefs, advocacy and actions regarding universal health coverage. From 2007 to 2016, my Wellbeing Foundation Africa’s Alaafia Universal Health Access Fund had supported the Kwara State Government in its partnership with Hygeia and the Pharmaccess Foundation, in launching the Kwara Community Health Insurance Scheme (CHIS), providing a comprehensive package of healthcare to all indigenes, and mitigating the economic devastation of unplanned point of care expenses with a record-breaking and prize winning low capacitation fee recognised as recently as 2012, 2014 and 2015.
The Kwara State CHIS was renamed KwaraCares in late 2018, and shockingly, was inexplicably not accessed or not available to Risikat and her children in 2020 despite its strongly vociferous media presence.
So when I intervened in Riskiat’s situation with a token donation for her children’s education, it is not just because of compassion for a woman and children with striking eyes. It is because a small investment in Riskiat—allowing her basic economic empowerment, and the ability to make her own autonomous choices for her life and that of her children independently—has the potential to stop a cycle of disempowerment and negative dependency that Riskiat and so many others experience.
Alongside making the donation, I also immediately requested that the eminent Professors of Medicine at the long renowned University of Ilorin Medical Centre of Excellence and Teaching Hospital respectfully offer the family full medical screening, as the striking beauty of their blue eyes aside, it is not unusual for cases of ocular albinism to be associated with rare genetic conditions.
I made this donation and medical referral as I continue to advocate that public health and education policies must deliberately, intentionally, and accountably replenish resources. They must reinforce learning and knowledge and embrace gender-data statistical values in managing pro-poor innovations and universal health coverage, to put people first, particularly women, newborns and girls, and leave no one behind, particularly in Kwara State where the Wellbeing Foundation, stakeholders and non-governmental organisations continue to work so hard and long to deliver the lowest under-5 mortality in the land.
Riskiat and her children accepting the donation from the Wellbeing Foundation Africa[/caption]
As a child, Riskiat went to primary and secondary school, but didn’t sit her final examinations because her parents could not pay the fees, as she explained to PUNCHNG. Instead, her parents enrolled Riskiat in an apprenticeship, and following the apprenticeship, she worked in a shop where she met her husband, Abdulwasiu, in her early 20s.
After courting for a year, Riskiat and Abdulwasiu married, and Riskiat quickly gave birth to three children: five-year-old Kaosara and one set of twins, two-year-olds Hasanat Kehinde and Taiwo. The daughters, Kaosara and Hasanat Kehinde, inherited Riskiat’s distinct eye colour, while Taiwo, the son, had traditional brown eyes. The family lived together in Abdulwasiu’s family home, and Abdulwasiu, a vulcaniser, struggled to support the children’s diet and education, particularly as the COVID-19 pandemic brought Nigeria to a halt.
It is clear through Riskiat’s interview that Abdulwasiu’s family was distrustful of Riskiat already—but the trigger point that led to the family breakdown happened when the male twin, Taiwo, fell ill earlier this year. As Riskiat illustrates in PUNCHNG, the family could not financially support his care, and ultimately, Taiwo died from his illness. The grief and devastation eroded the family’s cohesion even further: distraught because of the loss of his son, poverty-stricken and pressured by his family’s scepticism about the fact that Riskiat and the blue-eyed daughters had survived, Abdulwasiu instructed Riskiat to move out of his parents’ home.
“He told me that his parents said they could not live with children with blue eyes. My husband also said his parents told him to marry a woman that would produce children with normal eyes,” she told PUNCHNG.
We have always known that unplanned point-of-care medical expenses can throw families into poverty, but Risikat’s story shows us the devastating effect that unavailability of medical coverage can wreak. It impacts lives negatively far beyond the original community coverage aims of health for all.
What Riskiat has yet to experience is self-sustaining autonomy via her own economic empowerment. As a child she was barred from further education because her family could not afford the fees. As a young adult, she attempted to make a living for herself, but instead married young and then struggled to feed, educate and protect her family because she relied on her husband, who could not support them. At 30, Riskiat has fire in her belly and light in her blue eyes: she insists that she does not want her husband back, and is steadfast in her interest in finding the best path forward for her children.
“God who created us has plans for every individual. I don’t have any specific thing (planned) for her and her sister. I only wish that they would become great in future” she said to PUNCHNG.
[video width="848" height="480" mp4="https://toyinsaraki.org/wp-content/uploads/2020/08/WhatsApp-Video-2020-08-08-at-2.25.56-PM.mp4"][/video]
Riskiat’s inability to control and plan her own life is the story of many women just like her, particularly in Nigeria. Country-wide, at age 20, less than 4% of men are married, compared to about 50% of women in rural areas. In some areas, around 40% of girls are married and 11% give birth all before age 15, which robs them of their educational attainment, career mobility and earning power, and makes them vulnerable to dangerous pregnancy complications like fistula. Moreover, we know that when we invest in women and girls, they invest in everyone else around them. That’s why I was not surprised to read that Risikat took a decision to sell her small patent medicines shop to raise the resources to feed her family during trying times. Women typically invest a higher proportion of their earnings in their families and communities than men. Women’s economic participation and ownership of their own finances helps overcome poverty and improves children’s nutrition, health, and school attendance.
Reading about how Risikat lost her twin son Taiwo, due to not being able to afford the necessary medical care in Kwara State in 2020, shocked my core beliefs, advocacy and actions regarding universal health coverage. From 2007 to 2016, my Wellbeing Foundation Africa’s Alaafia Universal Health Access Fund had supported the Kwara State Government in its partnership with Hygeia and the Pharmaccess Foundation, in launching the Kwara Community Health Insurance Scheme (CHIS), providing a comprehensive package of healthcare to all indigenes, and mitigating the economic devastation of unplanned point of care expenses with a record-breaking and prize winning low capacitation fee recognised as recently as 2012, 2014 and 2015.
The Kwara State CHIS was renamed KwaraCares in late 2018, and shockingly, was inexplicably not accessed or not available to Risikat and her children in 2020 despite its strongly vociferous media presence.
So when I intervened in Riskiat’s situation with a token donation for her children’s education, it is not just because of compassion for a woman and children with striking eyes. It is because a small investment in Riskiat—allowing her basic economic empowerment, and the ability to make her own autonomous choices for her life and that of her children independently—has the potential to stop a cycle of disempowerment and negative dependency that Riskiat and so many others experience.
Alongside making the donation, I also immediately requested that the eminent Professors of Medicine at the long renowned University of Ilorin Medical Centre of Excellence and Teaching Hospital respectfully offer the family full medical screening, as the striking beauty of their blue eyes aside, it is not unusual for cases of ocular albinism to be associated with rare genetic conditions.
I made this donation and medical referral as I continue to advocate that public health and education policies must deliberately, intentionally, and accountably replenish resources. They must reinforce learning and knowledge and embrace gender-data statistical values in managing pro-poor innovations and universal health coverage, to put people first, particularly women, newborns and girls, and leave no one behind, particularly in Kwara State where the Wellbeing Foundation, stakeholders and non-governmental organisations continue to work so hard and long to deliver the lowest under-5 mortality in the land.
FROM July 22nd, 2020
I am overjoyed to receive a photo and update from a Wellbeing Africa Foundation mum today, and I must share the story.
In 2017, Mrs O was pregnant with triplets, and had been a student of my #Mamacare360 program. She needed, but couldn't afford a Caesarean, and the hospital just kept her waiting. The hospital was ready to abandon them. I have always advocated for socio-economic birth preparedness within universal health coverage, but birth waits for no-one, so I dashed there to help immediately. That's because a sound anti-poverty strategy should not only aim to increase incomes, but also provide the poor with a variety of assets — personal, social, political and environmental to help them overcome the myriad of challenging circumstances. Sometimes being there for the right person, with the right help, at the right place, can change a life (or in this case, three more lives) way beyond the original aim of poverty alleviation. Here is a photo of the absolutely beautiful triplets today: they have grown so big and strong, and it has made a sunny day today even brighter. [caption id="attachment_1178" align="alignnone" width="300"] The triplets, 2020[/caption]
The triplets, 2020[/caption]
FROM July 21st, 2020
A few weeks ago, I read an absolutely harrowing story of abuse in Akwuke, near Enugu City, Nigeria, and it has been on my mind ever since. I am consumed by the fact that its graphic nature and intimate impact were entirely preventable, if only the right systems were in place.
Early in June, a wife and mother of two young boys—we will call her Mrs. K—asked her husband for money to prepare food for the family. He had a history of violence, and he lashed out about the inquiry: when she proceeded to make pap for her 3-month-old baby, he doused her breasts in boiling water. She reacted in the throes of excruciating pain, and also unable to breastfeed her baby. The Women’s Aid Collective (WACOL) posted the story on Twitter, including graphic photos that I am choosing not to continue to publicise. WACOL has confirmed that the husband is now in police custody, but the psychological, emotional and physical damage to Mrs. K and her children has been done, and it is on us to use this case as a calling to rethink how we are handling the scourge of domestic violence in Nigeria.
The story is the horrific climax of a pattern that we know to be true when it comes to domestic violence: notable triggering factors for the husband’s actions in this case are concerns about money, food, and the fact that Mrs. K was exercising her personal autonomy—through breastfeeding the baby. We know firstly that domestic violence is rising due to pressures about money amidst the pandemic; secondly, research also shows that male partners who are inclined to violence increase aggression during pregnancy and after birth, and thirdly, we know that jealousy (in this case, about feeding the baby) can be a trigger for men inclined to violence.
While the global community is aware of these factors, limited access to reporting pathways means local organisations weren’t able to shield Mrs. K before the abuse was so great that it required extreme intervention. Her case makes evident that the reporting of incidents of intimate nature, such as sexual assault and domestic violence, necessitates the transfer of Sexual Assault Referral Centres (SARC) from police stations to hospitals.
The Nigerian police force is culturally hyper-masculine and male-dominated, and Nigerians are 20 times more likely to be killed by the police than by terrorists. It is obvious that an aggressive and masculine environment in a conservative cultural setting is not a safe space for vulnerable women to share intimate stories about private parts of their body. In fact, a police station in Nigeria could be the worst place I could think of for a woman to go to seek relief. That’s why I’ve begun reaching out to call for a timely policy shift, nationally, to shift SARCs to hospitals: the hospitals would assume locus as expert witnesses, and bear the formal responsibility for reporting and advising the police on sexual and domestic violence cases. In turn, the idea is that injured women, or women in danger would feel more comfortable seeking treatment about intimate issues than in a police station. They would be treated for their ailments, and hospital staff would assume the responsibility for translating actionable items to the police. Like any crime, the prospect of swift justice, would also serve as a deterrent, and thus a very timely tool in the strategy to effect preventive social behavioural change.
This call to action is about ensuring we have the right systems in place to safeguard and ultimately empower vulnerable women with the public resources we have available. It is said that sexual and gender based violence is within the lived experience of almost half of our women and girls; equipping health personnel with specialist SGBV SARC and mental health training is both prerequisite, and an imperative.
At the Wellbeing Foundation Africa, we have long offered women attending our health facility based Mamacare antenatal and postnatal sessions a safe space, and a curriculum to discuss concerns, and if needed, report their worries. Nigeria’s updated National Gender Policy should take a whole-family, socio-economic and mental health approach to tackling the scourge of domestic violence; and one way we can start is by ensuring the safe haven of refuge, of a kind of solace: a comfortable environment for vulnerable women to give forensic evidence, find relief, and heal. We must do it for Mrs. K.
FROM July 14th, 2020
I thoroughly enjoyed kick-starting the new week by participating at the UN High-level Political Forum side event entitled, "From Page to Action: Accountability for the Furthest Left behind in COVID-19 & Beyond.” The conversation was strong, timely and direct, as well as being a fantastic way to launch the 2020 Report of the UN Secretary-General’s Independent Accountability Panel for Every Woman Every Child. Co-hosted by the Governments of Japan, South Africa, and Georgia and co-organized by the Every Woman Every Child Secretariat, the Independent Accountability Panel (IAP), International Health Partnership for UHC 2030 (UHC2030), and the Partnership for Maternal, Newborn & Child Health (PMNCH), I appreciated the opportunity of knowledge sharing to deepen the efforts and engagement of my organisations, the Wellbeing Foundation Africa, and Wellbeing For Women Youth Voices towards promoting institutional accountability at national, regional and global policy tiers. As we herald the new commitments targeted at mitigating the disruptions of the Sars-Cov2 pandemic in expectation of focused investments, we are once again reminded that the initiation, solution and fiscal appropriations to drive the delivery and accountability of truly accessible health for all must be embraced and fall within the remits of local and national parliaments. Today, and every day, I particularly commend the WHO Partnership for Maternal Newborn And Child Health PMNCH's ongoing strong collaboration with the International Parliamentary Union IPU, as signalled by the Inter-Parliamentary Union's historic first resolution towards Universal Health Coverage in 2019, substantiating global approaches to recordkeeping. I was particularly enthused by contributions from a number of high-level speakers and leading voices for the delivery of Universal Health Coverage, namely, H.E. Mr. Cyril Ramaphosa; President of South Africa; Chairperson of the African Union, Mr. Shinichi Kitaoka; President, Japan International Cooperation Agency JICA, Ms. Joy Phumaphi, Co-Chair, Independent Accountability Panel for Every Woman Every Child, Mr. Elhadj As Sy; Chair of the Board, Kofi Annan Foundation, Ms. Gabriela Cuevas Barron, President, Inter-Parliamentary Union, Dr. Khuất Thị Hải Oanh; Civil Society Engagement Mechanism, UHC2030, Dr. Natalia Kanem, Executive Director, UNFPA, H.E. Mr. Kaha Imnadze; Permanent Representative of Georgia to the UN, H.E. Ms. María Fernanda Espinosa Garcés; Member, UHC Movement Political Advisory Panel, UHC2030, Ms. Evalin Karijo; Project Director, Youth in Action, Amref Health Africa, Mr. Peter MacDougall, Assistant Deputy Minister of Global Issues and Development, Global Affairs Canada, Dr. Tedros Adhanom Ghebreyesus; Director-General, WHO; Chair, H6 Partnership, Rt. Hon. Helen Clark, Former Prime Minister, New Zealand; Board Chair, PMNCH, and of course, Ms. Gillian Tett; Chair of the Editorial Board & Editor-at-Large (US), The Financial Times (Moderator), alongside so many EWEC partners and frontline organisations. But as the COVID-19 pandemic’s grip on the world shows no immediate signs of loosening, organisations must therefore acclimatise effectively, by integrating the dual-mindset towards technology, in equipping their workforces and ensuring that the dissemination of information – particularly pertaining to health - remains both accurate and accessible. By making this part of an ongoing global transition a priority, we will see to it that society’s most vulnerable individuals are able to continue accessing the information and services which remain a key component in their livelihood. As Nigeria, seeks to mitigate the regrettable and inexcusable reputational damage that recent appalling breaches in cybersecurity have caused, we must also underscore the vital role that technologically supported security platforms play in enabling for remote operations and a continued key health services to be delivered when implemented effectively. Invoking cybersecurity measures have been and continue to constitute a key component in ensuring that accurate health information is circulated worldwide, particularly during this Covid-19 pandemic. We must therefore support all initiatives and efforts in the direction of this construct remaining a top global priority.
FROM July 6th, 2020
For many years, the welcomed priority, purpose and daily-sensitised goal for Women and Girls, Families and Communities - nationally and across our continent as a whole - has been to solidly create, inform, empower and manifest a true demonstration of equality, access and social responsibility regarding their health, their education and the equitable opportunities afforded to assure and improve basic wellbeing, from birth to age.
Through the continued collaborative efforts of our nation’s healthcare professionals, researchers, thought-leaders, community volunteers and the service users themselves, Nigeria had long subscribed to the notion of investing in Universal Basic Education. However, the first time that citizens experienced the concrete benefit of an intentional basic or primary public health assistance was in 2018, when Nigeria’s 8th National Assembly appropriated the Basic Health Care Provision Fund – a pinnacle moment in the redemption of the 2001 Abuja Declaration towards achieving Universal Health Coverage. Today, that resounding national applause remains of strong resonance to the Joint Civil Society Organisations Primary Healthcare Revitalisation Support Group to the Eighth National Assembly, which I had chaired.
With that being said, a real sense of recurring readiness and receptiveness to campaigns, cultural change and the communication surrounding health and wellbeing as a whole remains palpably evident, statistically proven and collectively celebrated by many – both nationally, and worldwide, and is categorised amongst what still remains a series of promising results acquired through WBFA’s advocacy and partnership efforts with policy-makers and parliamentarians worldwide.
In addition, and perhaps more pertinently given the progression of the ongoing COVID-19 pandemic, my morale embodies the significance and importance of global partnership interventions such as that of the Global Financing Facility and the Global Citizen Fund. Their commitment to amplifying the importance of collective efforts in acquiring globally accessible health tools and resources during the pandemic, brings us all one step closer to the concept of continuity of services becoming a very possible reality.
As, the Global Financing Facility announced its predictions last week, it conveyed a new set of commitments aimed at mitigating the disruption of services to a number of the countries and global communities most in need. GFF forecasts a possible 18% increase in child mortality, and a 9% increase in maternal mortality across Nigeria over the next year as a direct result of essential health services becoming fragmented during this COVID-19 pandemic. We had only recently learnt the surprising news that Nigeria's 9th National Assembly had predicted a reduction in the value of the primary healthcare and basic education budgets, which as unaddressed to date – reflect as cuts.
However, as 30th June marked the International Day of Parliamentarianism, I was also caused to reflect upon the OECD’s interpretations of the role of parliaments during the COVID-19 crisis. The COVID-19 pandemic is posing threats not only to human health and life, but also to people’s socio-economic well-being and countries’ economic growth. According to the OECD, the global economy is currently suffering its deepest recession since the Great Depression in the 1930s.
One of the many visible issues of the current pandemic is the rampant unemployment and loss of income. As well as the increase in poverty, it could impede people from accessing basic services due to unaffordability and inaccessibility. It is estimated that 2.9-5.2 million people could lose their jobs in Indonesia as a result of this global health crisis. Clearly the pandemic is heightening inequality and inequity among citizens as well as within the countries themselves.
Yet, presently, the role of parliament is more relevant today than it has been ever before. Parliaments can propose and adopt necessary laws to assist their respective governments in intercepting and tackling COVID-19 and its adverse impacts. Further, parliaments can oversee the expenditure of the public funds related to COVID-19. It is crucial to ensure that the funds are allocated appropriately, and that all individuals receive fair distribution of strategically proposed COVID-19 containment measures.
In responding to the COVID-19 crisis, parliaments in Nigeria, and around the world have also established designated Task Forces for COVID-19, aiming to provide assistance and support in the form of medical equipment and personal protective equipment to hospitals and community health centres, in a globally observed and commended response. Every state has different capacities and resources to counter the challenges, whether it is providing and maintaining optimal and accessible healthcare, upholding a functioning and thriving society or managing the state of the global economic. Therefore, international co-operation is imperative, in order to ensure that states - especially within low- to middle-income countries, are able to thrive in this moment of crisis, and eliminate their obstacles in tackling COVID-19.
Not surprisingly, three weeks ago, I had joined a high-level discussion on how the ongoing COVID-19 pandemic perpetuates the pressing need to implement Universal Health Care. In welcoming the Africa Leads UHC One By One 2030 Report, and in the new Unite For Action global commitments, I fully agreed that primary health care must cover the breadth of the journey from hospital to hut in communities, and improve the social determinants of all those living and working therein.
We should not wait to improve the situation until, God forbid, the next crisis occurs. We have to ensure that our nations’ socio-economic development would not leave anyone behind, as envisaged by the 2030 Agenda. In that regard, every decision, law and regulation made must also be based on principles of equality, participation, non-discrimination, accountability and transparency.
I have urged all African Leaders to reinforce and reconfigure their commitments to the 2001 Abuja Declarations in order to exceed the minimum pledged 15% of respective Consolidated Revenue Funds, if we are indeed to fulfil our mantra’s of Africa Rising – to match these global commitments with clear manifestation of a sense and purpose, of evidenced intention, to put our people first, justifying continued global partnerships and multi-lateral assistance.
As we face the prospect of reinstating routine primary health and education services that were so destructively interrupted by the coronavirus pandemic, it is clear that Africa needs to factor in the replenishment and reinforcement of investments in both primary health care, and primary education. In doing so, they will build resilience to emerge from the pandemic in a stronger position than before. We must ensure that our weakest frontline services can deliver a healthier, better and stronger educated future for all.
 As we herald the new commitments targeted at mitigating the disruptions of the Sars-Cov2 pandemic, in expectation of focused investments we are reminded then, that the initiation, solution and budgetary injection must primarily derive from the pots that sit within local parliaments, while recalling that in fact, in 2019, the Inter-Parliamentary Union did actively play its part in passing its historic first resolution towards universal health coverage, substantiating global approaches to recordkeeping.
Parliaments themselves should also intensify this co-operation and share their best practices, experiences and challenges in dealing with the COVID-19. International organisations such as the OECD and its Global Parliamentary Network have a pivotal role to play during these unprecedented times. They help to facilitate pertinent policy dialogues on important socio-economic matters and provide us with advice and recommendations, so that parliaments can use them as guidelines to improve the situation and/or propose to its governments.
To use the example of the Indonesian Parliament view that the implementation and achievement of the Sustainable Development Goals (SDGs) cannot be postponed amid the COVID-19 pandemic, I restate the fact that the SDGs should be the measure for parliaments to prevent trade-offs in this moment of crisis, for example, between the economy and health, in any laws or programmes. It is also important to emphasise that the entire Indonesian House of Representatives, including those in the commissions, are working to support the implementation and achievement of the SDGs, supporting resolutions relevant to SDGs and that are in the public interest.
This is also the time for us as Nigerians, and as Africans, to open our eyes and realise the importance of improving individuals' social and economic rights – especially the poor and vulnerable – such as clean water and sanitation (SDG 6) and economic growth tied to decent work (SDG 8). It is clear that fighting COVID-19 requires people to have clean water and sanitation – and not everyone has access to it.
Much of our nation’s willingness to learn, embrace and engage with the plethora of ongoing initiatives that have so positively contributed to the building and delivery of timely, appropriate and affordable care concepts and pathways in Nigeria today, is arguably attributable to the overarching and consistent primary theme of ‘accessibility’ these tremendous efforts were primarily built upon. A fearlessly competent, responsible and promising generation have successfully ensured that accessibility remains a true ethos and the pertinent undercurrent when shaping and delivering an intentional and undeniably imperative standard of care. Sadly, their efforts have now rather tragically arrived at a potential point of trepidation.
These findings should fill every stakeholder with encouraging zeal, renewed passion and an inexplicable sense of determination to work towards establishing tangible, long-term solutions for this pandemic and beyond. We must continue forward – and ensure that a path towards the sustainable replenishment of much needed resources is assured.
To date, the responses and levels of engagement from members of society coupled with repeated statistical confirmations of increased success following the introduction of a number of health and wellbeing initiatives, further echoes my sentiments and of many others. Now more than ever before, the nation requires a firm continuation of a well-functioning, culturally and economically appropriate primary health and basic education system – one which must remain accessible to all and for all, in all its entirety. With this being said then, the most poignant way of ensuring that this can and should be made possible, is to maintain the level of financial input that 9th NASS initially committed to and maintained in the lead up to this unfortunate outcome.
In light of the recent COVID-19 outbreak, and while duly and empathetically acknowledging the economical setbacks that such a global pandemic has birthed, it is with the greatest of respect, care, honour, but also pride for all that we as a nation have achieved, that I make mention of this decision being a very important one.
From our global counterparts and stakeholders, right through to a growing community of invested and daily-committed healthcare and education facilitators here in our nation of Nigeria, the transitions and great strides made and being reflected by way of national and international policy, practice and (societal) position are going from strength to strength. Many of you have responsibly embarked on a lifelong journey which has continuously proven to be of great societal, medical and generational benefit. This is particularly evident statistically.
With health, as with education, the access to upholding and maintaining it, and human engagement really do go hand in hand: the intentional attitude and efforts our nation employs daily in a bid to truly care, educate and continue advocating for a significantly positive quality of life for all, is in actual fact, entirely dependent on the resources being made available to professionals and those within their care.
Access to affordable healthcare and education then, should be a precise and continuous embodiment of the primary intention behind the service and its delivery. I believe that the truest way in which we can continue to facilitate, impact and inform attitudes and approaches to healthcare and education in our nation, in a way that evidently works well, is to truly uphold our level of (physical and financial) input. Only then, can we truly make it holistically accessible.
Last week, I signed my name to join the #GlobalGoalUnite call for urgent investments and actions.
Join me, by signing the campaign here, too: www.globalcitizen.org
As we herald the new commitments targeted at mitigating the disruptions of the Sars-Cov2 pandemic, in expectation of focused investments we are reminded then, that the initiation, solution and budgetary injection must primarily derive from the pots that sit within local parliaments, while recalling that in fact, in 2019, the Inter-Parliamentary Union did actively play its part in passing its historic first resolution towards universal health coverage, substantiating global approaches to recordkeeping.
Parliaments themselves should also intensify this co-operation and share their best practices, experiences and challenges in dealing with the COVID-19. International organisations such as the OECD and its Global Parliamentary Network have a pivotal role to play during these unprecedented times. They help to facilitate pertinent policy dialogues on important socio-economic matters and provide us with advice and recommendations, so that parliaments can use them as guidelines to improve the situation and/or propose to its governments.
To use the example of the Indonesian Parliament view that the implementation and achievement of the Sustainable Development Goals (SDGs) cannot be postponed amid the COVID-19 pandemic, I restate the fact that the SDGs should be the measure for parliaments to prevent trade-offs in this moment of crisis, for example, between the economy and health, in any laws or programmes. It is also important to emphasise that the entire Indonesian House of Representatives, including those in the commissions, are working to support the implementation and achievement of the SDGs, supporting resolutions relevant to SDGs and that are in the public interest.
This is also the time for us as Nigerians, and as Africans, to open our eyes and realise the importance of improving individuals' social and economic rights – especially the poor and vulnerable – such as clean water and sanitation (SDG 6) and economic growth tied to decent work (SDG 8). It is clear that fighting COVID-19 requires people to have clean water and sanitation – and not everyone has access to it.
Much of our nation’s willingness to learn, embrace and engage with the plethora of ongoing initiatives that have so positively contributed to the building and delivery of timely, appropriate and affordable care concepts and pathways in Nigeria today, is arguably attributable to the overarching and consistent primary theme of ‘accessibility’ these tremendous efforts were primarily built upon. A fearlessly competent, responsible and promising generation have successfully ensured that accessibility remains a true ethos and the pertinent undercurrent when shaping and delivering an intentional and undeniably imperative standard of care. Sadly, their efforts have now rather tragically arrived at a potential point of trepidation.
These findings should fill every stakeholder with encouraging zeal, renewed passion and an inexplicable sense of determination to work towards establishing tangible, long-term solutions for this pandemic and beyond. We must continue forward – and ensure that a path towards the sustainable replenishment of much needed resources is assured.
To date, the responses and levels of engagement from members of society coupled with repeated statistical confirmations of increased success following the introduction of a number of health and wellbeing initiatives, further echoes my sentiments and of many others. Now more than ever before, the nation requires a firm continuation of a well-functioning, culturally and economically appropriate primary health and basic education system – one which must remain accessible to all and for all, in all its entirety. With this being said then, the most poignant way of ensuring that this can and should be made possible, is to maintain the level of financial input that 9th NASS initially committed to and maintained in the lead up to this unfortunate outcome.
In light of the recent COVID-19 outbreak, and while duly and empathetically acknowledging the economical setbacks that such a global pandemic has birthed, it is with the greatest of respect, care, honour, but also pride for all that we as a nation have achieved, that I make mention of this decision being a very important one.
From our global counterparts and stakeholders, right through to a growing community of invested and daily-committed healthcare and education facilitators here in our nation of Nigeria, the transitions and great strides made and being reflected by way of national and international policy, practice and (societal) position are going from strength to strength. Many of you have responsibly embarked on a lifelong journey which has continuously proven to be of great societal, medical and generational benefit. This is particularly evident statistically.
With health, as with education, the access to upholding and maintaining it, and human engagement really do go hand in hand: the intentional attitude and efforts our nation employs daily in a bid to truly care, educate and continue advocating for a significantly positive quality of life for all, is in actual fact, entirely dependent on the resources being made available to professionals and those within their care.
Access to affordable healthcare and education then, should be a precise and continuous embodiment of the primary intention behind the service and its delivery. I believe that the truest way in which we can continue to facilitate, impact and inform attitudes and approaches to healthcare and education in our nation, in a way that evidently works well, is to truly uphold our level of (physical and financial) input. Only then, can we truly make it holistically accessible.
Last week, I signed my name to join the #GlobalGoalUnite call for urgent investments and actions.
Join me, by signing the campaign here, too: www.globalcitizen.org
FROM June 20th, 2020
There are more displaced peoples in Nigeria—over two million—than the populations of Ilorin, Abuja and even Benin City. The scale of this situation in Nigeria is a tragedy for our people and our economy. At home in Nigeria, the conditions being faced by our population of concern are an increased cause for alarm and focused action within our COVID-19 response strategies – Nigeria is facing immense humanitarian and protection challenges due to the ongoing insurgency in the North East. The conflict has caused grave human rights violations, impacting particularly on the most vulnerable civilians. According to the UNHCR, as of May 2020, there are 2,046,604 internally displaced persons in the Northeast region, with 90% of the displacements in Borno, Adamawa and Yobe states. Outside of the Northeast an estimated 578,119 people are displaced due to banditry and farmer-herders conflict. There are 61,361 registered refugees and asylum seekers as of April 2020, with 60% located in Cross Rivers, 21% in Taraba, 12% in Benue and 6% registered in Lagos whom are classified as urban refugees and asylum seekers. There are a further 292,513 Nigerian Refugees in our neighbouring countries of Niger (55%), Cameroon (40%), and Chad (5%). View the map>> In summary, as of May this year, the total number of people attributed to Nigeria’s existing population of concern stood at 2,107,965. More than 61,000 were registered as refugees and asylum seekers, and the significant remainder originating from neighbouring nations were identified as internally displaced persons (IDP). The spectrum of challenges that refugees and displaced persons face is very broad: they may be traumatised, having lost homes, livelihoods and identities. However, when the host communities have strong systems in place, the suffering is mitigated, and the road to recovery can begin. I have always felt that refugees should have health rights guaranteed in any host location, and health-enhanced certifiable identities. The United Kingdom, Greece and Turkey support the health of refugees effectively, with the help of the World Health Organisation, which works closely with government health departments to provide culturally and linguistically sensitive health services to refugees. That’s why in February I was pleased to attend the launch of the Lancet Migration, a collaboration of researchers in migration and health who are building evidence to drive policy change in this area. I’ve been involved with helping to provide aid to many refugee camps in Northern Nigeria, and I’ve come to the understanding that ensuring health care should be standard in supporting the dignity of displaced persona. On World Refugee Day today, I commit to working with Lancet Migration, and call for attention on the rights of refugees in relation to accessibility to health care.
FROM June 1st, 2020
This year marked the start of the United Nations' Decade of Delivery, where we were promised that things would change for the empowerment of women and girls. Armed with research to prove how much better off our world would be with the rights of women and girls realised, we in the global advocacy community declared that it is well past time to start living in a gender equal reality.
FROM May 29th, 2020
The recent stories about violent police killings of African Americans are pulling at my heartstrings. My expertise is in child and maternal health and wellbeing in Africa, and police brutality in the United States may seem like it is 6,218 miles (the distance from Lagos to Minneapolis) away from my wheelhouse. But that would be denying the reality that we Africans are a global community united by the colour of our skin and ancestries that have been altered by systems of oppression that have spanned and scrambled our societies for generations, and which we have, collectively and individually, climbed to overcome.
FROM May 26th, 2020
As we mark Africa Day, I am encouraged by the milestones we have achieved, standing together as one united Africa, towards providing equity in health access since the Alma Ata declaration of 1978. Personally, a high point for Nigeria was in 2018 when Nigeria's National Assembly, chaired by my husband H.E. Dr Bukola Saraki MBBS, CON, helped establish the Basic Health Care Provision Fund. It was a key and catalytic step towards achieving Universal Health Coverage for our citizens. As the coronavirus pandemic puts health systems to unprecedented tests, I call on our African leaders, of governments, of policies, and of innovative actions, to rise to the challenge of the #AfricaWeWant. We must accelerate investments and actions to meet the health needs of our citizens by strengthening primary health care services with efficient diagnostics, referrals and treatment. Let's walk the talk for primary health care and wellbeing. As we stand together in rallying the right resources to combat COVID-19, I also call for the reinforcement and replenishment of the 2001 Abuja Declaration—a pledge made by the African Union, standing as one, promising to increase their health budget to at least 15% of the state's annual budget. The World Health Organisation reported in 2010 that only one African country had reached that target. Today in 2020, we must replenish and reinforce those promises to ensure that every citizen can access an efficient system of quality health.
FROM May 20th, 2020
During a normal year I would be traveling to the World Health Assembly this week, but this year I joined state leaders and world-renowned experts virtually from our homes, in light of the COVID-19 pandemic. Still, the spirit is evident: global collaboration on the state of our world’s health has never in our lifetime been more necessary.
FROM May 8th, 2020
I am excited to announce that Wellbeing Foundation Africa is partnering with U.S.-based company Fortify to address iron deficiency: the major underlying cause of maternal deaths during childbirth in developing countries. I started working on improving iron deficiency in Nigeria in 2014 with a programme called Green Food Steps. I worked with Unilever’s biggest brand Knorr to educate women and daughters to practice new, nutritious cooking habits. But when I met the Fortify team to talk about a partnership last year, I was struck by how elegant yet practical a solution they have for iron deficiency anemia: they help add iron to ingredients that make up everyday meals—such as tomato paste. Tomato paste is already built into the food supply, it’s a big part of the meals every African eats; that’s why they’ve worked to produce 20 million sachets of iron-fortified tomato paste varieties in Nigeria monthly. Implementing more iron in our food staples is not just a compassionate move to improve maternal health: it’s economically beneficial, too. According to the World Health Organization, timely treatment of iron deficiency anemia can ultimately raise national productivity levels by as much as 20%. That’s why I’m so excited to engage First Ladies and women leaders—because of the impact they bring to women, families and communities in improving maternal health outcomes—but also policymakers across Africa to accelerate efforts to eradicate iron deficiency. Read more on Wellbeing Africa.
FROM May 4th, 2020
FROM April 28th, 2020
Together, we are facing a global health crisis. Each day, as the death toll due to COVID-19 rises, people in governments, institutions, hospitals, communities and households around the world are having to navigate unprecedented sacrifice and hardship – making decisions with profound effects on their lives and livelihoods. As a collective network of girls, women, advocates, and allies working in global development, we stand together to encourage global collaboration to combat COVID-19. Only by working together can we ensure that no one is left behind in our response to the pandemic. Our focus now must be on supporting vulnerable communities and the most vulnerable people within our communities – in the spirit of solidarity, but also for our own protection. This includes girls and women who are now at a higher risk of gender-based violence and rights abuses, and at-risk groups (including people who have disabilities or identify as LGBTQIA) who are being targeted or are unable to access routine services. At a time of ever-increasing social distancing, there has never been a more crucial need for community and selfless leadership. The World Health Organization’s continued focus on saving lives and supporting and protecting the most vulnerable of us will play a pivotal role in our recovery. Now more than ever, countries need to unite behind a strong WHO – sharing knowledge, strategy, technical resources and financial investment to defeat the global threat we all face. We must make no concessions for blame, politicisation or racism in developing an inclusive and effective solution to this crisis. Across the world, we see the power of community and shared resources, as individuals step forward to support each other. Our heroes – the predominantly-female health workforce, working day and night to serve our communities and unite us – have demonstrated that cooperation is to mitigate the impact of COVID-19. In such challenging times, it is crucial that we overcome any efforts to divide us. Join us by signing on
FROM April 15th, 2020
 UN Secretary-General Antonio Guterres at a press briefing on the eve of an International Conference on the future of 4.6 million Afghan refugees living in Pakistan—in Islamabad on February 16, 2020. REUTERS/Saiyna Bashir[/caption]
UN Secretary-General Antonio Guterres at a press briefing on the eve of an International Conference on the future of 4.6 million Afghan refugees living in Pakistan—in Islamabad on February 16, 2020. REUTERS/Saiyna Bashir[/caption]
‘Countries with strong national health systems and universal health coverage are better able to cope with outbreaks and other health emergencies’
 Afghan parliamentary candidate Suhaila Sahar during an election campaign in Kabul on October 8, 2018. Research suggests female parliamentarians are more likely to give greater priority to health. REUTERS/Omar Sobhani[/caption]
NUMBER FOUR: Women and men have different, socially defined roles—and this perpetuates inequalities and weakens health security. Women carry out the majority of care for sick family and community members, and that puts women at greater risk of contracting infections like COVID-19. At the same time, women’s role as household caregivers can be leveraged for better health promotion and disease prevention/management at the family and community levels—but only if they are empowered with accurate information and the means to support the sick. COVID-19 was initially associated with a particular food market in Wuhan, China, where it is likely that the majority of traders were women. After the SARS outbreak in China in 2002, women in the same professions could have been vital allies in the cultural and behavioral change needed to avert a new viral outbreak—but clearly, this opportunity was missed. In many country contexts women are less educated than men, have less access to digital technology, and are generally overlooked as potential change agents.
NUMBER FIVE: Biology and gender determinants of health affect the way disease is transmitted and progresses. Data are still being collected and analysed, but early figures from the COVID-19 outbreak in China show higher mortality among men than women, especially in older age groups.
Afghan parliamentary candidate Suhaila Sahar during an election campaign in Kabul on October 8, 2018. Research suggests female parliamentarians are more likely to give greater priority to health. REUTERS/Omar Sobhani[/caption]
NUMBER FOUR: Women and men have different, socially defined roles—and this perpetuates inequalities and weakens health security. Women carry out the majority of care for sick family and community members, and that puts women at greater risk of contracting infections like COVID-19. At the same time, women’s role as household caregivers can be leveraged for better health promotion and disease prevention/management at the family and community levels—but only if they are empowered with accurate information and the means to support the sick. COVID-19 was initially associated with a particular food market in Wuhan, China, where it is likely that the majority of traders were women. After the SARS outbreak in China in 2002, women in the same professions could have been vital allies in the cultural and behavioral change needed to avert a new viral outbreak—but clearly, this opportunity was missed. In many country contexts women are less educated than men, have less access to digital technology, and are generally overlooked as potential change agents.
NUMBER FIVE: Biology and gender determinants of health affect the way disease is transmitted and progresses. Data are still being collected and analysed, but early figures from the COVID-19 outbreak in China show higher mortality among men than women, especially in older age groups.
‘Early figures from the COVID-19 outbreak in China show higher mortality among men than women, especially in older age groups’One hypothesis is that higher smoking rates by men leaves them more susceptible to respiratory viruses like SARS-CoV-2, which causes COVID-19. There are other gender-related aspects of the disease that are virtually unknown—for example, we still need to understand how COVID-19 affects pregnant and breastfeeding women in order to protect both women and the unborn child. A different virus, Zika, if contracted by a pregnant woman, does serious harm to the unborn child. Nothing similar has been reported with COVID-19, but this example show that it is critical that policy responses to epidemics examine the impact of both biological sex and the gender determinants of health. [caption id="attachment_1087" align="aligncenter" width="640"]
 A man wearing an N95 mask smokes in Singapore on February 23, 2020. Higher smoking rates among men may leave them more susceptible to respiratory viruses and account for higher COVID-19 mortality. REUTERS/Feline Lim[/caption]
A man wearing an N95 mask smokes in Singapore on February 23, 2020. Higher smoking rates among men may leave them more susceptible to respiratory viruses and account for higher COVID-19 mortality. REUTERS/Feline Lim[/caption]
NUMBER SIX: Global health rests on the foundation of women’s unpaid work. Here’s an uncomfortable fact: women in health contribute an estimated 5 percent to global GDP ($3 trillion), of which almost 50 percent is unrecognised and unpaid. Some of the world’s poorest women and girls are effectively subsidising health systems and missing out on opportunities to enter education and the formal labor market. This is not only inequitable—it weakens global health security everywhere. Infectious diseases like COVID-19 do not respect national borders, and we are all only as safe as people in the weakest national health system. Women’s unpaid work needs to be recorded, redistributed (within the family and community) and rewarded, with women enabled to transition into paid formal sector employment.
‘We cannot fight a global health challenge like this by drawing from just half the talent pool’
FROM April 15th, 2020
The world is hurting, and we need the WHO now more than ever before. Millions are suffering and misinformation is spreading, with fear and even racism impeding mechanisms for an effective response. Countries and communities are acting both together and apart. Right now, every community needs information based strictly in science and supported with the benefit of a global perspective. The world needs a well-functioning global organization designed to facilitate international coordination. We need the WHO, our standard-bearer in unprecedented times for an unprecedented virus. The pandemic is a stark reminder that humans are connected, and that what happens in one country can impact the everyday lives, social fabrics and economies of countries far away. Human connectivity holds power: the positive impact of our collective will to physically distance from one another alone shows what power we hold. Guided by the heart beat of world health—the WHO—together we have pulled resources, research, and we have made a global effort to benefit the health of all of us. We are grateful for those who have recovered due to the efforts of indefatigable health workers who have detected, tracked, traced and treated the affected, even as we have mourned the lives and livelihoods that we have lost. Together we must continue to marshal support to combat this virus. We hold the hope for better days ahead.
FROM March 25th, 2020
World Tuberculosis Day 2020 – It Is Crucial To Deepen TB Advocacy And Actions To Ensure Tuberculosis Does Not Become Totally Invisible During The COVID-19 Pandemic – Toyin Saraki, Founder, Wellbeing Foundation Africa I was recently following the research findings of Madhukar Pai, Canada Research Chair of Epidemiology and Global Health at McGill University, Montreal Canada, where he called for a damage control plan for tuberculosis during the ongoing COVID-19 Pandemic. As the coronavirus COVID-19 pandemic sweeps the world, the global health community working to fight TB have growing anxiety about what this pandemic will do to a much older infectious killer - tuberculosis (TB). We know from the Ebola experience that epidemics can disrupt even basic services such as routine immunization. No doubt, COVID-19 will adversely affect all routine health services everywhere. But TB services is might be one of the biggest casualties. Why? Even before COVID-19, TB had a notorious track record as a ‘Captain of the Men of Death’. TB kills 4000 people each day, and 1.5 million people each year. TB is the leading killer of people living with HIV/AIDS. An estimated 10 million people developed TB in 2018, and nearly half a million people developed drug-resistant TB (DR-TB). COVID-19 is a crisis of social solidarity and social investment. This applies to TB as well. It is crucial to deepen TB advocacy and actions to make sure TB does not become completely invisible during the COVID-19 pandemic. People are leaving no stone unturned to stop the coronavirus pandemic. If we show even half of this dedication towards ending TB, we can stop millions from dying from a preventable and curable disease. I stand in solidarity with the Stop TB community as we support people affected by COVID-19. This World TB Day we support the fight against the new pandemic, share our lessons, experiences and tools so that united we can defeat it. We want to remind global leaders the urgency to invest in better and more resilient health systems, today more than ever we realise the need to end endemics like TB or COVID-19. To fight COVID19, we can use the tools needed to End TB: infection control, artificial intelligence, x-rays, contact tracing, telemedicine and psycho-social support. Years of under-investment made tuberculosis and its drug resistant forms the biggest infectious disease killer with over 4000 deaths per day. We can’t afford to repeat these mistakes and be unprepared for pandemics like COVID19. Most TB survivors have gone through the isolation, fear, discrimination and stigma that we are facing with COVID 19. Let’s hear their voices and learn resilience from them. It’s Time To End TB. It’s time to recognize that people with #TB are vulnerable to COVID19, including prisoners, migrants, people living with #HIV, and those who are malnourished. Healthcare workers are at the centre of the fight against diseases such as tuberculosis or COVID-19 - While most of us are at home, social distancing, the health workers leave their houses and families to ensure that people with TB get diagnosed, treated and cured and also battle COVID-19. I appreciate and applaud their efforts as frontline health heroes. I join the Stop TB Partnership in calling on global leaders to join forces to protect people affected by TB and especially vulnerable populations from #COVID19. It’s time to ensure we #LeaveNoOneBehind #ItsTimeToEndTB
FROM February 9th, 2020
Along with the global health community, The Wellbeing Foundation Africa has taken note of the WHO declaration of a public health emergency of international concern over the global outbreak of the Novel Coronavirus.
WHO has identified 13 top priority countries (Algeria, Angola, Cote d’Ivoire, the Democratic Republic of the Congo, Ethiopia, Ghana, Kenya, Mauritius, Nigeria, South Africa, Tanzania, Uganda, and Zambia) which either have direct links or a high volume of travel to China.
“To ensure rapid detection of the novel coronavirus, it is important to have laboratories which can test samples and WHO is supporting countries to improve their testing capacity. Since this is a new virus, there are currently only two referral laboratories in the African region which have the reagents needed to conduct such tests."
“However, reagent kits are being shipped to more than 20 other countries in the region, so diagnostic capacity is expected to increase over the coming days. Active screening at airports has been established in a majority of these countries and while they will be WHO first areas of focus, the organization will support all countries in the region in their preparation efforts"
"It is critical that countries step up their readiness and in particular put in place effective screening mechanisms at airports and other major points of entry to ensure that the first cases are detected quickly”
The Wellbeing Foundation Africa commends and thanks the thousands of courageous frontline heroes, the frontline health professionals who are working around the clock in affected regions to treat the sick, save lives and bring this outbreak under control. The Wellbeing Foundation Africa continues to advocate and urge, particularly in Nigeria which is currently responding to a Lassa Fever outbreak in over 11 states, that investment in a skilled and sustainable, locally led frontline health workforce able to detect, report and respond to threats and deliver quality health services including water, sanitation and hygiene essentials for infection prevention and control, is crucial to building health systems resilient to outbreak.